Medicare covers services & supplies considered medically necessary to treat a disease or condition. Some of these items include lab tests, surgeries, doctor visits, wheelchairs & walkers What does Medicare cover? What are my coverage choices?
Full Answer
What are the different parts of Medicare?
Medicare covers services & supplies considered medically necessary to treat a disease or condition. Some of these items include lab tests, surgeries, doctor visits, wheelchairs & walkers What does Medicare cover?
What is the resource limit for Medicare&your Handbook?
Real estate ( other than your primary residence ); Bank accounts, including checking, savings and certificates of deposit; Stocks; Bonds, including U.S. Savings Bonds; Mutual funds; Individual Retirement Accounts (IRAs); or Cash at home or anywhere else.
What does medically necessary mean for Medicare?
Have resources (including the income of their spouse if married and living together) within the limits established by statute; and File a low-income subsidy (Extra Help) application or be deemed eligible. Medicare beneficiaries do not need to be enrolled in a …
What is Medicare?
Medicare Advantage is Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage. These “bundled” plans include Part A, Part B, and usually Part D. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
What are considered resources for Medicare?
Definition of resources for Medicare Part D Extra Help. Resources are cash and other assets that an individual owns that could convert to cash to be used for his or her support and maintenance.Jul 15, 2010
How can I avoid paying Medicare premiums?
Those premiums are a burden for many seniors, but here's how you can pay less for them.Sign up for Part B on time. ... Defer income to avoid a premium surcharge. ... Pay your premiums directly from your Social Security benefits. ... Get help from a Medicare Savings Program.Jan 3, 2022
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Be a Medicare beneficiary enrolled in Part A and Part B,Be responsible for paying the Part B premium, and.Live in a service area of a plan that has chosen to participate in this program.Nov 24, 2020
What are the major sources of funding for Medicare?
Funding for Medicare comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest. The different parts of Medicare are funded in varying ways.Mar 16, 2021
Is there really a $16728 Social Security bonus?
The $16,728 Social Security bonus most retirees completely overlook: If you're like most Americans, you're a few years (or more) behind on your retirement savings. But a handful of little-known "Social Security secrets" could help ensure a boost in your retirement income.Dec 9, 2021
Is your Medicare premium deducted from Social Security?
Yes. In fact, Medicare can automatically deduct your Part B premium directly from your Social Security check if you are both enrolled in Part B and collecting Social Security benefits. Most Part B beneficiaries have their premiums deducted directly from their Social Security benefits.Jan 14, 2022
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
How can I increase my Social Security benefits after retirement?
Below are the nine ways to help boost Social Security benefits.Work for 35 Years. ... Wait Until at Least Full Retirement Age. ... Sign Up for Spousal Benefits. ... Receive a Dependent Benefit. ... Monitor Your Earnings. ... Avoid a Tax-Bracket Bump. ... Apply for Survivor Benefits. ... Check for Mistakes.More items...
Why did I get an extra Social Security payment this month 2021?
According to the CMS, the increases are due to rising prices and utilization across the healthcare system, as well as the possibility that Medicare may have to cover high-cost Alzheimer's drugs like Aduhelm.Jan 12, 2022
Which of the following services are covered by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
What are the income limits for Medicare 2024?
5% Inflation AssumptionPart B Premium2022 Coverage (2020 Income)2024 Coverage (2022 Income)Standard * 3.4Single: >= $500,000 Married Filing Jointly: >= $750,000 Married Filing Separately >= $409,000Single: >= $500,000 Married Filing Jointly: >= $750,000 Married Filing Separately >= $397,0005 more rows•Apr 12, 2022
What is the largest third party payer?
MedicareMedicare is the largest third-party payer and is provided by the federal government.
What is Medicare?
Medicare is a federal health insurance program for people 65 years of age or older, certain younger people with disabilities, and people with End-Stage Renal Disease (ESRD)
What are my coverage choices?
Original Medicare (Part A & Part B), Medicare Advantage Plan (Part C), Prescription Drug Plan (Part D), Medicare Supplement Insurance (Medigap)
What does Part B cover?
Medicare Part B generally covers “medically necessary services” & preventive services
What can I expect to pay for Part A and Part B (Original Medicare)?
Usually you will not pay a monthly premium for Part A coverage (Hospital Insurance) if you or your spouse paid Medicare taxes while working.
What does Part C (Medicare Advantage Plan) cover?
Part C is offered by private companies that contract with Medicare to provide you with all of your Part A & Part B benefits. Medicare Advantage Plans must cover all services that Original Medicare (Part A & Part B) covers, except hospice care, and is provided by private insurance companies.
What does Part D (Prescription Drug Plan) cover?
Part D adds prescription drug coverage & is offered by insurance companies and other private companies approved by Medicare. Each Medicare Prescription Drug Plan has a unique list of covered medications. These medications are organized into different “tiers” based on the specific plan with each tier having a different cost.
What does Medicare Supplement Insurance (Medigap) cover?
A Medigap policy is sold by a private company & can help pay some health care costs not covered by Original Medicare (ex: coinsurance, deductibles, medical care when you travel outside the U.S.)
Where to mail Social Security form?
This form should be mailed to Social Security at the address on the enclosed postage-paid envelope: Social Security Administration Wilkes-Barre Data Operations Center P.O. Box 1020 Wilkes-Barre, PA 18767-9910
What is a relative?
For this question, a relative is someone related to you by blood, adoption, or marriage (but not including your spouse). How many relatives live with you and depend on you or your spouse for at least one-half of their financial support?
What is the appeal process for Social Security?
The appeals process enables beneficiaries who disagree with Social Security’s Extra Help determinations to get a new decision by an independent reviewer. The appeals process has just one formal administrative step. Beneficiaries can choose either a hearing by telephone or a case review. Beneficiaries still dissatisfied with Social Security’s final decision can file an action in Federal district court.
Can Social Security data exchange be used to reconcile income?
The information that is available to us via data exchange may not be current. If this question is answered “Yes,” the response can be used to reconcile discrepancies between the alleged income and the income shown in Social Security’s records without contacting the applicant for verification. A decrease in income could affect the eligibility for and amount of a subsidy.
What is Medicare for?
Medicare is the federal health insurance program for: 1 People who are 65 or older 2 Certain younger people with disabilities 3 People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
What is a medicaid supplement?
A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles. Some Medigap policies also cover services that Original Medicare doesn't cover, like medical care when you travel outside the U.S.
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
What percentage of Medicare is coinsurance?
In Original Medicare, this is a percentage (like 20%) of the Medicare approved amount. You have to pay this amount after you pay the deductible for Part A and/or Part B. In a Medicare Prescription Drug Plan, the coinsurance will vary depending on how much you have spent.
How often does Medicare pay deductibles?
For example, in Original Medicare, you pay a new deductible for each benefit period for Part A, and each year for Part B. These amounts can change every year.
When does the AEP take effect?
AEP occurs from [October 15 through December 7] of every year.
What is copayment in Medicare?
A copayment is usually a set amount you pay. For example, this could be $10 or $20 for a doctor’s visit or prescription.
How many days does Medicare pay for a hospital stay?
In Original Medicare, a total of 60 extra days that Medicare will pay for when you are in a hospital more than 90 days during a benefit period. Once these 60 reserve days are used, you do not get any more extra days during your lifetime. For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance.
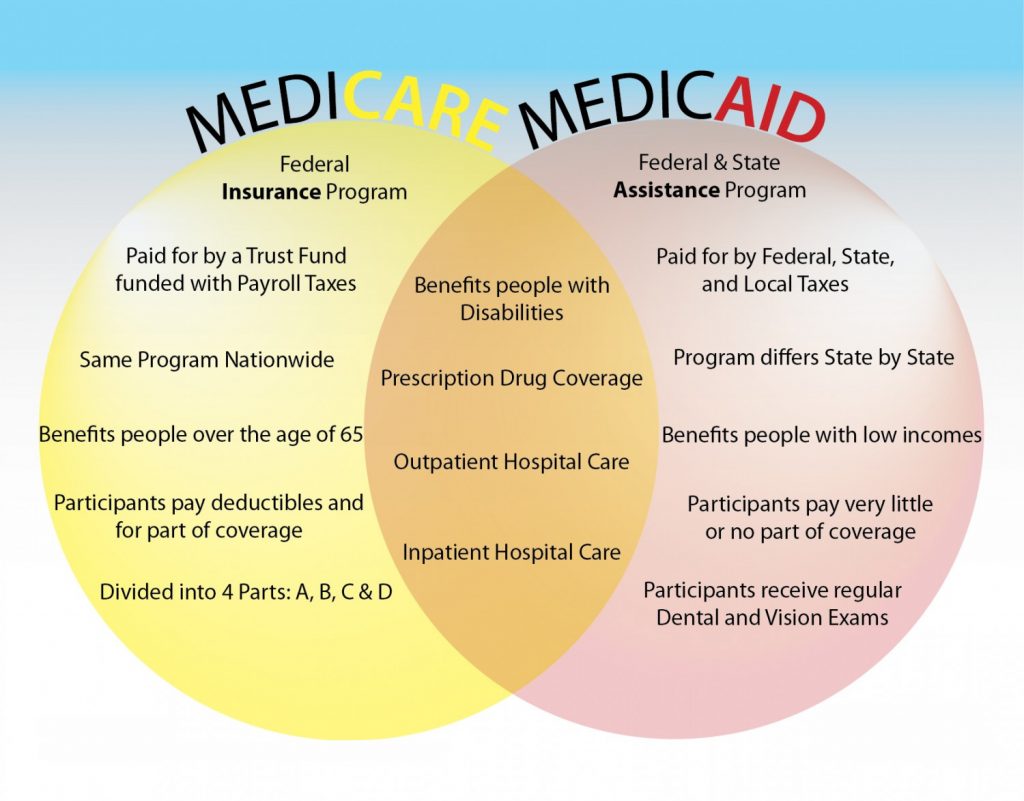
Can you have both Medicare and Medicaid?
Some people qualify for both Medicare and Medicaid (these people are also called “dual eligibles”). If you have Medicare and full Medicaid coverage, most of your health care costs are covered. You have the option of Original Medicare or a Medicare Advantage Plan (like an HMO or PPO).
What is the gap in Medicare coverage?
Also known as the “donut hole,” this is a gap in coverage that occurs when someone with Medicare goes beyond the initial prescription drug coverage limit. When this happens, the person is responsible for more of the cost of prescription drugs until their expenses reach the catastrophic coverage threshold.
What does SLMB cover?
SLMB benefits cover the cost of the monthly Medicare Part B premium. The standard Part B premium in 2021 is $148.50 per month and is required of all Medicare Part B beneficiaries.
How do you qualify for SLMB?
Each state Medicaid program has its own rules concerning qualification.
What other Medicare Savings Programs are there?
SLMB is just one of the available Medicare Savings Programs. Others include:
How do you apply for SLMB?
Contact your state Medicaid program for information and assistance with applying for the SLMB program.
Is there Medicaid assistance for Medicare Advantage beneficiaries?
Individuals who qualify for both Medicare and Medicaid are considered “dual eligible” and may qualify for a certain type of Medicare Advantage plan called a Special Needs Plan. And one particular type of Special Needs Plan is a Dual Eligible Special Needs Plan (D-SNP).
What is Medicare Part A?
Medicare Part A covers medically necessary services and treatment you get in an inpatient setting, including: *Medicare covers nursing care when non-skilled, custodial care (such as help with daily tasks like bathing or eating) isn’t the only care you need. This coverage is generally for a limited period of time.
What is medically necessary?
Get Started. “Medically necessary” is a standard that Medicare uses when deciding whether to cover a health-care service or item. This applies to everything from flu shots and preventive screenings, to kidney dialysis and wheelchairs.
Does Medicare cover cataract surgery?
However, if you get cataract surgery to implant an intraocular lens, Medicare helps cover the cost of corrective lenses (either one pair of eyeglasses or one set of contact lenses). You’ll pay 20% of the Medicare-approved amount, and the Medicare Part B deductible applies.
What is advance coverage decision?
If you aren’t sure whether a service or item you may need is covered, you can ask Medicare for an advance coverage decision, which is a document from Medicare letting you know whether a particular service or equipment is covered and what your costs may be.
Does Medicare Advantage cover hospice?
By law, Medicare Advantage plans are required to cover at least the same level of health coverage as Original Medicare, including all medically necessary services under Medicare Part A and Part B (with the exception of hospice care). However, individual Medicare Advantage plans also have the flexibility to cover extra services ...
Can you appeal a denied claim on Medicare?
If you’ve already received a service or equipment and Medicare has denied your claim, you have a right to appeal the decision. The appeals process works differently depending on whether you have Original Medicare or a Medicare Advantage plan. You also have a right to ask for an expedited appeal if waiting for a standard decision could endanger your health. For more information, take a look at this online publication on the Medicare appeals process here.
Does Medicare cover dental care?
In some cases, Medicare may cover a service it normally doesn’t cover if it’s related to a covered procedure. For example, while most routine dental care isn’t normally covered, Medicare will cover a dental exam that is part of a pre-op exam if you’re about to get a kidney transplant or heart valve replacement.
What does Medicare cover?
What might this mean for you as a beneficiary? According to the above definition, Medicare covers services that it views as medically necessary to diagnose or treat your health condition. Services must also meet criteria supplied by national coverage determinations and local coverage determinations.
What is medically necessary?
According to Medicare.gov, “medically necessary” is defined as “health-care services or supplies needed to prevent, diagnose, or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”. In any of those circumstances, if your condition produces debilitating symptoms or side effects, ...
Is glaucoma covered by Medicare?
Glaucoma screenings are covered for all beneficiaries with Medicare Part B who have a high risk for glaucoma. Factors that put you at high risk for glaucoma include having diabetes; having a family history of glaucoma; being African American and age 50 or older; and being Hispanic American and age 65 or older.
Does Medicare cover mammograms?
Intensive behavioral therapy for obesity is covered for all beneficiaries with Medicare Part B who have a body mass index (BMI) of 30 or higher. Mammograms are covered for women with Medicare Part B who are 40 or older; one baseline mammogram is covered for women with Part B between 35 to 39 years old.
Is prostate cancer covered by Medicare?
Prostate cancer screenings are covered for all men with Medicare Part B over age 50, starting the day after their 50th birthday. Screenings for depression. Screenings and behavioral counseling interventions in primary care to reduce alcohol misuse.
Is Medicare Part B covered by Medicare?
Services that are not considered medically necessary. Services that aren’t deemed medically necessary are not covered by Original Medicare , Part A and Part B. It’s possible that some of these services may be covered by a Medicare Advantage plan, but that depends on your specific plan benefits. Non-medically necessary services according ...
What is the top number of systolic pressure?
The top number (135 in this example) is the systolic pressure, measured as your heart beats and pushes blood through your veins, notes the National Institutes of Health. The bottom number (86 in this example) is the diastolic pressure, measured as your heart rests between beats.
What is the normal blood pressure range?
What is the standard range for blood pressure? The National Institutes of Health (NIH) reports that normal blood pressure is 120/80 or lower (these figures are described below). It wasn’t until your blood pressure reached 140/90 that it was considered high blood pressure, or hypertension.
What is stage 2 hypertension?
Stage 2 hypertension (high blood pressure): 140 or higher / 90 or higher. If your blood pressure reaches hypertensive crisis level, it means you need a doctor to check whether you have any organ damage or need changes to your medications, according to the ACC.
Can blood pressure change?
Now that researchers have changed the number that’s considered high blood pressure, it might mean that you have high blood pressure now, even if your blood pressure numbers put you in “normal” range last time you saw your doctor. Of course, notes the National Institutes of Health (NIH), your blood pressure numbers can change many times ...