Does Medicare cover infusion drugs?
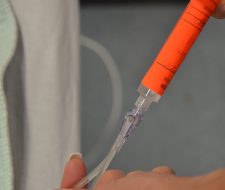
Injectable and infused drugs: Medicare covers most injectable and infused drugs when a licensed medical provider gives them, because these types of drugs aren't usually self-administered.
What does Medicare consider self-administered drugs?
“Self-administered drugs” are medications that you would normally take on your own, like medications that you take every day to control blood pressure or diabetes. In most cases, Part B generally doesn't pay for self-adminstered drugs used in the hospital outpatient setting.
Does Medicare cover Avastin injections?
The Centers for Medicare & Medicaid Services (CMS) established a national Medicare payment amount for Lucentis; however, there is no national Medicare payment amount for Avastin when used to treat wet AMD in a physician's-office setting.
Are infusions covered under Part B Medicare?
Medicare Part B covers drugs that are infused through durable medical equipment. That can include insulin when the use of an insulin pump is determined to be medically necessary.
Why does Medicare not cover self-administered drugs?
Medicare Part B covers outpatient hospital stays, but self-administered medications have very limited coverage.
Does Medicare Part D cover IV antibiotics at home?
But infusion treatments such as IV antibiotics, some cancer medications and hydration, may not be. The medicines are generally covered by Medicare Part D, but there is no coverage for the related professional services (i.e., home nursing), supplies, and equipment needed to safely administer the therapy in the home.
How much does an Avastin injection cost?
Avastin costs about $50 per injection. Lucentis costs about $2,000 per injection. Doctors choose the more expensive drug more than half a million times every year, a choice that costs the Medicare program, the largest single customer, an extra $1 billion or more annually.
What is the cost of Avastin?
The cost for Avastin intravenous solution (25 mg/mL) is around $849 for a supply of 4 milliliters, depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans.
What is Avastin prescribed for?
Avastin is used with chemotherapy and hits your cancer from another angle. Avastin is a tumor-starving (anti-angiogenic) therapy. The purpose of Avastin is to prevent the growth of new blood vessels. This includes normal blood vessels and blood vessels that feed tumors.
Does Medicare pay for IVIG treatment?
Currently, Medicare pays for IVIG medications for beneficiaries who have primary immune deficiency who wish to receive the drug at home.
What drugs are not covered by Medicare?
Medicare does not cover:Drugs used to treat anorexia, weight loss, or weight gain. ... Fertility drugs.Drugs used for cosmetic purposes or hair growth. ... Drugs that are only for the relief of cold or cough symptoms.Drugs used to treat erectile dysfunction.More items...
Is a PICC line covered by Medicare?
Medicare will cover home infusion therapy equipment and supplies when they are used in your home, but you will still be responsible for a portion of the cost. The equipment and supplies are considered durable medical equipment, which is covered by Medicare Part B.
How do I bill Avastin injection?
Coding guidance Providers should bill HCPCS code J7999, which is a not otherwise classified (NOC) code, for the compounded form of Avastin administered through an intravitreal injection. Providers should bill CPT code 67028 for the intravitreal injections, in addition to the drug(s) utilized.
How Much Does Medicare pay for Eylea injections?
Does Medicare Cover Eylea Injections? Eylea is the brand name for the drug; also, it's an injection to treat wet age-related macular degeneration. If your doctor determines treatment with Eylea is necessary, Part B will cover it. After you have met your Part B deductible, you pay 20% of the cost of the injections.
How is Avastin supplied?
Injection: 100 mg/4 mL (25 mg/mL) or 400 mg/16 mL (25 mg/mL) clear to slightly opalescent, colorless to pale brown solution in a single-dose vial. None. Serious, and sometimes fatal, gastrointestinal perforation occurred at a higher incidence in patients receiving Avastin compared to patients receiving chemotherapy.
What is the average cost of Eylea per injection?
Eylea will run $1,850 per dose, Bloomberg reports, compared with $2,000 for Lucentis, and $16,000 for a full year, compared with $24,000 for the Roche drug.