How do you become dual eligible for Medicare and Medicaid?
- Estate Recovery
- MAGI Conversion Plan
- Seniors & Medicare and Medicaid Enrollees
- Verification Plans
- Minimum Essential Coverage
- Spousal Impoverishment
- Medicaid Third Party Liability & Coordination of Benefits
- Medicaid Eligibility Quality Control Program
Does Someone on Medicaid automatically qualify for Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
What is dual eligibility for Medicare and Medicaid?
Dual eligibility for Medicare and Medicaid means that you’re enrolled in Medicare and either: receiving full Medicaid benefits; receiving assistance with Medicare premiums
Is Medicare better than Medicaid?
Ultimately, Medicare is a program meant to provide healthcare to Americans age 65 or older (as well as Americans younger than 65 with qualifying disability) while Medicaid is designed to help provide healthcare to low income Americans without any age limit. A few differences between the programs include: Equal but separate.
When can a patient have both Medicare and Medicaid?
Some people qualify for both Medicare and Medicaid and are called “dual eligibles.” If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered. You can get your Medicare coverage through Original Medicare or a Medicare Advantage Plan.
When a patient is covered through Medicare and Medicaid which coverage is primary?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
Can I have dual coverage with Medicare?
If you qualify for both Medicare and Medicaid, you are considered "dual eligible." Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
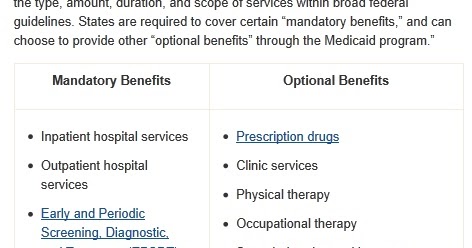
Do Medicaid and Medicare cover the same things?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
What is the point of secondary insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance. Secondary insurance can help you improve your coverage by giving you access to additional medical providers, such as out-of-network doctors. It can also provide benefits for uncovered health services, such as vision or dental.
Can you use 2 insurance plans?
While it sounds confusing, having dual insurance like this is perfectly legal—you just need to make sure you're coordinating your two benefits correctly to make sure your medical expenses are being covered compliantly.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is the medical income limit for 2021?
For dependents under the age of 19, a household income of 266 percent or less makes them eligible for Medi-Cal. A single adult can earn up to $17,775 in 2021 and still qualify for Medi-Cal. A single adult with one dependent can earn up to $46,338 annually and the child will still be eligible for Medi-Cal.
Can medical check your bank account?
While Medicaid agencies do not have independent access to a Medicaid recipient's financial statements, Medicaid does an annual update to make sure a Medicaid recipient still meets the financial eligibility requirements. Furthermore, a Medicaid agency can ask for bank statements at any time, not just on an annual basis.
Which state has highest income limit for Medicaid?
AlaskaThe state with the highest income limits for both a family of three and individuals is Washington, D.C. If you live in this area, a family of three can qualify for Medicaid if their income is at 221% of the FPL....Medicaid Income Limits by State 2022.StateAlaskaParents (Family of 3)138.00%Other Adults138.00%2022 Pop.720,76349 more columns
Who is not eligible for Medicare?
Did not work in employment covered by Social Security/Medicare. Do not have 40 quarters in Social Security/Medicare-covered employment. Do not qualify through the work history of a current, former, or deceased spouse.
Who is not eligible for Medicare Part A?
Why might a person not be eligible for Medicare Part A? A person must be 65 or older to qualify for Medicare Part A. Unless they meet other requirements, such as a qualifying disability, they cannot get Medicare Part A benefits before this age. Some people may be 65 but ineligible for premium-free Medicare Part A.
What is the eligibility criteria for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Who are the dual-eligible recipients?
People who are dual-eligible for Medicare and Medicaid are referred to as dual-eligible beneficiaries. Moreover, each state determines Medicaid coverage, and as a result, Medicaid benefits may differ.
Medicare Ineligibility
The Medicare eligibility requirement is that you must be 65 years old or older. If you or your spouse are 65 years old or older and have paid enough Medicare taxes through previous employment, you or your spouse may be eligible for premium-free Part A of the Medicare program (hospital coverage).
Medicaid Ineligibility
Medicaid eligibility varies depending on where a person resides, as various states have different qualifications.
Dual eligibility
A person must qualify for either partial-dual or full-dual coverage to be eligible for both Medicare and Medicaid.
Variations in geography
Medicaid benefits and coverage vary from one state to the next, and there are differences between them. Depending on the state, Medicaid coverage may be available to those who earn more than the standard income limits.
Medicare Part D Extra Assistance Program
Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual.
Summary
A person’s health and income level may qualify them for both Medicare and Medicaid.
How old do you have to be to get medicare?
You’re eligible for Medicare if you’re over the age of 65 or on disability for at least 24 months. Although, you apply for Medicare online at the Social Security Administration website.
How long does it take for medicaid to approve?
Approval time for Medicaid can take up to 60 days. Benefits are for US citizens; but, children of illegal immigrants can qualify. If you get Social Security supplemental benefits, you’ll qualify for Medicaid. Also, Medicaid has benefits Medicare doesn’t; this includes vision, dental, and long-term custodial care.
Can you disenroll with Medicare Dual Eligible?
Is there a Special Enrollment Period for Medicare Dual-Eligible? Those with Medicaid and Medicare qualify for a Special Enrollment Period; you can disenroll, join, or switch plans. The Special Enrollment Period begins the month a person is eligible for assistance.
Is Medicare free for low income people?
With Medicare, think “care” for those 65+ or those with disabilities. Then, Medicaid is “aid” to those with a low income. Medicaid is free. Medicare is not free.
Does medicaid cover Medicare?
Criteria for Medicaid can differ between states. Medicaid pays the part that Medicare doesn’t cover with partial dual-eligibility. Further, Medicaid will cover your Part B premiums, and if applicable, Part A. Beneficiaries who qualify for both are dual-eligible.
Is Medicare a federal or state program?
But, just because you have one, doesn’t mean you’ll automatically have the other. Medicare is a federal program, while Medicaid is a state program.
Is medicaid free?
Medicaid is free. Medicare is not free. Those with Medicaid won’t be subject to the Part B premium or Part B late enrollment penalties. But, those with only Medicare will be responsible for applicable costs. Just because Medicaid is free doesn’t mean it’s for everyone. Approval time for Medicaid can take up to 60 days.
What Is Medicare?
Before we dive into dual-eligibility, let’s start off by defining each program. In order to qualify for Medicare, the requirements are straightforward.
What Is Medicaid?
Medicaid is administered by state governments. This is unlike Medicare, which is a federal program.
Can I Qualify for Both Medicare and Medicaid?
Millions of people qualify for both entitlement programs. This is a good thing because Medicare does not cover all medical expenses. Medicare enrollees are often left with bills for deductibles, copayments, and coinsurance.
Your Guide to Medicare and Medicaid Benefits
If you qualify for both, it is highly recommended to apply. Dual-eligibility is going to ensure the lowest possible cost to your family. Health care that Medicare does not cover is often picked up by Medicaid.
What is the difference between Medicare and Medicaid?
Takeaway. Medicare is the federal health insurance program in the United States for people age 65 and older. Medicaid is a joint federal and state program to help people with limited resources or income pay for medical costs.
How many people are on Medicare and Medicaid?
According to Health Affairs, about 9.2 million people, representing about 16 percent of Medicare enrollees and about 15 percent of Medicaid enrollees, are enrolled in both Medicare and Medicaid. Keep reading to learn more about dual eligibility, benefits, and state-by-state differences.
What is dual eligibility?
You’re also considered a dual eligible beneficiary if you’re enrolled in Medicare Part A or Part B and receiving cost-sharing through a Medicare savings program (MSP). Below is table summarizing the benefits and eligibility criteria for each of the different MSPs in 2021: MSP. Benefits.
What is fee for service Medicaid?
fee-for-service Medicaid coverage. plans that include all Medicare and Medicaid benefits. Income and resource standards are defined by federal law for full Medicaid and the Medicare Savings Programs. At their discretion, states can effectively raise the federally mandated limits.
Is Medicare a dual beneficiary?
If you’re eligible for both Medicare and Medicaid, you’re considered a dual eligible beneficiary. Dual eligibility is typically determined by your age, any disabilities, and income.
Is Medicare free for older people?
It also covers people with certain disabilities and health conditions. Medicare is not free coverage — you’ll still pay deductibles, premiums, and copays for medical services.
Is dual eligibility covered by insurance?
If you’re a dual eligibility beneficiary, it’s likely that most of your healthcare costs are covered. The information on this website may assist you in making personal decisions about insurance, but it is not intended to provide advice regarding the purchase or use of any insurance or insurance products.
Understanding what the two programs are
Just when you think that Medicare itself cannot get any more confusing, it does. But, for some Americans, it becomes more confusing in a positive way.
What is Medicare?
If you’re familiar with The Best Senior Services’ website and blogs, then you’re probably familiar with the available Medicare plans out there. But for those who are new here and wanting to learn more about the program, Medicare is a health insurance program that covers Americans who are at least 65 years old.
What is Medicaid?
Medicaid has been around since 1965, the same year Medicare was implemented. It is a federal program that helps with healthcare costs for millions of Americans, like children, pregnant women, seniors, Americans with disabilities and more.
How do I qualify for Medicare and Medicaid programs?
Luckily for many, the qualifications outlined by Medicare and Medicaid are cut-and-dry, meaning you’ll have a great understanding of whether you’re eligible before you begin the application process. Those who are eligible for Medicare’s services typically tend to be at least 65 years old.
Can I qualify for both Medicare and Medicaid?
The short answer is: yes! If you’re qualified for Medicaid, you can qualify for Medicare, too, and vice versa. When you qualify for both programs, it’s known as having ”Dual Eligibility.” And for those with Dual Eligibility, there is a possibility that all of your healthcare costs will be covered.
Dual Enrollment Is Available for Low-Income Individuals
Medicare and Medicaid are two separate programs, each with different eligibility requirements. Individuals must enroll on Medicare and Medicaid separately. All seniors who are eligible for retirement Social Security benefits are entitled to Medicare. In addition, many people who are living with a disability will be able to claim Medicaid.
Some Seniors May Qualify for Other Medical-Related Assistance
In addition to Medicaid, many seniors may be eligible for other assistance, depending on the state they reside in. For example, many states offer a Home and Community Based Services waiver that provides support with all or part of the cost of assisted living or other long-term care.
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
What is dual eligible for medicaid?
Qualifications for Medicaid vary by state, but, generally, people who qualify for full dual eligible coverage are recipients of Supplemental Security Income (SSI). The SSI program provides cash assistance to people who are aged, blind, or disabled to help them meet basic food and housing needs.
When will Medicare become the main health insurance?
July 08, 2020. Most Americans understand that when they turn 65, Medicare will become their main health insurance plan. However, many Americans are less familiar with another health care program, Medicaid, and what it means if they are eligible for both Medicare and Medicaid. If you are dual eligible, Medicaid may pay for your Medicare ...
What is Medicare Advantage?
Medicare Advantage plans are private insurance health plans that provide all Part A and Part B services. Many also offer prescription drug coverage and other supplemental benefits. Similar to how Medicaid works with Original Medicare, Medicaid wraps around the services provided by the Medicare Advantage plan andserves as a payer of last resort.
What is dual eligible?
The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”.
What is Medicaid managed care?
Medicaid managed care is similar to Medicare Advantage, in that states contract with private insurance health plans to manage and deliver the care. In some states, the Medicaid managed care plan is responsible for coordinating the Medicare and Medicaid services and payments.
Does Medicare cover Part A and Part B?
Some Medicare beneficiaries may choose to receive their services through the Original Medicare Program. In this case, they receive the Part A and Part B services directly through a plan administered by the federal government, which pays providers on a fee-for-service (FFS) basis. In this case, Medicaid would “wrap around” Medicare coverage by paying for services not covered by Medicare or by covering premium and cost-sharing payments, depending on whether the beneficiary is a full or partial dual eligible.
Is Medicaid a payer of last resort?
Medicaid is known as the “payer of last resort.”. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid.

Who Are The Dual-Eligible Recipients?
Medicare Ineligibility
Medicaid Ineligibility
Dual Eligibility
Variations in Geography
Medicare Part D Extra Assistance Program
Summary
- A person’s health and income level may qualify them for both Medicare and Medicaid. Meanwhile, Medicare will generally cover healthcare costs initially, and Medicaid assists with out-of-pocket and non-covered expenses. Medicaid eligibility varies by state, as well as the income level restrictions.