
What is the notice of Medicare non-coverage (nomnc)?
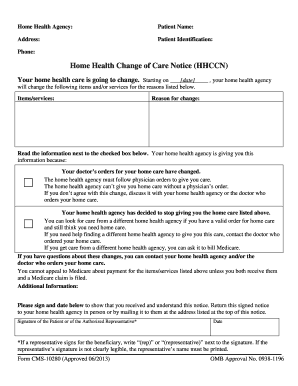
collectively referred to as “plans”) must deliver a completed copy of the Notice of Medicare Non-Coverage (NOMNC) to beneficiaries/enrollees receiving covered skilled nursing, home health (including psychiatric home health), comprehensive outpatient rehabilitation facility , and hospice services. The NOMNC must be delivered at least two calendar days before Medicare covered
What does nomnc stand for?
A Notice of Medicare Non-Coverage (NOMNC) is a notice that indicates when your care is set to end from a home health agency (HHA), skilled nursing facility (SNF), comprehensive outpatient rehabilitation facility (CORF), or hospice. It includes information for how to appeal the provider ’s decision to a Quality Improvement Organization (QIO).
Is nomnc required for Medicare Advantage patients?
Dec 01, 2021 · HHAs, SNFs, Hospices, and CORFs are required to provide a Notice of Medicare Non-Coverage (NOMNC) to beneficiaries when their Medicare covered service (s) are ending. The NOMNC informs beneficiaries on how to request an expedited determination from their Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) and gives ...
Where can I find the MAED notice of Medicare non-coverage (nomnc)?
a nomnc is a centers for medicare and medicaid services (cms) approved form that a provider must deliver to a patient covered under a medicare advantage or dsnp plan who is receiving covered skilled services, such as home health agency (hha), skilled nursing facility (snf), and comprehensive outpatient rehabilitation facility (corf) services, in …
When must you provide a client with an Nomnc Notice of Medicare non-coverage?
When to Deliver the NOMNC The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily.
Who is responsible for issuing Nomnc?
Providers must deliver the NOMNC to all beneficiaries eligible for the expedited determination process per §260.2. A NOMNC must be delivered even if the beneficiary agrees with the termination of services. Medicare providers are responsible for the delivery of the NOMNC.May 24, 2013
What is a Notice of Medicare non-coverage form?
Informs beneficiaries of their discharge when their Medicare covered services are ending. Issued by: Centers for Medicare & Medicaid Services (CMS)Dec 30, 2020
Can a Nomnc be rescinded?
Any changes likely due to medical and may result in rescinding the NOMNC for ongoing skilled (in some instances). Question: We were told that if someone discharges from Managed Medicare directly to Hospice care, and NOMNC is not needed.
What is the purpose of the Nomnc?
A Notice of Medicare Non-Coverage (NOMNC) is a notice that indicates when your care is set to end from a home health agency (HHA), skilled nursing facility (SNF), comprehensive outpatient rehabilitation facility (CORF), or hospice.
What does Nomnc stand for?
Notice of Medicare Non-CoverageA Medicare health provider must give an advance, completed copy of the Notice of Medicare Non-Coverage (NOMNC) to enrollees receiving skilled nursing, home health (including psychiatric home health), or comprehensive outpatient rehabilitation facility services, no later than two days before the termination of services.
How do you explain ABN to patients?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
What is an Advance beneficiary Notice of Non-Coverage?
The Advance Beneficiary Notice of Non-coverage (ABN), Form (CMS-R-131) helps Medicare Fee-for-Service (FFS) beneficiaries make informed decisions about items and services Medicare usually covers but may not cover in specific situations.
What is a DENC form?
Detailed Explanation of Non-Coverage (DENC, Form CMS-10124) Explains the specific reasons for the end of covered services. Issued by: Centers for Medicare & Medicaid Services (CMS)Dec 30, 2020
Under which scenario would both a Nomnc and SNF ABN be required?
General Response: The provider cannot give a retroactive notice. The patient was admitted under Medicare benefits. Once the team determines the patient is “not at a skilled level of care,” the 2-day notice is required with the NOMNC and the SNF ABN provided.
How many additional pages are needed for a dual eligible NOMNC?
Additional Pages Needed: The 3 additional translation pages found with the Dual Eligible NOMNC are required to be given with the NOMNC. Link to this NOMNC can be found on slide 12.
How many points should a date be in a document?
Note that the date should be in no less than 12-point type. If handwritten, entries must be at least as large as 12- point type and legible.
Can non-coverage be used as a detailed explanation?
additional pertinent information that may be useful to the enrollee. It may not be used as the Detailed Explanation of Non-Coverage, even if facts pertinent to the termination decision are provided.
When is a NOMNC required?
Answer: The NOMNC is required 2 days before the end of therapy. The ABN is only used to communicate ongoing treatment the patient may request, and Medicare will likely not cover. The ABN would be provided timely to give the patient information needed to make the financial decision.
What is SNF ABN?
The SNF ABN (not the ABN - very different) is given as the financial responsibility and liability now shifts to the patient. Not all hospice patients have room and board covered if under routine hospice benefit. they are responsible for the daily rate.
How long is a Medicare extended treatment notice valid?
A single notice for an extended course of treatment is only valid for 1 year. If the extended course of treatment continues after 1 year, issue a new notice.
How long does it take for Medicare to refund a claim?
Medicare considers refunds timely within 30 days after you get the Remittance Advice from Medicare or within 15 days after a determination on an appeal if you or the beneficiary file an appeal.
Does Medicare cover frequency limits?
Some Medicare-covered services have frequency limits. Medicare only pays for a certain quantity of a specific item or service in each period for a diagnosis. If you believe an item or service may exceed frequency limits, issue the notice before furnishing the item or service to the beneficiary.
What happens if you terminate a service?
Terminations stop all or certain items or services. If you terminate services and the beneficiary wants to continue getting care no longer considered medically reasonable and necessary, you must issue the notice before the beneficiary gets the noncovered care.
When do you issue a reduction notice?
Reductions occur when a component of care decreases (for example, frequency or service duration). Do not issue the notice every time there is a reduction in care. If a reduction occurs and the beneficiary wants to continue getting care no longer considered medically reasonable and necessary, you must issue the notice before the beneficiary gets the noncovered care.
Is an ABN valid for Medicare?
An ABN is valid if beneficiaries understand the meaning of the notice. Where an exception applies, beneficiaries have no financial liability to a non-contract supplier furnishing an item included in the Competitive Bidding Program unless they sign an ABN indicating Medicare will not pay for the item because they got it from a non-contract supplier and they agree to accept financial liability.
