What it is Telehealth includes certain medical or health services that you get from your doctor or other health care provider using audio and video communications technology, like your phone or a computer (or audio-only telehealth services in some cases). Some examples of Medicare-covered telehealth services include:
Full Answer
Is Netflix free with T-Mobile Senior Plan?
Is there an offer for me? For those who want more, T-Mobile Magenta 55+ and Magenta MAX 55+ plans include unlimited talk, text, and smartphone data on our network-with taxes and fees included-up to 40GB of 4G LTE mobile hotspot data, Netflix on Us, Gogo in-flight Wi-Fi, 2G international travel data, and more.
What services does T-Mobile provide?
T-Mobile offers mobile Broadband Internet Access Services for smartphones, basic phones, tablets, netbooks, USB modems, mobile hotspot devices and other wireless devices over our 2G, 3G, 4G, and 5G broadband networks.
How much is the activation fee for T-Mobile?
The fee reportedly applies to users who buy an unlocked phone from a supplier other than AT&T and activate it on their accounts. Sprint's activation fee ranges as high as $30 per device; T-Mobile doesn't charge an activation fee but instead requires a $20 "SIM starter kit" for new phone purchases.
What is federal government affordable connectivity program?
The Affordable Connectivity Program is an FCC benefit program that helps ensure that households can afford the broadband they need for work, school, healthcare and more.
What is T-Mobile's cheapest plan?
$10 per month plus tax, the lowest price smartphone plan ever from the Un-carrier, that includes 1000 minutes of talk, 1000 texts and 1GB of high-speed smartphone data.
How much is T-Mobile Best Unlimited Everything monthly plan?
$85 a monthT-Mobile's truly unlimited plan costs $85 a month or $200 for four lines.
How good is T-Mobile coverage?
T-Mobile offers 62% nationwide coverage, while Verizon offers 70%, AT&T offers 68%, and Sprint offers 30%. Since T-Mobile's coverage area is 6% smaller than AT&T's, T-Mobile wins the award for third-best coverage in the nation amongst the Big Four networks.
Is switching from Verizon to T-Mobile worth it?
When should you pick Verizon or T-Mobile? Budgeters: Pick T-Mobile. T-Mobile offers cheaper unlimited plans than Verizon at every tier of service. If you're looking for a non-unlimited data plan, then Verizon is actually better (we would also recommend these plans).
How can I avoid AT&T activation fee?
To get this done, first, you need to reach out to the AT&T customer representative. Talk to them about getting your activation fee waived. Though there is no guarantee you'll get the fee waived entirely, there is a possibility of getting a 50% reduction in the fee you're expected to pay.
How do I get Biden's free internet?
“High-speed internet is not a luxury any longer. It's a necessity,” President Joe Biden remarked. You can go to getinternet.gov to see if you qualify. Those who receive federal programs like SNAP, WIC, free and reduced lunch, medicaid and others qualify.
Whats the difference between lifeline and ACP?
Lifeline is the FCC's permanent program to support affordable access to essential communications services such as broadband Internet access. The ACP is a new program designed to provide additional support to make broadband more affordable for certain low-income households.
When did affordable connectivity program start?
Established Program as of April 1, 2020.
What is telehealth in healthcare?
Telehealth is the broad scope of care that includes telemedicine. Telemedicine includes clinical services. Whereas telehealth consists of both clinical and non-clinical services. For example, doctor training and administrative meetings would fall under telehealth.
What is the 2017 Telehealth Parity Act?
Also, the 2017 Act initiated remote patient-monitoring for those with chronic conditions. Two years earlier, Congress introduced The Medicare Telehealth Parity Act of 2015.
Will Medicare expand telehealth services in 2021?
Updated on April 6, 2021. Medicare continues to expand telemedicine and telehealth services. As virtual care becomes more necessary, doctors and patients look for Medicare to cover services. Today, telemedicine and Medicare benefits continue to expand. Part B includes more telehealth services than ever before.
Is telemedicine a virtual follow up?
And, a virtual follow up doctor’s visit would be telemedicine. To make things more complicated, the World Health Organization uses the term “ telematics ” to describe health activities that take place via communication technology. Telematics is both telemedicine and telehealth. So, all telemedicine is telehealth.
Can Medicare reimburse you for telemedicine?
Reimbursement from Medicare is only for live telemedicine. You must have a real-time video chat with your doctor. The goal is to mirror an in-person visit as close as possible. Live telemedicine is like an office, except its not face-to-face. Two states within the U.S. have different guidelines.
Can telehealth replace in-person care?
While telehealth can’t fully replace in-person care, it does compliment care by increasing access. During the Pandemic, Trump began making telehealth available to those on Medicare. Well, he is making this access permanent. This rule would also reduce clinician burden while giving convenient doctor access to those in rural areas.
Does Medicare cover telemedicine?
Medicare only reimburses telemedicine that takes place via live videoconference. Current telemedicine has coverage through Part B. Also, the location during the time of service must be in a patient’s home or an allowable facility. There are no location restrictions for doctors.
What services does Medicare provide through telehealth?
Medicare beneficiaries will be able to receive a specific set of services through telehealth including evaluation and management visits ( common office visits), mental health counseling and preventive health screenings.
What is telehealth for Medicare?
Under President Trump’s leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. These policy changes build on the regulatory flexibilities granted under the President’s emergency declaration. CMS is expanding this benefit on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans – particularly those at high-risk of complications from the virus that causes the disease COVID-19 – are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus.
How long does Medicare bill for evaluation?
Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes: 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes.
When will Medicare start paying for telehealth?
Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances.
Does Medicare cover telehealth visits?
The Medicare coinsurance and deductible would generally apply to these services. However, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
note
Medicare law no longer limits how much it pays for your medically necessary outpatient therapy services in one calendar year.
note
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like:
note
Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs. Ask questions so you understand why your doctor is recommending certain services and whether Medicare will pay for them.
What is Medicare marketing guidelines?
The Medicare Marketing Guidelines (MMG) implement the Centers for Medicare & Medicaid Services’ (CMS) marketing requirements and related provisions of the Medicare Advantage (MA, MA-PD ) (also referred to as Plan), Medicare Prescription Drug Plan (PDP) (also referred to as Part D Sponsor), and except where otherwise specified, Section 1876 cost plans (also referred to as Plan) rules, (i.e., Title 42 of the Code of Federal Regulations, Parts 422, 423, and 417). These requirements also apply to Medicare-Medicaid Plans (MMPs), except as modified or clarified in state-specific marketing guidance for each state’s demonstration. State-specific guidance is considered an addendum to the MMG. State-specific marketing guidance for MMPs will be posted to http://www.cms.gov/Medicare-
What is co-branding in Medicare?
Co-branding is defined as a relationship between two or more separate legal entities, one of which is an organization that sponsors a Medicare plan. Co-branding is when a Plan/Part D Sponsor displays the name(s) or brand(s) of the co-branding entity or entities on its marketing materials to signify a business arrangement. Co-branding arrangements allow a Plan/Part D Sponsor and its co-branding partner(s) to promote enrollment in the plan. Co-branding relationships are entered into independent of the contract that the Plan/Part D Sponsor has with CMS.
What is a third party marketing organization?
Third-party marketing organizations are entities such as a Field Marketing Organization (FMO), General Agent (GA), or similar type of organization that has been retained to sell or promote a Plan’s/Part D Sponsor’s Medicare products on the Plan’s/Part D Sponsor’s behalf either directly or through sales agents or a combination of both.
What is a script in Medicare?
Informational scripts are designed to respond to beneficiary questions and requests and provide objective information about a plan or the Medicare program. Sales and enrollment scripts are intended to steer a beneficiary towards a plan or limited number of plans, or to enroll a beneficiary into a plan.
What is an educational event for Medicare?
Educational events are designed to inform Medicare beneficiaries about Medicare Advantage, Prescription Drug or other Medicare programs and do not include marketing (i.e., the event sponsor does not steer, or attempt to steer, potential enrollees toward a specific plan or limited number of plans).
What is a non-benefit/non-health service provider?
Third parties that provide non-benefit/non-health services (“Non-benefit/non-health service providing third party entities”) are organizations or individuals that supply non-benefit related information to Medicare beneficiaries or a Plan’s/Part D Sponsor’s membership, which is paid for by the Plan/Part D Sponsor or the non-benefit/non-health service-providing third-party entity.
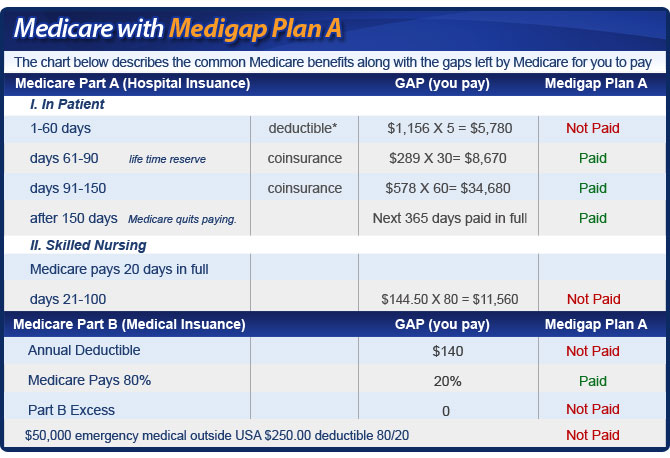
Can you use prior year Medicare premiums?
Plans may use the prior year’s Medicare premium and deductible amounts instead of waiting for CMS to release the upcoming year’s amounts. Plans that apply the Medicare-defined cost-sharing for Inpatient Hospital Care, and Skilled Nursing Facility may also use the prior year’s Medicare cost-sharing amounts.
