Full Answer
How soon before 65 should I apply for Medicare?
You can apply up to four months before you want your retirement benefits to start. For example, if you turn 62 on December 2, you can start your benefits as early as December, and apply in August. Even if you are not ready to retire, you still should sign up for Medicare three months before your 65th birthday.
Are you automatically enrolled in Medicare at age 65?
Unless you have already been receiving benefits from Social Security or the Railroad Retirement Board at least four months before you turn 65, you will not be automatically enrolled in Medicare when you turn 65. You will need to sign up for Medicare yourself by applying with Social Security. Keeping Your Medicare Card Safe
Can you buy into Medicare before age 65?
You typically must be at least 65 years old to receive Medicare, even if you are receiving Social Security retirement benefits. There are some exceptions to this rule, however. Although reaching age 62 does not qualify you for Medicare, it can carry some significance for your spouse if they receive Medicare benefits.
Who can get Medicare before age 65?
You could be eligible for Medicare before you reach age 65 if you have:
- Social Security disability
- RRB disability pension
- specific health conditions
- family relationship

What happens if I enroll in Medicare after age 65?
Most people age 65 or older are eligible for free Medical hospital insurance (Part A) if they have worked and paid Medicare taxes long enough. You can enroll in Medicare medical insurance (Part B) by paying a monthly premium. Some beneficiaries with higher incomes will pay a higher monthly Part B premium.
Does Medicare automatically kick in at 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Do I have to switch to Medicare when I turn 65?
As long as you have group health insurance from an employer for which you or your spouse actively works after you turn 65, you can delay enrolling in Medicare until the employment ends or the coverage stops (whichever happens first), without incurring any late penalties if you enroll later.
Is it ever too late to sign up for Medicare?
If you don't enroll in Medicare during the initial enrollment period around your 65th birthday, you can sign up during the general enrollment period between Jan. 1 and March 31 each year for coverage that will begin July 1. However, you could be charged a late enrollment penalty when your benefit starts.
Do they automatically send you a Medicare card?
You should automatically receive your Medicare card three months before your 65th birthday. You will automatically be enrolled in Medicare after 24 months and should receive your Medicare card in the 25th month.
What documents do I need to apply for Medicare?
What documents do I need to enroll in Medicare?your Social Security number.your date and place of birth.your citizenship status.the name and Social Security number of your current spouse and any former spouses.the date and place of any marriages or divorces you've had.More items...
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Is Medicare Part A free?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
Do you have to enroll in Medicare Part B every year?
Do You Need to Renew Medicare Part B every year? As long as you pay the Medicare Part B medical insurance premiums, you'll continue to have the coverage. The premium is subtracted monthly from most people's Social Security payments. If you don't get Social Security, you'll get a bill.
How long does it take for Medicare approval?
between 30-60 daysMedicare applications generally take between 30-60 days to obtain approval.
What are the 3 enrollment periods for Medicare?
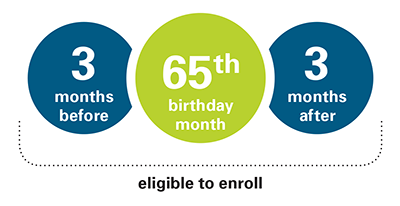
Initial Enrollment Period3 months before.Your 65th birthday month.3 months after.7-month window.
How long does it take to get a new Medicare card?
Within 3-4 weeks, you should receive a letter confirming your application for coverage is approved. Your new Medicare card will arrive soon after.
How to enroll in Medicare Part B?
When your number is called, take the forms to the Social Security employee and inform them you wish to enroll in Medicare Part B utilizing Medicare’s Special Enrollment Period (SEP) process. Since you are within 90 days of your requested effective date, they are required to process your enrollment. Don’t let them tell you to come back when you are closer to your enrollment start date. However, they could ask you to come back another day if they aren’t taking any more walk-ins that particular day. They will stamp your paperwork and provide you a copy.
How long is the Medicare enrollment period?
When you’re first eligible for Medicare, there is a 7-month Initial Enrollment Period (IEP). Your IEP spans the three months prior to your birthday month, your birthday month, and the three months after your birthday month. But what if you don’t plan to enroll in Medicare at age 65?
What happens if you don't sign up for Medicare?
Specifically, if you fail to sign up for Medicare on time, you’ll risk a 10 percent surcharge on your Medicare Part B premiums for each year-long period you go without coverage upon being eligible.
How long does it take to get Medicare?
Learn how to make sure they have health insurance once you’re enrolled. Medicare eligibility starts at age 65. Your initial window to enroll is the seven-month period that begins three months before the month of your 65th birthday and ends three months after it. Seniors are generally advised to sign up on time to avoid penalties ...
When do you get Medicare if you leave your job?
In that case, you’ll get an eight-month special enrollment period to sign up for Medicare if and when you leave your job or your employer stops offering coverage. It will start the month after you separate from your employer, or the month after your group health coverage ends – whichever happens sooner.
How long do you have to sign up for a Part B plan?
Sign up during those eight months, and you won’t have to worry about premium surcharges for being late. And the eight-month special enrollment period is also available if you’re delaying Part B enrollment because you’re covered under your spouse’s employer-sponsored plan, assuming their employer has at least 20 employees.
Do you have to double up on Medicare?
No need to double up on coverage. Many seniors are no longer employed at age 65, and thus rush to sign up for Medicare as soon as they’re able. But if you’re still working at 65, and you have coverage under a group health plan through an employer with 20 employees or more, then you don’t have to enroll in Medicare right now.
Does Medicare pay for Part A?
That said, it often pays to enroll in Medicare Part A on time even if you have health coverage already. It won’t cost you anything, and this way, Medicare can serve as your secondary insurance and potentially pick up the tab for anything your primary insurance (in this case, your work health plan) doesn’t cover.
How to get Medicare documents from Social Security?
There are several ways to get these documents to Social Security to prove you had creditable coverage and have a Special Enrollment Period to apply for Medicare. You may upload the forms to the Social Security site while you are applying, mail the forms to Social Security, take them in-person to your local office, or in some situations, you may fax them. Based on feedback from our clients, uploading them to the Social Security site while you are applying for Medicare tends to achieve the fastest processing results.
How long is the GI window for Medicare?
However, your GI window is only 63 days long, and does not apply to every Medigap plan. If you were eligible for Medicare prior to 2020, you can get GI for Plan A, B, C, F, K, and L. If you became eligible for Medicare in 2020 or later, the GI is available to you for Plan A, B, D, G, K, and L.
How long is the Medigap open enrollment period?
Your Medigap Open Enrollment window is a 6-month period that begins the day your Part B starts.
How long does it take to get backdated Social Security?
If you apply for Part A (and Social Security) and you are six months or more beyond your full retirement age, you will get six months of backdated benefits from Social Security. Since Social Security and Medicare Part A go hand-in-hand, this means your Part A effective date will also retroact six months.
What to do if employer cannot complete CMS L564?
If your employer cannot complete their portion of Form CMS-L564, you can complete Section A, leave Section B blank, and include at least one other acceptable proof of group health coverage. Proof of creditable coverage may include but is not limited to:
Can you delay Medicare if you are 65?
By delaying Medicare and staying on employer coverage past 65, you will have a different enrollment process when it comes time to retire than those who enroll during their Initial Enrollment Period (IEP).
Is Medicare Part D voluntary?
Medicare Part D. If you have delayed Medicare Parts A and B, you have also delayed Part D. Enrolling in Part D is voluntary but even if you do not currently take prescription drugs, it is in your best interest to enroll to avoid penalties for signing up late.
When do you sign up for Medicare at 65?
When you near your 65th birthday, you will enter what is called your Initial Enrollment Period (IEP). This seven-month period begins three months before you turn 65, includes the month of your birthday and continues for three additional months. This is your first opportunity to sign up for Medicare.
Why don't people sign up for Medicare at 65?
The most common reason for people not signing up for Medicare when they turn 65 is because they are still working. Because they’re still working, they’re likely covered under their employer’s health insurance plan and are also unlikely to be collecting Social Security retirement benefits.
Is it mandatory to sign up for Medicare at 65?
Technically, it is not mandatory to sign up for Medicare at 65 or at any age, for that matter. But it’s important to consider the situations in which you might decide not to enroll in Medicare at 65 so that you can make sure not to have any lapse in health insurance coverage or face a Medicate late enrollment penalty.
Does Medicare cover health insurance?
Being covered under your employer-provided health insurance plan has no bearing on your Medicare eligibility. Medicare works in conjunction with several other types of health insurance – including health insurance provided by employers or unions – and won’t prevent you from enrolling.
Does Medicare have a late enrollment penalty?
Medicare Part D, which provides coverage for prescription medications, is optional but can also come with a late enrollment penalty if you don’t sign up when you’re supposed to. This penalty is a little more complex to calculate but remains in place for as long as you have Part D coverage. The Part D late enrollment penalty applies if you experience a stretch of at least 63 consecutive days without creditable drug coverage following your IEP and then later enroll in a Part D plan.
When is the best time to enroll in Medicare Supplement?
Medicare Supplement insurance – this coverage may help pay your Medicare Part A and Part B costs, like copayments, coinsurance, and deductibles. You need Part A and Part B to qualify. Usually the best time to enroll is during your Medicare Supplement Open Enrollment Period. That 6-month period starts the month you’re both 65 or older, and enrolled in Part B.
What if you are still working at 65?
What if you’re still working when you hit 65? If you qualify for Medicare, but you’re not getting Social Security benefits yet, you usually don’t get enrolled automatically in Medicare.
What is a stand alone Medicare plan?
Stand-alone Medicare prescription drug plan (Medicare Part D) – you might want this type of plan if you need prescription drug coverage. You need Part A or Part B to qualify. If you don’t enroll during your Medicare Initial Enrollment Period (IEP), you might have to wait to sign up.
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) – this program gives you an alternative way to get your Medicare Part A and Part B benefits (many plans also include prescription drug benefits too). You need Part A and Part B to qualify, and then the plan (instead of the government) manages those benefits for you.
Do you have to take action if you are automatically enrolled in Medicare?
But even if you’re automatically enrolled in traditional Medicare, you do have to take action if you want other Medicare coverage.
Is Medicare Part A premium free?
Enroll in Medicare Part A as soon as they’re eligible. Even if your employer plan has hospital coverage, Part A is premium-free for most people. If your employer plan has hospital coverage, and you have a hospital stay, your plan and Medicare Part A will coordinate benefits to work out payment of your hospital costs.
Is it a good idea to sign up for Medicare?
Then, it’s usually a good idea to sign up for any other type of Medicare coverage you want, promptly. Here’s a quick rundown on the main Medicare coverage options you have besides Original Medicare – and when to sign up.
What happens if you overlook Medicare enrollment rules?
Medicare processes and rules are complex and rife with exceptions; if you overlook something in the enrollment rules, you may pay a high price in terms of both penalties and gaps in coverage. So you should consult with Medicare and with the benefits administrator for your employer coverage — before you enroll or decide to delay enrollment.
How long do you have to work to get Medicare Part A?
If by the time you reach 65 you’ve worked a total of approximately 10 years over your career, you’re entitled to premium-free Medicare Part A, which pays for in-patient hospital charges and more.
How many employees do you have to have to have Medicare Part B?
If the employer has fewer than 20 employees: If your or your spouse's employer has fewer than 20 employees and the health coverage is not part of a multiemployer group plan, at age 65 you must enroll in Medicare Part B, which will be your primary insurance. If you have an HSA and want to keep contributing: If you have an HSA ...
What is Medicare Part A?
If the employer has fewer than 20 employees: If your or your spouse's employer has fewer than 20 employees and the health coverage is not part of a multiemployer group plan, at age 65 you must enroll in Medicare Part A, which will be your primary insurance. “Primary” means that Medicare pays first, and then the employer insurance kicks in ...
How long do you have to keep HSA contributions?
Stop making contributions to your HSA at least six months before you sign up for Part B. And you’ll want to sign up for Medicare at least a month before you stop work ...
Does Medicare Part A cover my employer?
Because in some cases, Medicare Part A may cover what your employer plan does not. But as with so many aspects of Medicare, there are caveats, exceptions and potential pitfalls. If the employer has 20 or more employees: If your or your spouse's employer has 20 or more employees and a group health plan, you don't have to sign up for Medicare ...
Is Medicare cheaper than group health insurance?
If your employer (or your spouse’s employer) requires you to pay a large portion of the premium on your group health insurance, you may find Medicare cheaper and the coverage adequate. So compare your current coverage and out-of-pocket expenses — including premiums, deductibles, copays and coinsurance — with your costs and benefits under Medicare, which may also pay some expenses not covered by your group plan.
How far in advance can you start Medicare?
While active employment continues, you can specify the date on which you want Medicare coverage to begin, up to three months in advance. Otherwise, your coverage begins on the first day of the month after you enroll.
When is the Medicare enrollment period?
General Enrollment Period (GEP) If you miss the deadline for your IEP or SEP (or if you don’t qualify for a SEP), you can enroll in Medicare only during a general enrollment period, which runs from Jan. 1 to March 31 each year, with coverage not beginning until July 1 of the same year. If you need Medicare prescription drug coverage, ...
When is open enrollment for Medicare Part A?
Note: You cannot enroll in Medicare Part A or B for the first time during Medicare’s annual open enrollment period, which runs from Oct. 15 to Dec. 7 each year . This period is only for people already in Medicare who want to change their type of coverage for the following year. You can sign up with a Part D drug plan for the first time during open enrollment if you missed other deadlines for signing up.
How long can you join a health insurance plan?
You can join a plan anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
What happens if you miss the 8 month special enrollment period?
If you miss this 8-month Special Enrollment Period, you’ll have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B. The penalty goes up the longer you wait to sign up.
When does the 8 month special enrollment period start?
Your 8-month Special Enrollment Period starts when you stop working, even if you choose COBRA or other coverage that’s not Medicare.
Does Cobra end with Medicare?
Your COBRA coverage will probably end when you sign up for Medicare. (If you get Medicare because you have End-Stage Renal Disease and your COBRA coverage continues, it will pay first.)
Do you have to tell Medicare if you have non-Medicare coverage?
Each year your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan. (Don’t send this information to Medicare.)