If you don’t, you’ll receive a termination notice informing you that you no longer have coverage. Now if you manage to pay what you owe in premiums within 30 days of that termination notice, you’ll get to continue receiving coverage under Part B. If you don’t do that, your coverage will be discontinued.
Full Answer
What does it mean if I don’t qualify for Medicare?
So strictly speaking, not having worked long enough to “qualify” means only that you can’t receive benefits for Medicare Part A (hospital insurance) without paying premiums for them.
Can you get Medicare if you don’t work?
But can you still get Medicare if you haven’t worked for that length of time during your life? The short answer is yes. You can get free Medicare Part A through your spouse or if you have certain medical conditions or disabilities. You can also choose to pay for Part A if you don’t qualify.
Is it possible to avoid Medicare?
While Medicare is not mandatory, it can be difficult to avoid it. If you refuse Medicare completely, you will not be allowed to receive Social Security payments.
What happens if I don’t sign up for Medicare when I’m 65?
What happens if I don’t sign up for Medicare when I’m 65? A. Joining Medicare is voluntary. But there may be consequences—in the form of a late penalty—if you don’t enroll at the “right” time, depending on your circumstances.

What happens if you don't qualify for Medicare Part A?
If you have to buy Part A, and you don't buy it when you're first eligible for Medicare, your monthly premium may go up 10%. You'll have to pay the higher premium for twice the number of years you didn't sign up.
Can you get Medicare if you don't qualify for Social Security?
Even if you don't qualify for Social Security, you can sign up for Medicare at 65 as long you are a U.S. citizen or lawful permanent resident.
Can you be denied for Medicare?
Medicare can deny coverage if a person has exhausted their benefits or if they do not cover the item or service. When Medicare denies coverage, they will send a denial letter. A person can appeal the decision, and the denial letter usually includes details on how to file an appeal.
How do you pay for Medicare Part B if you are not collecting Social Security?
If you have Medicare Part B but you are not receiving Social Security or Railroad Retirement Board benefits yet, you will get a bill called a “Notice of Medicare Premium Payment Due” (CMS-500). You will need to make arrangements to pay this bill every month.
How much does Medicare cost at age 62?
Reaching age 62 can affect your spouse's Medicare premiums He can still receive Medicare Part A, but he will have to pay a monthly premium for it. In 2020, the Medicare Part A premium can be as high as $458 per month.
What income is used to determine Medicare premiums?
modified adjusted gross incomeMedicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
How do you handle a denied Medicare claim?
If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
How long does it take to get approved for Medicare?
between 30-60 daysMedicare applications generally take between 30-60 days to obtain approval.
How far back does Social Security check your bank account?
Some of the things we do count are • Cash; • Your checking and savings accounts; • Christmas club accounts; • Certificates of deposit; and • Stocks and U.S. Savings Bonds. Any payments that you get from SSI or Social Security for past months won't be counted as a resource for nine months after the month you get them.
Do you automatically get Medicare with Social Security?
You automatically get Medicare because you're getting benefits from Social Security (or the Railroad Retirement Board). Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
What if I haven't worked long enough to qualify for Medicare?
So strictly speaking, not having worked long enough to “qualify” means only that you can’t receive benefits for Medicare Part A (hospital insurance) without paying premiums for them. ...
How many credits do you need to get Medicare?
Normally, you need to have earned about 40 “credits” or “quarters” by paying Social Security and Medicare payroll taxes while working — equal to about 10 years of work — in order to get Part A services without paying premiums. The premiums have already been covered by your payroll taxes.
What is Medicare Part B?
But you most likely qualify for Medicare Part B ( which covers doctors’ services, outpatient care and medical equipment) and for Part D (prescription drug coverage) because these have nothing to do with how long you’ve worked.
What happens if you decline Medicare?
Declining. Late enrollment penalties. Takeaway. If you do not want to use Medicare, you can opt out, but you may lose other benefits. People who decline Medicare coverage initially may have to pay a penalty if they decide to enroll in Medicare later. Medicare is a public health insurance program designed for individuals age 65 and over ...
What is Medicare Part A?
Medicare is a public health insurance program designed for individuals age 65 and over and people with disabilities. The program covers hospitalization and other medical costs at free or reduced rates. The hospitalization portion, Medicare Part A, usually begins automatically at age 65. Other Medicare benefits require you to enroll.
Is there a penalty for not signing up for Medicare Part B?
If you choose not to sign up for Medicare Part B when you first become eligible, you could face a penalty that will last much longer than the penalty for Part A.
Does Medicare Advantage have penalties?
Medicare Part C (Medicare Advantage) is optional and does not have penalties on its own, but penalties may be included for late enrollment in the parts of Medicare included within your Medicare Advantage plan.
Is Medicare mandatory at 65?
While Medicare isn’t necessarily mandatory, it is automatically offered in some situations, and may take some effort to opt out of.
Is Medicare Part D mandatory?
Medicare Part D is not a mandatory program, but there are still penalties for signing up late. If you don’t sign up for Medicare Part D during your initial enrollment period, you will pay a penalty amount of 1 percent of the national base beneficiary premium multiplied by the number of months that you went without Part D coverage.
What happens if I don't sign up for Medicare at 65?
What happens if I don’t sign up for Medicare when I’m 65? A. Joining Medicare is voluntary. But there may be consequences—in the form of a late penalty—if you don’t enroll at the “right” time, depending on your circumstances.
What happens if you delay a car insurance payment for 5 years?
For example, if you delay five years, you’ll pay an extra 50 percent of the cost of that year’s premium. The penalty amount grows larger over time because it’s pegged to the cost of each year’s Part B premiums, which generally rise every year.
What happens if you delay signing up for Part B?
You need to carefully consider your rights and options .) Part B (doctors and outpatient services): If you delay signing up for Part B beyond the time when you’re first eligible for it, you could incur a late penalty. (The exception is if you’re still working and have “primary” health insurance from your employer.)
Is there a penalty for not signing up for Part A?
Part A (hospital insurance) : There is no penalty for delaying to enroll in Part A if you qualify for it automatically on the basis of you or your spouse’s work record. But in most circumstances, there’s no reason not to sign up as soon as you’re eligible.
Do you have to pay a late penalty for prescription drugs?
There are exceptions. You would not risk a late penalty for as long as you have other insurance for prescription drugs (such as coverage under an employer health plan or retiree benefits) that is considered at least as good as Part D. If this is the case, you won’t need Part D unless you lose or drop such coverage.
What is the income limit for Medicare Part A?
The income limits are higher (up to $4,339/month for an individual, and $5,833 for a couple in 2020), but the asset limit is lower, at $4,000 for an individual and $6,000 for a couple.
What is extra help for Medicare?
Medicare offers “ Extra Help ” for Medicare enrollees who can’t afford their Part D prescription drug coverage. In 2020, if you’re a single person earning less than $1,615 per month ($2,175 for a couple), with financial resources that don’t exceed $14,610 ($29,160 for a couple), you may be eligible for “Extra Help.”.
Does Medicare cover long term care?
Medicare does not cover custodial long-term care, but Medicaid does, if the person has a low income and few assets. Almost two-thirds of the people living in American nursing homes are covered by Medicaid (almost all of them are also covered by Medicare).
Is Medicare a dual program?
Medicare-Medicaid dual eligibility. People who are eligible for MSPs are covered by Medicare, but receive assistance with premiums (and in some cases, cost-sharing) from the Medicaid program. But some low-income Medicare enrollees are eligible for full Medicaid benefits, in addition to Medicare. About 20 percent of Medicare beneficiaries are dually ...
How old do you have to be to get Medicare?
To apply, you must be 65 years old and a U.S. citizen or a lawfully admitted noncitizen who has lived in the United States for 5 years or more. If you buy Medicare Part A coverage, you must also enroll in Medicare Part B and pay those monthly premiums. The 2021 monthly premium for Part A coverage can be up to $471 per month. ...
When will I get Medicare if I have SSDI?
If you have a disability and have been receiving SSDI benefits for at least 24 months (2 years), you will automatically be enrolled in premium-free Medicare at the beginning of the 25th month.
How long do you have to be a working person to get Medicare Part B?
There’s no work history requirement to enroll in Medicare Part B. You can enroll as long as you’re at least 65 years old. Once you enroll in Medicare Part B, you will pay a monthly premium of $148.50 in 2021. Your premium may be more if your income is higher.
What is Medicare Advantage?
Medicare Advantage is a private insurance option that offers the same basic benefits as original Medicare (Part A and Part B), plus additional benefits like vision and dental care. You must be eligible for original Medicare to qualify for a Medicare Advantage plan.
How long does it take for Medicare to cover prescriptions?
While this plan is optional, Medicare requires you to have sufficient prescription drug coverage within 63 days of the date you become eligible for Medicare. This applies whether you get that coverage through Medicare, your employer, or another source.
How long does Medicare last?
Medicare is health insurance that’s provided through the U.S. government. It’s available once you turn 65 years old or if you: receive Social Security disability benefits for at least 2 years. receive disability pension benefits from the Railroad Retirement Board.
How many quarters can you work to get Medicare?
In general, Medicare is available premium-free if you’ve worked a total of 40 quarters (10 years or 40 work credits). But can you still get Medicare if you haven’t worked for ...
How many Americans are in the middle of the ACA?
Caught in the Middle: 2.3 Million Americans. The ACA provides tax credits (also called subsidies) for low-income people who purchase coverage on the exchanges. However, these tax credits only apply for those with incomes between 100 percent and 400 percent of the Federal Poverty Level.
When will the poverty level income numbers be released?
The 2021 figures, which may be slightly different, are expected to be published later in January 2021 in the Federal Register by the U.S. Department of Health and Human Services.
What is the ACA tax credit?
The ACA provides tax credits (also called subsidies) for low-income people who purchase coverage on the exchanges. However, these tax credits only apply for those with incomes between 100 percent and 400 percent of the Federal Poverty Level.
What is short term medical insurance?
Short-term medical insurance is a solution that many people are using to fill this gap. They may use it for a few months or for an extended period of time. It allows them to take comfort while getting lower-cost health insurance coverage for themselves and their families. Temporary health insurance for individuals who don’t qualify for Medicaid ...
Is Medicaid expansion optional?
Not all states agreed to the Medicaid expansion that was allowed through the ACA. Although the authors of the ACA expected the expansion to be national, a June 2012 ruling by the U.S. Supreme Court made the Medicaid expansion optional, at the choice of the states.
Is Obamacare an unaffordable plan?
There is not usually a lot left over for insurance premiums and out-of-pocket medical costs. That is why the Obamacare exchange—if you don’t qualify for tax credits—is usually an unaffordable option for low-income individuals and families. Even if a plan is available on the exchange for which you can afford the premiums (without a subsidy), ...
Is health insurance a low income expense?
For Americans with low income, health insurance is not often at the top of the list of expenses with which they are concerned. Food, housing, utilities, clothing and the immediate needs of their children come first. There is not usually a lot left over for insurance premiums and out-of-pocket medical costs. That is why the Obamacare exchange—if you ...
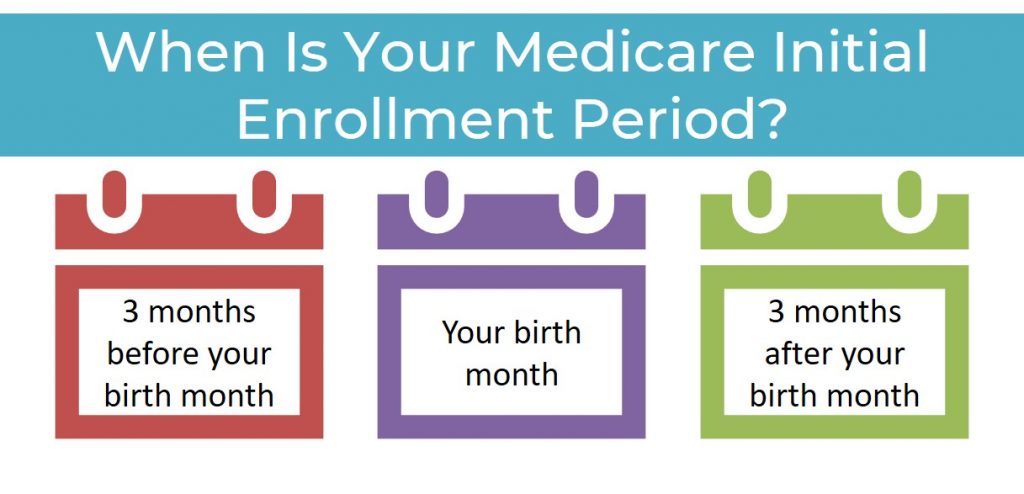
How far in advance can you start Medicare?
While active employment continues, you can specify the date on which you want Medicare coverage to begin, up to three months in advance. Otherwise, your coverage begins on the first day of the month after you enroll.
When is the Medicare enrollment period?
General Enrollment Period (GEP) If you miss the deadline for your IEP or SEP (or if you don’t qualify for a SEP), you can enroll in Medicare only during a general enrollment period, which runs from Jan. 1 to March 31 each year, with coverage not beginning until July 1 of the same year. If you need Medicare prescription drug coverage, ...
When is the open enrollment period for Medicare Part A?
Note: You cannot enroll in Medicare Part A or B for the first time during Medicare’s annual open enrollment period, which runs from Oct. 15 to Dec. 7 each year. This period is only for people already in Medicare who want to change their type of coverage for the following year.
