The “allowed amount” is one medical insurer pays which is not necessarily to the exact fee practice set the fee. This is like what medical insurers typically pay the allowed charge or the usual, customary, and reasonable fee for a product or service within the specific section of the country.
What is the “allowable amount” for medical insurance?
Durable Medical Equipment — Reimbursement for durable medical equipment and for which billed charges: (a) Are $100.00 or less shall be limited to 80% of billed charges; (b) Exceed $100.00 shall be reimbursed at a maximum amount of the supplier or manufacturer’s invoice amount, plus the lesser of 15% of invoice amount.
What is the billed amount in medical billing?
When you see her for an office visit, her bill will show $150, but the allowed amount will only be $110. She won't get paid the other $40, because it's above the allowed amount. The portion of the $110 allowed amount that you have to pay will depend on the terms of your health plan.
What is the maximum reimbursement for a procedure?
The “allowed amount” is one medical insurer pays which is not necessarily to the exact fee practice set the fee. This is like what medical insurers typically pay the allowed charge or the usual, customary, and reasonable fee for a product or …
What is not included in the Medicare allowable amount?
Feb 19, 2021 · Based on the above costs, the health clinic would be allowed by Medicare to charge $350 total for the services and items provided.

What is allowable amount in medical billing?
The maximum amount a plan will pay for a covered health care service. May also be called “eligible expense,” “payment allowance,” or “negotiated rate.” If your provider charges more than the plan's allowed amount, you may have to pay the difference. ( See Balance Billing)
What is the difference between billed amount and allowed amount?
Billed charge – The charge submitted to the agency by the provider. Allowed charges – The total billed charges for allowable services.Sep 3, 2015
What is the allowed amount listed on an EOB?
Allowed Amount: maximum allowed charge as determined by your benefit plan after subtracting Charges Not Covered and the Provider Discount from the Amount Billed. 25. Deductible Amount: the amount of allowed charges that apply to your plan deductible that must be paid before benefits are payable. 26.
What is allowable amount?
The allowable amount (also referred to as allowable charge, approved charge, eligible expense) is the dollar amount that is typically considered payment-in-full by an insurance company and an associated network of healthcare providers.Dec 15, 2017
How is billed amount calculated in medical billing?
Amount Billed – The full amount billed by your provider to your health plan. Amount Paid by Your Health Plan – The portion of the charges eligible for benefits minus your copay, deductible, coinsurance, network discount, and amount paid by another source up to the billed amount.Sep 19, 2018
What does 80% of billed charges mean?
Coinsurance is a percentage of the health care bill that you pay. For example, you pay 20% and your insurance company pays 80%. Your out-of-pocket cost is based on the total amount that your insurance has allowed for the visit, NOT on the hospital charges.
What are excluded charges on EOB?
1. EXCLUDED CHARGES Charges not eligible, which could be a discount written off by the provider, or a charge you are responsible for paying. 2. CO-PAY The amount you are responsible for paying a PPO provider when a service is rendered.
How do you find the allowed amount?
If you used a provider that's in-network with your health plan, the allowed amount is the discounted price your managed care health plan negotiated in advance for that service. Usually, an in-network provider will bill more than the allowed amount, but he or she will only get paid the allowed amount.Feb 17, 2022
What is EOB 2021?
Updated on April 17, 2021. When you run across the term allowed amount on your health insurance explanation of benefits (EOB), it can cause some confusion. It’s the total amount your health insurance company thinks your healthcare provider should be paid for the care he or she provided. The allowed amount is handled differently if you use an ...
Do you have to pay out of network deductible?
You’ll pay any copay, coinsurance, or out-of-network deductible due; your health insurer will pay the rest of the allowed amount (again, that's assuming your plan includes out-of-network coverage; most HMO and EPO plans do not, meaning that you'd have to pay the entire bill yourself if you see an out-of-network provider).
What is balance billing?
This is called balance billing and it can cost you a lot. (In some circumstances, the balance bill comes as a surprise to the patient, because they were using an in-network hospital and didn't realize that one or more of the physicians (or other healthcare providers) who provided treatment was actually out-of-network.
What is fee in healthcare?
A fee is the price a healthcare provider charges for a product or service. This is similar to each product like electronic item comes with price. Each practice calculates the fee based on the Medicare allowed amount for that year and that area.
What is Medicare approved amount?
Medicare approved amount – In Original Medicare, this is the amount a doctor or supplier who accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is an allowed amount?
The “allowed amount” is one medical insurer pays which is not necessarily to the exact fee practice set the fee. This is like what medical insurers typically pay the allowed charge or the usual, customary, and reasonable fee for a product or service within the specific section of the country.
What is a fee schedule?
These fee schedules determine the allowed amount. A Fee Schedule is a list of reimbursement amount for each procedure. These vary according to various localities. This allowed amount is the maximum that a carrier will pay for a particular procedure.
What does UCR mean in medical terms?
UCR (usual, customary and reasonable) – The amount paid for a medical service in a geographic area based on what providers in the area usually charge for the same or similar medical service. The UCR amount sometimes is used to determine the allowed amount.
What is Medicare approved amount?
The Medicare-approved amount, or “allowed amount,” is the amount that Medicare reimburses health care providers for the services they deliver. Learn more about the Medicare-approved amount and how it affects your Medicare costs. There’s a lot of terminology for Medicare beneficiaries to learn, and among them is “Medicare-approved amount” ...
How much does Medicare pay for X-rays?
The X-rays may have a Medicare-approved amount of $200. And the brace itself might have a Medicare-approved amount of $50. (Note: these costs are hypothetical and are not based on actual Medicare costs for the services or items mentioned.) Based on the above costs, the health clinic would be allowed by Medicare to charge $350 total for ...
What does Medicare cover?
The Medicare-approved amount applies mostly to services covered by Medicare Part B, which covers outpatient services like doctor’s appointments, and it also covers durable medical equipment (DME) such as wheelchairs and blood sugar test strips.
What is a participating provider?
Participating provider. A participating provider “accepts Medicare assignment,” meaning they agree to accept the Medicare-approved amount as full payment for their service or item. They bill Medicare using what are called CPT codes .
What is allowable charge?
Allowable charges are available to participating providers to help avoid refund situations. They are for informational purposes and not intended for providers to establish allowable charges. Blue Cross regularly audits our allowable charge schedule to ensure that the allowable charge amounts are accurate.
Does a physician have to inform BCBSKS of the existence of agreements?
The physician agrees to fully and promptly inform BCBSKS of the existence of agreements under which such physician agrees to accept an amount for any and or all services as payment in full which is less than the amount such physician accepts from BCBSKS as payment in full for such services.
What is co-insurance in insurance?
Co-insurance = Allowed amount – Paid amount – Write-off amount. • Deductible: Deductible is the amount the patient has to pay for his health care services, whereas only after the patient meets the deductible the health insurance plan starts its coverage. The patient has to meet the Deductibles every year.
What is 3.06 Medicare?
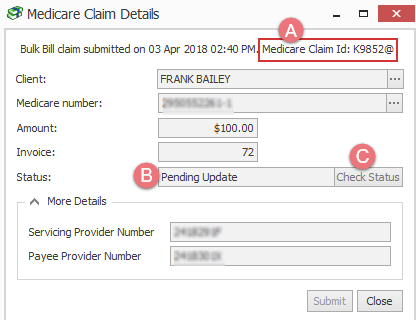
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to make a claim for medicaid or Medicare?
Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program to learn what forms ...
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
Putting It Together
Your full fee ($150) – the adjusted amount ($50 ) = the total amount ($100) [which is the patient responsibility ($20) + insurance reimbursement ($80)].
Denny
Denny has interviewed hundreds of mental health practitioners to better understand their struggles and solutions, all with the goal of making the professional side of behavioral health a little easier, faster, and less expensive.