CMS continually monitors the quality of coverage provided by private Medicare plans and if a Medicare plan falls below CMS standards, the plan may be sanctioned and required to change internal practices or procedures before being allowed to market the plan again or enroll new members.
What's a Medicare health plan?
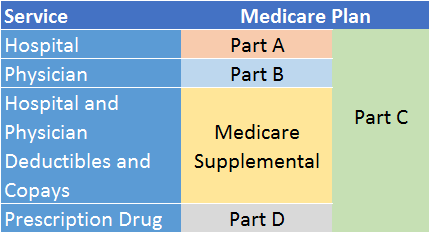
What's a Medicare health plan? Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What are the Medicare Advantage plan penalties?
The penalties come from a CMS oversight and enforcement group that found that between 2018 and 2020, the plans did not meet the 85 percent threshold of premium revenue spent on Medicare Advantage members, according to the Star Tribune .
What are the rules for meeting with a Medicare agent?
Independent agents and brokers selling plans must be licensed by the state, and the plan must tell the state which agents are selling their plans. If you're going to meet with an agent, the agent must follow all the rules for Medicare plans and some specific rules for meeting with you.
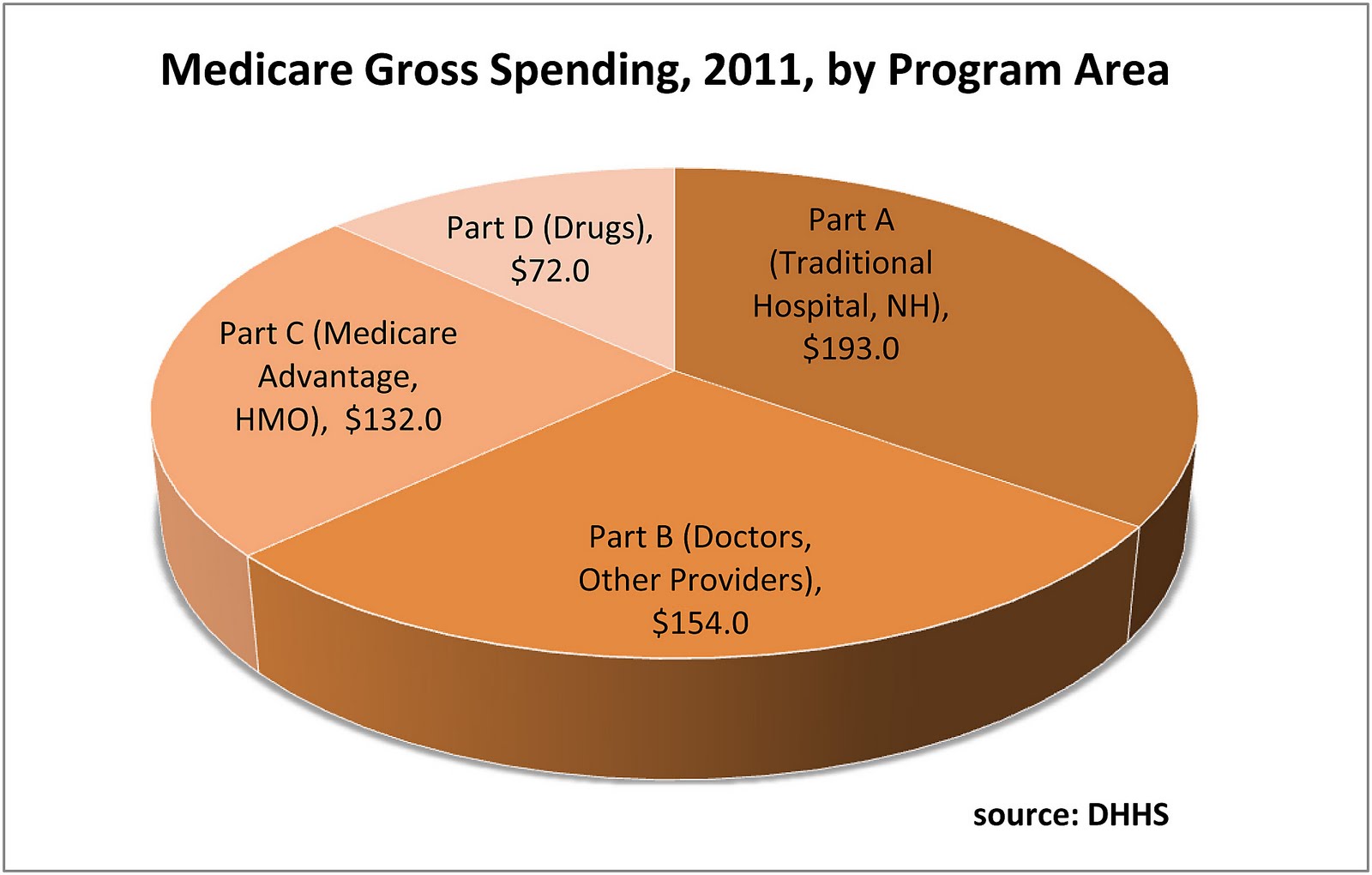
What are 4 types of Medicare plans?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What are the 2 types of Medicare plans?
Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). You can join a separate Medicare drug plan to get Medicare drug coverage (Part D). You can use any doctor or hospital that takes Medicare, anywhere in the U.S.
How does CMS ensure plans are compliant?
CMS will also conduct targeted market conduct examinations, as necessary, and respond to consumer inquiries and complaints to ensure compliance with the health insurance market reform standards. CMS will work cooperatively with the state to address any concerns.
What plans are regulated by CMS?
Health PlansHealth Plans - General Information.Health Care Prepayment Plans (HCPPs)Managed Care Marketing.Medicare Advantage Rates & Statistics.Medicare Cost Plans.Medigap (Medicare Supplement Health Insurance)Medical Savings Account (MSA)Private Fee-for-Service Plans.More items...
What are the 3 types of Medicare?
Different types of Medicare health plansMedicare Advantage Plans. ... Medicare Medical Savings Account (MSA) Plans. ... Medicare health plans (other than MA & MSA) ... Rules for Medicare health plans.
What are the top 3 Medicare Advantage plans?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCMS ratingHumana5.03.6Blue Cross Blue Shield5.03.8Cigna4.53.8United Healthcare4.03.81 more row•Feb 25, 2022
What is Medicare compliance?
The Medicare Compliance Program is specifically designed to prevent, detect, and correct noncompliance as well as fraud, waste, and abuse.
Does CMS require a compliance program?
The development and implementation of a compliance program is voluntary, but CMS believes that an effective compliance program is a cost-effective investment. It should be noted, however, that CMS is not specifically authorizing funding for any of the recommendations contained in this guidance.
What is the difference between compliance and enforcement?
Compliance: the state of conformity with regulatory requirements including, but not limited to, legislative provisions, regulations, rules, standards, and orders. Enforcement: actions taken to induce, encourage, or compel compliance with regulatory requirements.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What does regulated by CMS mean?
CMS regulations establish or modify the way CMS administers its programs. CMS' regulations may impact providers or suppliers of services or the individuals enrolled or entitled to benefits under CMS programs.
What does CMS stand for in Medicare?
Centers for Medicare & Medicaid ServicesHome - Centers for Medicare & Medicaid Services | CMS.