What does PR 96 mean on a medical bill?
What does PR 96 mean? Whenever claim denied as CO 96 – Non Covered Charges it may be because of following reasons: Diagnosis or service (CPT) performed or billed are not covered based on the LCD. Services not covered due to patient current benefit plan. Click to see full answer.
What is the reason code for Medicare Part 96?
Reason Code 96: Medicare Secondary Payer Adjustment Amount. Reason Code 97: Payment made to patient/insured/responsible party/employer. Reason Code 98: Predetermination: anticipated payment upon completion of services or claim adjudication.
Can We Bill a patient with a remark code of PR?
At least one Remark Code must be provided (may be comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.) What we can do – See the additional remark code for exact reason and act accordingly. What we can do – PR – stands for Patient responsibility. Hence we can bill the patient.
What is a non-covered charge PR 96?
CO/PR 96 Non-covered charge(s) (THE PROCEDURE CODE SUBMITTED IS A NON-COVERED MEDICARE SERVICE) Resources/tips for avoiding this denial. There are multiple resources available to verify if services are covered by Medicare we can use that resources.
What is Medicare Reason code 96?
Transportation to/from this destination is not covered. Ambulance services to or from a doctor's office are not covered.
What does PR mean on an EOB?
PR = Patient Responsibility. Note: The Group, Reason and Remark Codes are HIPAA EOB codes and are cross-walked to L&I's EOB codes.
What does PR mean in medical billing?
Patient ResponsibilityPR (Patient Responsibility) is used to identify portions of the bill that are the responsibility of the patient. These could include deductibles, copays, coinsurance amounts along with certain denials.
What is reason code PR?
PR – Patient Responsibility denial code list. MCR – 835 Denial Code List. PR – Patient Responsibility – We could bill the patient for this denial however please make sure that any other rejection reason not specified in the EOB. Same denial code can be adjustment as well as patient responsibility.
What is group code PR?
What does the denial code PR mean? PR Meaning: Patient Responsibility (patient is financially liable). A provider is prohibited from billing a Medicare beneficiary for any adjustment amount identified with a CO group code, but may bill a beneficiary for an adjustment amount identified with a PR group code.
What is pr2 on EOB?
PR-2 indicates amount applied to patient co-insurance.
What does PR 100 mean?
Non-Par Medicare claims (PR-100)
What is the PR code for deductible?
Claim Adjustment Reason CodesCOContractual ObligationCRCorrections and Reversal Note: This value is not to be used with 005010 and up.OAOther AdjustmentPIPayer Initiated ReductionsPRPatient Responsibility
What is a PR in nursing?
PR apparently stands for "practical nurse."
What is the denial code 96 mean?
96 Non-covered charge(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.)
What does PR 3 mean on an EOB?
Description: Copayment A specified dollar amount or percentage of the charge identified that is paid by a beneficiary at the time of service to a health care plan, physician, hospital, or other provider of care for covered service provided to the beneficiary.
What is PR 59 denial code?
Reason Code 59: Payment denied/reduced for absence of, or exceeded, pre-certification/authorization. Reason Code 60: Correction to a prior claim. Reason Code 61: Denial reversed per Medical Review.
What is PR 49?
Medicare Denial reason pr 49. These are non-covered services because this is a routine exam or screening procedure done in conjunction with a routine exam. What we can do – PR – stands for Patient responsibility. Hence we can bill the patient. However check your CPT and DX before bill the patient.
What is MA130 claim?
MA130 Your claim contains incomplete and/or invalid information, and no appeal rights are afforded because the claim is unprocessable. Please submit a new claim with the complete/correct information. What we can do – This is the general denial and see addition code for exact denial.
What is the reason code for a procedure?
Reason Code 1: The procedure code is inconsistent with the modifier used or a required modifier is missing. Reason Code 2: The procedure code/bill type is inconsistent with the place of service. Reason Code 3: The procedure/ revenue code is inconsistent with the patient's age.
What is the reason code for 177?
Reason Code 177: Patient has not met the required residency requirements. Reason Code 178: Procedure code was invalid on the date of service. Reason Code 179: Procedure modifier was invalid on the date of service. Reason Code 180: The referring provider is not eligible to refer the service billed.
Common Reasons for Denial
Non-covered charge (s). Medicare does not pay for this service/equipment/drug.
Next Step
If billed incorrectly (such as inadvertently omitting a required modifier), request a reopening. Utilize the Noridian Modifier Lookup Tool to ensure proper modifiers are included on claim
How to Avoid Future Denials
Review applicable Local Coverage Determination (LCD), LCD Policy Article documentation requirements for coverage and use of modifiers. Utilize the Noridian Modifier Lookup Tool to ensure proper modifiers are included on claim, prior to billing.
What is an EOB?
An EOB is a summary page showing how much money your insurance plan paid and how much money you must pay (if any) for a health service you got, like a doctor visit or lab test. Every time you get a health service, you’ll get an EOB from your insurance company in the mail or by email. An EOB is not a bill.
Why do you check your EOB?
Check your EOB to make sure you got the health services it shows you got. It might list more than one health service and provider. For example, if your doctor did a blood test during your visit, your EOB might list the doctor visit and the blood test as separate charges.
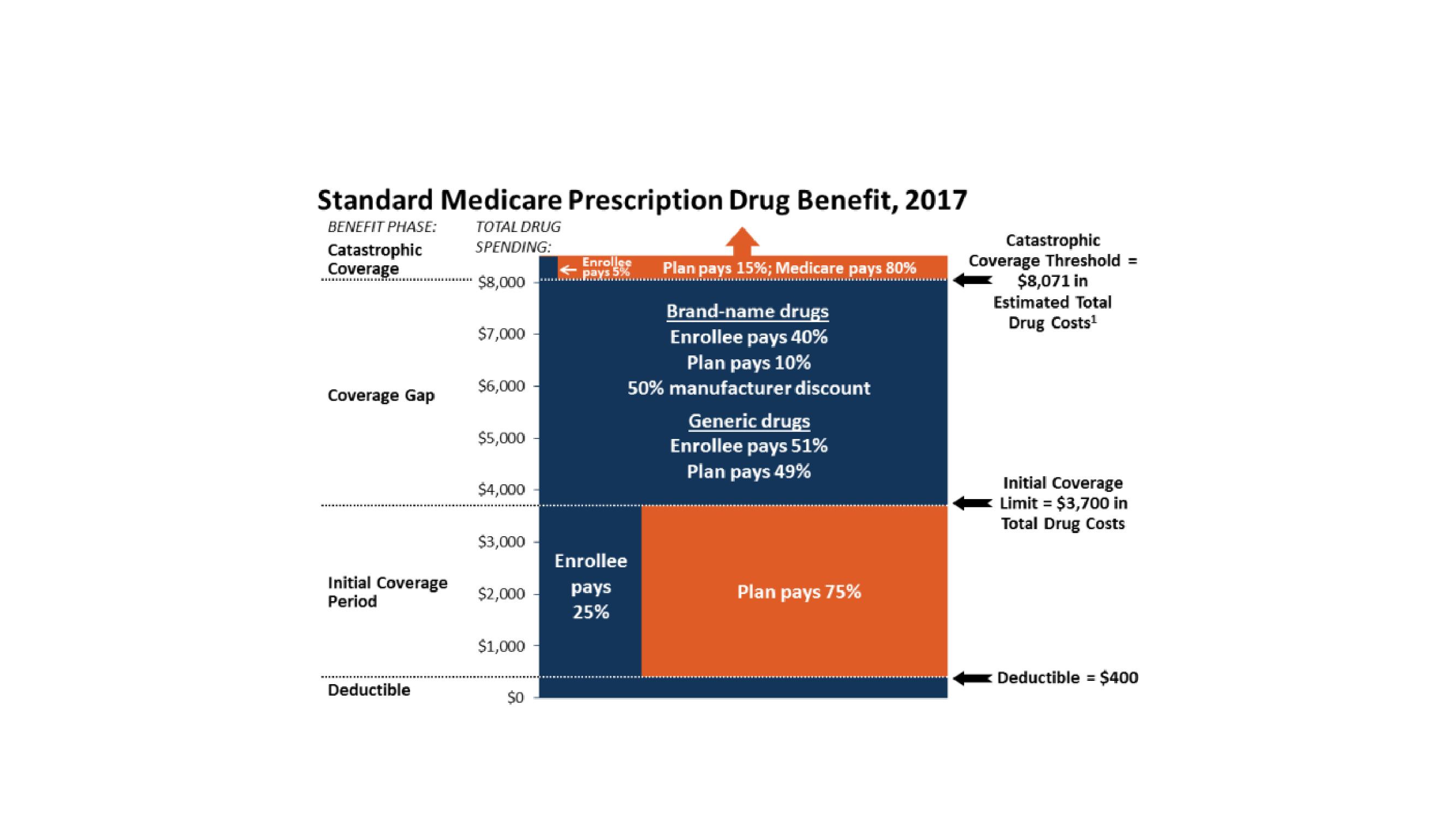
What is PR group code?
A PR group code signifies the amount that may be billed to the beneficiary or to another payer on the beneficiary’s behalf. For example, PR would be used with the reason code for patient deductible or coinsurance, if the patient assumed financial responsibility for a service not considered reasonable and necessary, for the cost of therapy or psychiatric services after the coverage limit had been reached, for a charge denied as result of the patient’s failure to supply primary payer or other information, or where a patient is responsible for payment of excess non-assigned physician charges. Charges that have not been paid by Medicare and/or are not included in a PR group, such as a late filing penalty (reason code B4), excess charges on an assigned claim (reason code 42), excess charges attributable to rebundled services (reason code B15), charges denied as result of the failure to submit necessary information by a provider who accepts assignment, or services that are not reasonable and necessary for care (reason code 50 or 57) for which there are no indemnification agreements are the liability of the provider. Providers may be subject to penalties if they bill a patient for charges not identified with the PR group code.