A conditional payment is a payment made by Medicare for an accident related treatment when:
- Payment is not received by the primary insurer within 120 days (from the date of service or discharge).
- The primary payer (insurer) denies the claim.
- The beneficiary fails to file a proper claim because of physical or mental incapacity.
How does Medicare affect medical billing?
Obamacare’s Affect on Medical Billing and Coding
- Increased Demand for Work. One of the undeniable facts about Obamacare is that more Americans will have health insurance, which means that demand for coding and billing professionals is bound ...
- Cumbersome Government-Related Processing Issues. ...
- Increased Medicare Efficiency. ...
- Job Outlook. ...
Can I refund the billing?
Billing administrators can take ownership of a reservation by selecting it and then selecting Grant access in the window that appears. ... You can cancel, exchange, or refund reservations with certain limitations. For more information, see Self-service exchanges and refunds for Azure Reservations.
Does medical billing pay well?
Top examples of these roles include: Head Of Medical Biller, Medical Billing Consultant, and Remote Biller. Importantly, all of these jobs are paid between $10,309 (20.6%) and $30,019 (59.8%) more than the average Independent Contractor Medical Biller salary of $50,164.
When can conditional primary Medicare benefits be paid?
Conditional Primary Medicare Payments for Group Health Plans (GHPs) Conditional primary Medicare benefits may be paid if the provider, the physician or other supplier, or the beneficiary failed to file proper claim with the GHP (or Large Group Health Plan [LGHP] due to beneficiary physical or mental incapacity.

When would Medicare make a conditional payment to a beneficiary?
MSP provisions allow conditional payments in certain situations when the primary payer has not paid or is not expected to pay within 120 days after receipt of the claim for specific items and/or services. Medicare makes these payments “on condition” that it will be reimbursed if it is shown another payer is primary.
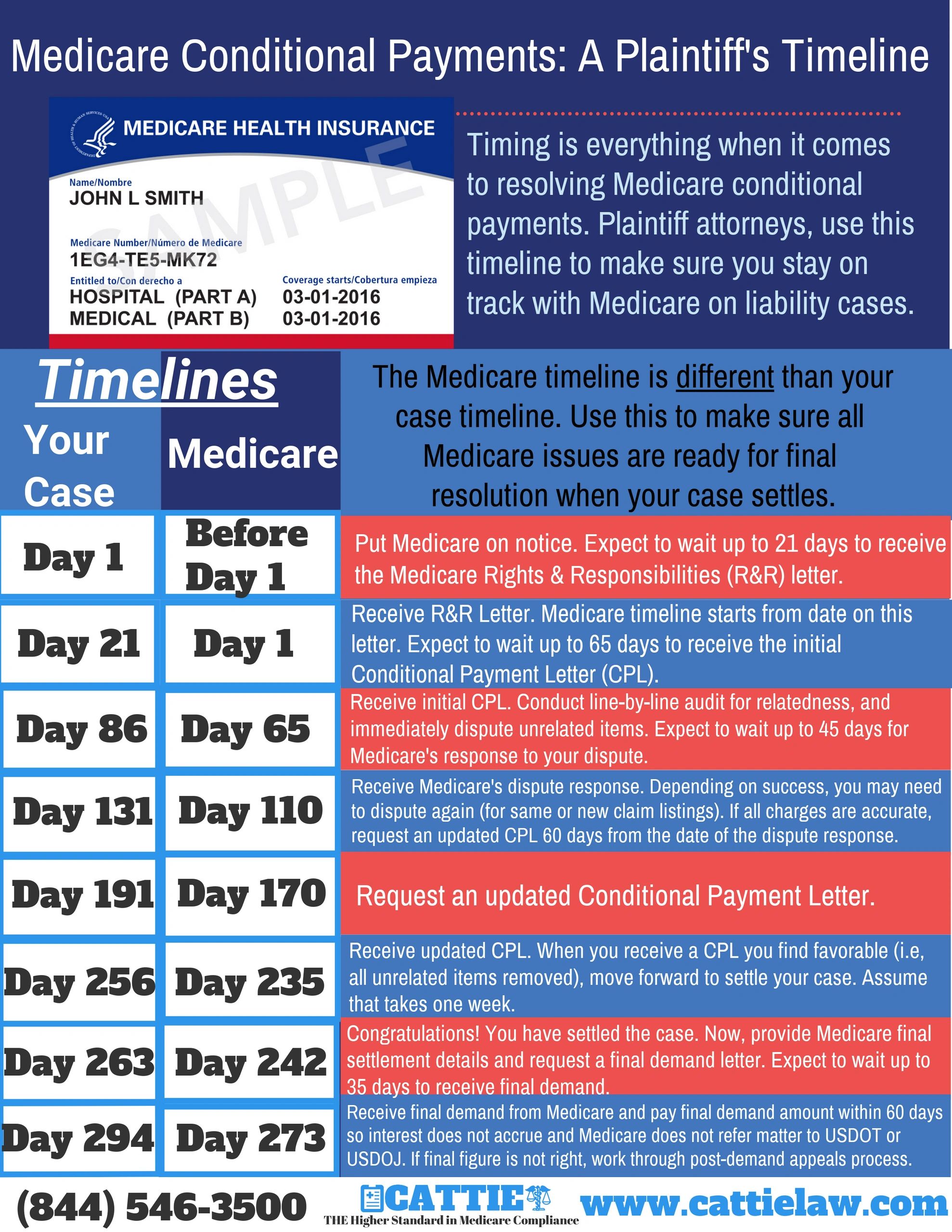
How do I request a Medicare conditional payment?
You can obtain the current conditional payment amount and copies of CPLs from the BCRC or from the Medicare Secondary Payer Recovery Portal (MSPRP). To obtain conditional payment information from the BCRC, call 1-855-798-2627.
Do I have to pay back conditional payments?
If you continue to certify for benefits while we review, you may have to pay back any conditional payments you received if we later find you ineligible.
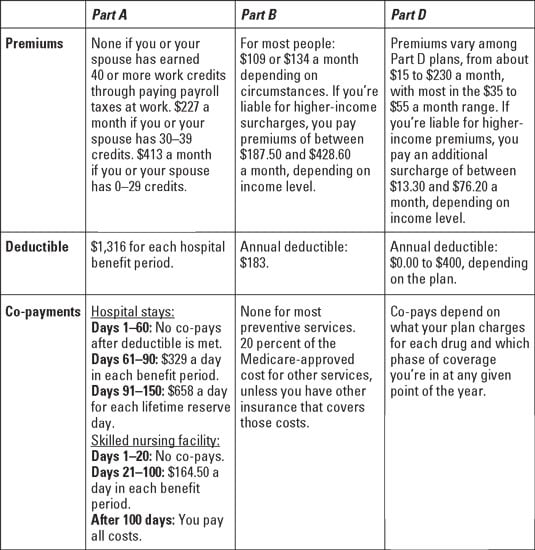
How does Medicare calculate secondary payment?
As secondary payer, Medicare pays the lowest of the following amounts: (1) Excess of actual charge minus the primary payment: $175−120 = $55. (2) Amount Medicare would pay if the services were not covered by a primary payer: . 80 × $125 = $100.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
Why would I be getting a letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
How does Medicare calculate final demand?
Step number two: take the gross settlement amount and subtract the total procurement cost to determine Medicare's final lien demand.
What is notice of conditional payment pending review?
Conversation. Once a conditional payment has been processed, EDD will mail a Notice of Conditional Payment Pending Eligibility Review (DE 5400). If eligible, an Additional Instructions (DE 238) notice will be sent to inform you what weeks were found eligible for benefits.
What is a conditional claim?
Conditional (or “contingent”) claim limitations recite a step or function that is only performed upon the satisfaction of some condition. In a method claim, a conditional limitation might follow the structure, “if A, then B,” reciting that the step B is performed if the condition A occurs.
Does Medicare secondary pay for copays?
Medicare is often the primary payer when working with other insurance plans. A primary payer is the insurer that pays a healthcare bill first. A secondary payer covers remaining costs, such as coinsurances or copayments.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
How do I know if my Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
What is conditional payment?
Conditional payment. A provider may submit a claim to Medicare for conditional payment for services for which another payer is responsible. If payment has not been made or cannot be expected to be made promptly from the other payer, Medicare may make a conditional payment, under some circumstances, subject to Medicare payment rules.
Does Medicare pay workers compensation?
The primary insurer denied the claims in full or when the claim was fully applied to deductible or coinsurance. Medicare will not make conditional payments associated with Workers' Compensation Medicare Set Aside or for an Ongoing Responsibilities for Medicals under auto/no-fault, liability, or workers' compensation.
Does Medicare deny a conditional claim?
Medicare will deny claims submitted for conditional payment when the provider submits the claim to the liability, no-fault, or WC claims and payment is denied if: There is an employer GHP that is primary to Medicare; and. You did not send the claim to the employer GHP first.
Why is Medicare considered a conditional payment?
Medicare may make a conditional payment when there is evidence that payment has not been made or cannot reasonably be expected to be made promptly by workers’ compensation, liability insurance (including self-insurance), or no-fault insurance. These payments are referred to as conditional payments because the money must be repaid to Medicare ...
What is prompt payment for Medicare?
These payments are referred to as conditional payments because the money must be repaid to Medicare when a settlement, judgment, award, or other payment is secured. Prompt or promptly means: Liability insurance (including self-insurance) Payment within 120 days after the earlier of the following: Date a general liability claim is filed ...
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
Why is Medicare conditional?
Medicare makes this conditional payment so you will not have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare when a settlement, judgment, award, or other payment is made.
What is a POR in Medicare?
A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities.
Can you get Medicare demand amount prior to settlement?
Also, if you are settling a liability case, you may be eligible to obtain Medicare’s demand amount prior to settlement or you may be eligible to pay Medicare a flat percentage of the total settlement. Please see the Demand Calculation Options page to determine if your case meets the required guidelines. 7.