If your network doctors leave your Medicare Advantage plan, and you want to switch plans, contact your local state health insurance program for help. You may have the right to switch to another Medicare Advantage plan or to traditional Medicare.
Can I Leave my Medicare plan mid-year if my doctor changes?
And there's good news for the roughly 22 million seniors who have Medicare Advantage plans, private alternatives to government-run Medicare: Those with these insurance policies can, under certain circumstances, leave their plans mid-year if their doctors do.
Can My Medicare Advantage plan Drop Me due to a condition?
If you currently have a Medicare Advantage plan, you might be concerned that a change in circumstances could cause the plan to drop you and leave you without coverage. The good news is that Medicare Advantage can’t drop you due to a health condition or disease.
Why do beneficiaries leave Medicare Advantage plans?
Beneficiaries ultimately leave their Medicare Advantage plans for a variety of reasons. You don't want to regret your choice because of a lack of benefits, network restrictions, or cost-sharing. Whether you go with Medicare, Medigap, or an Advantage plan, make sure to do your homework.
How do Medicare Advantage plans work?
for certain services like chemotherapy, dialysis, and skilled nursing facility care. Medicare Advantage Plans have a yearly limit on your out-of-pocket costs for medical services. Once you reach this limit, you’ll pay nothing for covered services. Each plan can have a different limit, and the limit can change each year.

What happens if you see a doctor outside of your network?
This means you'll be responsible for paying 100% of the cost of your out-of-network care. Keep in mind that this means 100% of what the provider bills since there is no network-negotiated rate with a provider who isn't in your health plan's network.
Does Medicare reimburse out of network?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Are you automatically disenrolled from a Medicare Advantage plan?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
What are the negatives to a Medicare Advantage plan?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
What does out-of-network reimbursement mean?
If you go out-of-network, your insurer may reimburse a small percentage of the total cost and you may be responsible for paying the balance out of your own pocket.
What payment rules apply when the patient sees an out-of-network physician?
B. What payment rules apply when the patient sees an out-of-network physician? The patient is responsible for a deductible of $250. After that deductible is met, the patient is responsible for 20% of the fee.
Can I switch from a Medicare Advantage plan back to Original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
In which situation may the Medicare Advantage MA organization decide to disenroll a member from an MA plan?
(A) The MA organization must disenroll an individual if the MA organization establishes, on the basis of evidence acceptable to CMS, that the individual is incarcerated and does not reside in the service area of the MA plan as specified at § 422.2 or when notified of the incarceration by CMS as specified in paragraph ( ...
Can I switch from Medicare Advantage to Medigap without underwriting?
For example, when you get a Medicare Advantage plan as soon as you're eligible for Medicare, and you're still within the first 12 months of having it, you can switch to Medigap without underwriting.
Who is the largest Medicare Advantage provider?
AARP/UnitedHealthcareAARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What is the highest rated Medicare Advantage plan?
According to MoneyGeek's scoring system, the top-rated Medicare Advantage plans are Blue Cross Blue Shield for preferred provider organizations and UnitedHealthcare for health maintenance organizations.
Can you change your Medicare Advantage plan anytime?
No, you can't switch Medicare Advantage plans whenever you want. But you do have options if you're unhappy with your plan. You can jump to another plan or drop your Medicare Advantage plan and change to original Medicare during certain times each year. You may be eligible to change plans at other times, too.
How many seniors have Medicare Advantage?
And there's good news for the roughly 22 million seniors who have Medicare Advantage plans, private alternatives to government-run Medicare: Those with these insurance policies can, under certain circumstances, leave their plans mid-year if their doctors do.
When is the open enrollment period for Medicare?
There also is the Medicare Advantage Open Enrollment Period which runs from Jan. 1 through March 31. This enrollment period, which began in 2019, allows you to switch Advantage plans or go back to original Medicare. You can switch plans during the Annual Open Enrollment period for Medicare, Oct. 15 to Dec. 7, as well. [.
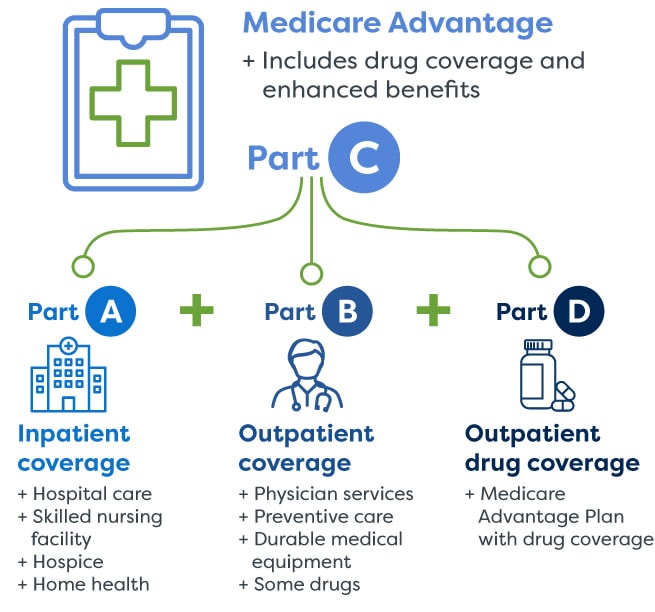
What is Medicare Advantage?
Many Medicare Advantage (MA) Plans (like HMOs or PPOs) have networks of health care providers which include doctors, other health care providers, hospitals, and facilities. It’s important to understand your plan’s provider network to make sure you get the care you need at the lowest cost.
Where do you get SNP care?
Generally, you must get your care and services from doctors, other health care providers, and hospitals in the SNP network (except emergency care, out-of-area urgent care, or out-of-area dialysis). SNPs typically have specialists in the diseases or conditions that affect their members.
Can you go out of network with an HMO?
In some plans, you may be able to go out-of-network for certain services, usually for a higher cost. This is called an HMO with a point-of-service (POS) option.
Why do people leave Medicare?
Other Potential Reasons Beneficiaries Leave Medicare Advantage Plans. While the reasons above are the most popular reasons people leave their plans, there may be other factors. Some other common reasons to leave Advantage coverage include: Your health care services may end up costing you quite a bit more. Some Medicare Advantage plans aren’t as ...
Is Part C coverage inclusive?
Most commonly, the policy isn’t as inclusive as they thought. When you look at the surface of a Part C policy, it seems simple enough—covering things like dental, vision, gym memberships, and more. But just because it covers the services, doesn’t mean that coverage is comprehensive. Usually, it’s better to buy a policy that covers you adequately. ...
Does Medicare cover dental?
Medicare doesn’t cover dental. But, some emergency jaw services may have coverage through Medicare. Often, Medicare Advantage plans are considered “ all-in-one ” plans because they include dental and vision coverage. But, your policy may only cover preventative services. With these limits, you could end up footing the bill for dental care ...
Can I see a doctor on Medicare Advantage?
Even with a Preferred Provider Organization plan, you’ll pay more to see doctors that aren’t in-network. But, Medigap beneficiaries can visit any physician that accepts Medicare. Although, if you don’t mind limitations to doctors and hospitals, an Advantage plan may work for you.
Is Medicare Advantage financially stable?
Some Medicare Advantage plans aren’t as financially stable and end coverage unexpectedly. Emergency care may be hard to come by. Some policies have strict rules to follow to get coverage. Health care while traveling can be hard to get. Plans that provide Part D coverage may limit specific high-cost prescriptions.
Why won't my Medicare Advantage plan drop me?
Loss of coverage. Eligibility. Special Needs Plans. Finding new coverage. Takeaway. A Medicare Advantage plan can’t drop you because of a health condition or disease. Your plan may drop you, though, if you fail to pay your premiums within a specified grace period. You might also lose your plan if it’s no longer offered by the insurance company, ...
When do you get a notice of change for Medicare Advantage?
Plan annual notice of change. If you have a Medicare Advantage plan, you will receive a letter each September that outlines any changes to your plan. The annual notice of change letter will come directly from your insurer, not from Medicare.
What is Medicare Advantage?
Medicare Advantage plans vary, but most include coverage for prescription drugs, as well as vision and dental care. Medicare Advantage plans are guaranteed issue. This means you’re guaranteed acceptance into the plan, provided you live in the plan’s service area and are eligible for original Medicare.
What happens if you miss Medicare open enrollment?
If you miss both your special enrollment window and open enrollment, your coverage will continue automatically through original Medicare. Because your Medicare Advantage plan will no longer be active, you won’t be able to enroll in a new Advantage plan during Medicare Advantage open enrollment.
What happens if you don't pay your Medicare premiums?
For example, if you don’t pay your premiums within the plan’s grace period for nonpayment, you can be dropped. Your plan can also drop you if it’ll no longer be offered in your area or through Medicare. Read on to learn more about why Medicare Advantage plans may end your coverage, how to find a new plan, and more.
What is a D SNP?
D-SNPs are designed to help individuals who have very low incomes and other issues receive optimum support and medical care.
When will Medicare Advantage be available for ESRD?
The new law allows individuals with ESRD to be eligible for Medicare Advantage plans, starting January 1, 2021. If you also qualify for an SNP, though, you might still prefer the coverage this type of plan provides.
