When an ESRD patient has existing GHP coverage, Medicare is the secondary payer of Medicare-covered services for a period of time known as the 30-month coordination period. The 30-month coordination period starts the first month you are eligible to get Medicare because of kidney failure (usually the fourth month of dialysis), even if you have not signed up for Medicare yet. At the end of the 30-month coordination period, Medicare will pay first for all Medicare-covered services. Check with your plan’s benefits administrator to see how your employer plan works with Medicare.
When does Medicare coverage based on ESRD end?
If the beneficiary has Medicare only because of ESRD, Medicare coverage will end when one of the following conditions is met: 36 months after the month the beneficiary had a kidney transplant. There is a separate 30-month coordination period each time the beneficiary enrolls in Medicare based on kidney failure.
How long is Medicare primary for ESRD?
Medicare becomes the primary payer of benefits after the 30-month coordination period ends, as long as the individual retains Medicare eligibility based on ESRD. A beneficiary may have more than one 30 - month coordination period.
Can you enroll in Medicare Advantage with ESRD?
If you have ESRD, you can enroll in a Medicare Advantage Plan during Open Enrollment (October 15 – December 7, 2020) for coverage starting January 1, 2021. When you decide how to get your Medicare coverage , you might choose Original Medicare or a Medicare Advantage Plan.
Does Medicare help with end-stage renal disease?
Medicare covers treatment for people with end-stage renal disease (ESRD) if you have permanent kidney failure requiring either dialysis or a kidney transplant. Medicare also covers the medical and hospital services it normally would that are necessary for your ESRD treatment.
What is ESRD?
How long does ESRD last?
What is ESRD in Medicare?
How much does Medicare pay for ESRD?
What causes kidney damage?
When will ESRD be available for Medicare?
When does Medicare start?
See more
About this website
Does Medicare cover those with end stage renal disease?
Medicare for those with End-Stage Renal Disease (ESRD Medicare) provides you with health coverage if you have permanent kidney failure that requires dialysis or a kidney transplant. ESRD Medicare covers a range of services to treat kidney failure.
Do I have to enroll in Medicare if I have ESRD?
If you have job-based insurance, retiree coverage, or COBRA when you become eligible for Medicare because you have End-Stage Renal Disease (ESRD Medicare), you do not have to enroll in Medicare right away.
How much is ESRD Medicare?
In inflation-unadjusted terms, total expenditures in Medicare FFS beneficiaries with ESRD increased from $28.0B in 2009 to $36.6B in 2018, or 30.7% (Figure 9.8).
How Long Does Medicare pay for dialysis?
When Medicare coverage ends. If you're only eligible for Medicare due to permanent kidney failure, your coverage will stop: 12 months after the month dialysistreatments are stopped. 36 months following the month youhave a kidney transplant.
ESRD MEDICARE GUIDELINES - National Kidney Foundation
1 ESRD MEDICARE GUIDELINES A. Eligibility Not all individuals with ESRD are eligible for Medicare. In addition to ESRD, one of the following criteria must be met:
CY 2022 End Stage Renal Disease Prospective Payment System Final Rule ...
Today, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that updates payment rates under the End-Stage Renal Disease (ESRD) Prospective Payment System (PPS) for renal dialysis services furnished to beneficiaries on or after January 1, 2022. This rule also finalizes updates to the Acute Kidney Injury (AKI) dialysis payment rate for renal dialysis services furnished by ESRD ...
ESRD Conditions for Coverage (CfCs) Final Rule Rollout Frequently Asked ...
7. Q. Under Subpart D, condition 494.140 (personnel qualifications), standard d (social worker), will there be any exceptions or grandfathering for social workers who do not have
ESRD Medicare costs and coverage - Medicare Interactive
Medicare covers the following care related to End-Stage Renal Disease (ESRD):. Kidney transplants; Hospital inpatient dialysis; Outpatient dialysis from a Medicare-certified hospital or free-standing dialysis facility; Home dialysis training, sometimes called self-dialysis, from a dialysis facility Training for you and caregivers who will provide home dialysis
End stage renal disease (ESRD) billing requirements
Condition code. Definition. 59. Non-primary ESRD facility. 70. Self-administered Anemia Management Drug (EPO) 80. ESRD beneficiary receiving home dialysis in nursing facilities, including SNFs (report along with condition code 74)
Medicare Coverage of Kidney Dialysis & Kidney Transplant Services.
6 Section 1: Medicare basics Determine if you’re eligible You can get Medicare no matter how old you are if your kidneys no longer work, you need regular dialysis or have had a kidney transplant, and one of these applies
What is ESRD in Medicare?
End stage renal disease (ESRD) is also known as permanent kidney failure. With this condition, your kidneys can no longer function on their own and you need regular dialysis or a kidney transplant. Medicare provides medical coverage for eligible people of all ages with ESRD.
When will ESRD be available for Medicare?
If you want to switch from original Medicare to a Medicare Advantage plan, you will be able to do so during the annual open enrollment period, which takes place from October 15 through December 7.
What is ESRD?
If your kidneys become damaged and are unable to do their job, kidney failure may eventually occur. Approximately 750,000 people in the United States have ESRD. People with ESRD account for 1 percent of the U.S. Medicare population, but 7 percent of its annual budget.
How long does ESRD last?
If you only have Medicare because you have ESRD, your coverage will end 12 months after you stop dialysis treatment or 36 months after you have a kidney transplant.
How much does Medicare pay for ESRD?
This means that Medicare pays an average of $80,000 per person or $36 billion total per year on ESRD treatments.
What causes kidney damage?
The most common cause of kidney damage is diabetes, followed by high blood pressure. Urinary tract problems, autoimmune diseases such as lupus, and genetic conditions such as polycystic kidney disease or Alport syndrome can also be the cause.
When does Medicare start?
Your eligibility for Medicare will begin 3 months after the date you start regular dialysis or receive a kidney transplant.
How long does it take for Medicare to pay for kidney transplant?
For example, if the beneficiary gets a kidney transplant that continues to work for 36 months, Medicare coverage will end. If after 36 months the beneficiary enrolls in Medicare again because they start dialysis or get another transplant, the Medicare coverage will start right away. There will be no 3-month waiting period before Medicare begins to pay.
What does the beneficiary expect to do after home dialysis training?
The beneficiary expects to finish home dialysis training and give self-dialysis treatments.
How long is Medicare based on ESRD?
Medicare is the secondary payer to group health plans (GHPs) for individuals entitled to Medicare based on ESRD for a coordination period of 30 months regardless of the number of employees and whether the coverage is based on current employment status.
How long does Medicare cover a transplant?
Medicare coverage can start two months before the month of the transplant if the transplant is delayed more than two months after the beneficiary is admitted to the hospital for that transplant or for health care services that are needed before the transplant.
What is the term for a kidney that stops working?
End-Stage Renal Disease (ESRD) End-Stage Renal Disease (ESRD) is a medical condition in which a person's kidneys cease functioning on a permanent basis leading to the need for a regular course of long-term dialysis or a kidney transplant to maintain life.
What is home dialysis training?
The beneficiary takes part in a home dialysis training program in a Medicare-approved training facility to learn how to do self-dialysis treatment at home;
When does Medicare start?
2. Medicare coverage can start as early as the first month of dialysis if:
When does Medicare start ESRD?
When your ESRD Medicare begins depends on your treatment plan: If you start a home dialysis training program, sometimes called self-dialysis, you are eligible for Medicare starting the first day of the first month of the home dialysis program. You must start the program before your third month of dialysis.
How to find out if you qualify for ESRD?
Contact the Social Security Administration (SSA) at 800-772-1213 to learn if you have enough work history to qualify for ESRD Medicare.
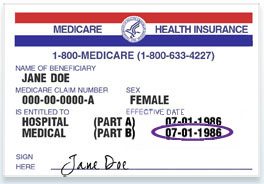
How old do you have to be to qualify for Medicare?
ESRD Medicare eligibility. To be eligible for ESRD Medicare, you must be under 65 and diagnosed with ESRD by a doctor. Additionally, you must have enough work history to qualify for Social Security Disability Insurance (SSDI) or Social Security retirement benefits, or enough railroad work history to qualify for Railroad Retirement benefits ...
Does Medicare cover kidney transplants?
Medicare for those with End-Stage Renal Disease (ESRD Medicare) provides you with health coverage if you have permanent kidney failure that requires dialysis or a kidney transplant. ESRD Medicare covers a range of services to treat kidney failure.
How long does it take to get Medicare Part D if you have ESRD?
If you qualify for Medicare because of ESRD, you will also be eligible to join a Medicare Part D prescription drug plan beginning three months before your date of Medicare eligibility and continuing for another three months thereafter.
What is a Medigap plan?
Medigap, or Medicare Supplement Insurance, helps cover some of the out-of-pocket costs associated with Original Medicare such as deductibles, copayments and coinsurance. Medigap plans are sold by private insurance companies, but the benefits they offer are somewhat regulated by the federal government.
What is the Medicare Advantage Plan called in 2021?
These beneficiaries were only eligible to join a type of Medicare Advantage plan called a Medicare Special Needs Plan (S NP).
Do You Have to Sign Up for Medicare If You Have ESRD?
While you don’t have to sign up for Medicare if you have ESRD, most people typically do, as Medicare Part A and Part B cover certain dialysis services and kidney transplants, as well as an extensive list of other benefits.
What is a Medigap plan?
Medigap is supplemental insurance that helps meet costs such as deductibles, copays, and coinsurances. Depending on a person’s policy, a plan may offer coverage for several expenses, including original Medicare’s out-of-pocket costs and some skilled nursing care costs.
Does Medicare cover kidney transplant surgery?
Medicare Part A traditionally covers hospitalizations and some surgeries, such as kidney transplant surgery. If a person qualifies for Medicare coverage based on their age (65 years and older) and undergoes dialysis, Part A will cover the costs.
What is the third requirement for Medicare to be the secondary payer under ESRD?
The third requirement for Medicare to be the secondary payer under ESRD is that the beneficiary is within a 30-month coordination period.
How long does Medicare last after kidney transplant?
Also, Medicare entitlement for an individual will end if he/she and has not received dialysis for 12 months or if 36 months have passed since the beneficiary has had a successful kidney transplant.
How long does it take for Medicare to become the primary payer?
Medicare becomes the primary payer of benefits after the 30-month coordination period ends, as long as the individual retains Medicare eligibility based on ESRD. A beneficiary may have more than one 30 - month coordination period.
How old do you have to be to be on Medicare?
The first requirement we will examine is that the beneficiary is on Medicare solely due to ESRD. Typically, the beneficiary will be under age 65, however, it is possible, although rare, for a beneficiary to be age 65 or older and on Medicare due solely to ESRD.
How long is the coordination period for Medicare?
If, for example, an individual fails to submit a timely application for Medicare or chooses not to apply for Medicare, the 30-month coordination period will be calculated with a start date based on the month in which he/she could have been enrolled, had an application for Medicare been made.
When does Medicare become the secondary payer?
If the individual obtains GHP coverage at any time during the 30-month coordination period, Medicare becomes the secondary payer for the balance of the coordination period.
When does Medicare start?
Medicare coverage usually starts the first day of the third month after the month in which a course of regular dialysis begins.
What is ESRD?
If your kidneys become damaged and are unable to do their job, kidney failure may eventually occur. Approximately 750,000 people in the United States have ESRD. People with ESRD account for 1 percent of the U.S. Medicare population, but 7 percent of its annual budget.
How long does ESRD last?
If you only have Medicare because you have ESRD, your coverage will end 12 months after you stop dialysis treatment or 36 months after you have a kidney transplant.
What is ESRD in Medicare?
End stage renal disease (ESRD) is also known as permanent kidney failure. With this condition, your kidneys can no longer function on their own and you need regular dialysis or a kidney transplant. Medicare provides medical coverage for eligible people of all ages with ESRD.
How much does Medicare pay for ESRD?
This means that Medicare pays an average of $80,000 per person or $36 billion total per year on ESRD treatments.
What causes kidney damage?
The most common cause of kidney damage is diabetes, followed by high blood pressure. Urinary tract problems, autoimmune diseases such as lupus, and genetic conditions such as polycystic kidney disease or Alport syndrome can also be the cause.
When will ESRD be available for Medicare?
If you want to switch from original Medicare to a Medicare Advantage plan, you will be able to do so during the annual open enrollment period, which takes place from October 15 through December 7.
When does Medicare start?
Your eligibility for Medicare will begin 3 months after the date you start regular dialysis or receive a kidney transplant.