Does Medicaid have copay or cost sharing?
State Medicaid agencies have legal obligations to pay Medicare cost-sharing for most "dual eligibles" – Medicare beneficiaries who are also eligible for some level of Medicaid assistance. Further, most dual eligibles are excused, by law, from paying Medicare cost-sharing, and providers are prohibited from charging them. [1]
What is the monthly cost for Medicare?
The standard monthly premium for Medicare Part B is $148.50 per month in 2021. Some Medicare beneficiaries may pay more or less per month for their Part B coverage. The Part B premium is based on your reported income from two years ago (2019).
What is happening to Medicare Cost plans?
- Yes, I've already comparison shopped and selected the best option.
- No, net yet, but I’m confident that I’ll pick the best plan before Dec. 7.
- No, I picked a good plan in the past and I’m happy to just let it renew.
- No, I feel overwhelmed by the process of trying to pick a different plan.
What does share of cost mean for Medicaid?
Your share-of-cost is the amount of healthcare expenses you must incur before Medicaid coverage kicks in for the month. You start each month without Medicaid health insurance coverage.
How does cost-sharing work in Medicare?
An example of the cost-sharing payment system allowed by the BBA is as follows: If Medicare allows $100 for a physician visit (and thus pays $80, or 80%), under full payment of cost sharing, the state would pay the full $20 remaining.
What is an example of cost-sharing?
Example: You have a copay. Your doctor's visit costs $100. You only pay $20 each visit. Insurance pays the remaining $80.
How does cost-sharing work?
Cost sharing means that you will not generally be paying for all of your covered medical expenses on your own, and that your individual health insurance plan may help you with these incurred expenses.
Do Medicare beneficiaries have cost-sharing?
The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries.
What are the benefits of cost-sharing?
Plans with lower cost-sharing (ie, lower deductibles, copayments, and total out-of-pocket costs when you need medical care) tend to have higher premiums, whereas plans with higher cost-sharing tend to have lower premiums. Cost-sharing reduces premiums (because it saves your health insurance company money) in two ways.
Is cost share the same as copay?
What is a co-payment or co-pay? A co-‐payment (also called a “co-‐pay”) is a form of cost-‐sharing. It is a set amount of money you will pay for a service ($3, $15, $40 etc). The amount is the same no matter how much the doctor or hospital charges for the service.
Who pays for cost-sharing reductions?
Who is eligible for cost-sharing reductions? Individuals and families with incomes up to 250 percent of the poverty line are eligible for cost-sharing reductions if they are eligible for a premium tax credit and purchase a silver plan through the Health Insurance Marketplace in their state.
Do you have to pay back cost-sharing reduction?
If I underestimate my income and end up earning more than 250 percent of the federal poverty level next year, will I have to pay back the cost-sharing subsidies? No. Unlike premium tax credits, which are reconciled each year based on the income you actually earned, cost-sharing reductions are not reconciled. (42 U.S.C.
Is health sharing a good idea?
Healthcare sharing ministries provide a viable option for those who are looking for an alternative to shopping on the ACA Marketplace. Members of these ministries can encourage one another through personal notes of encouragement, which can foster a sense of community and family between each other.
How much do Medicare beneficiaries spend out-of-pocket on health care?
Medicare Beneficiaries' Spending for Health Care People covered by traditional Medicare paid an average of $6,168 for health care in 2018. They spent almost half of that money (47 percent) on Medicare or supplemental insurance premiums.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What is the maximum out-of-pocket for Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
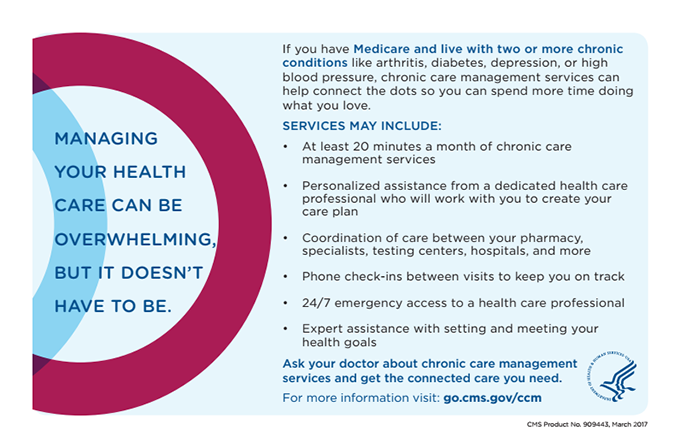
Medicare Cost Sharing Definitions
Medicare cost sharing may seem more complex than other forms of insurance because Medicare has four different parts, and each one covers something different. Two of those parts are public (Parts A and B), and two are private (Parts C and D).
Medicare Part A Cost Sharing
Medicare Part A is hospital insurance and it covers inpatient procedures, hospice care, and skilled nursing facilities. Many Medicare eligibles don’t pay a monthly premium for Part A. If you don’t meet the “premium-free Part A” requirements, you may pay up to $458 per month in 2020.
Medicare Part B Cost Sharing
Medicare Part B is medical insurance, and it helps pay for outpatient medical services such as doctor’s appointments, emergency medical transportation, outpatient therapy, and durable medical equipment (DME).
Medicare Part C Cost Sharing
Medicare Advantage (MA or Part C) are private plans that can cover additional benefits such as prescription drugs, dental, hearing, vision, and fitness classes. You must be enrolled in both Part A and Part B before you can enroll in a MA plan.
Medicare Part D Cost Sharing
Medicare Part D is prescription drug coverage. You may have to pay a monthly premium, for which the average cost was $33.19 nationwide in 2019.
Medicare Supplement Cost Sharing
Medicare Supplement (Medigap) plans have a different cost sharing structure than MA plans. Medigap plans have eight standardized coverage levels*. In 2020 there are eight different coverage levels:
We Can Help You Navigate Medicare Cost Sharing
Cost sharing with Medicare may seem complicated, and a licensed agent with Medicare Plan Finder can help you determine what you need. Our agents are highly trained, and they can find the Medicare Advantage, Medicare Supplement, and/or Medicare Part D plans in your area.
How much does Medicare pay for a physician visit?
For example, if Medicare allows $100 for a visit to a physician's office, Medicare will pay 80% of that amount, or $80. If the state Medicaid program pays only $70 for the same service, it would make no payment for that service delivered to a QMB. The authority (but not a requirement) for states to limit their QMB cost-sharing obligations ...
What is the law that states that Medicare is paid in full?
Two sections of the law require this result. The first is 42 U.S.C. § 1396a (n) (3) (A), which says that the amount paid by Medicare and the amount, if any, paid by the state shall be considered payment in full.
What is a QMB in Medicare?
Qualified Medicare Beneficiaries (QMBs) are people with Medicare who have incomes at or below 100% of the Federal Poverty Level , or a higher level set by their state, and very few resources. [1] . The QMB benefit is administered by State Medicaid programs. QMBs can be eligible for Medicare cost-sharing protections only, ...
Does Medicare have a cross-over billing agreement?
The MLN piece reminds providers that most states have "cross-over" billing agreements with Medicare whereby any Medicare claim for a person also receiving Medicaid is sent to the state for the state's share of payment.
Can you pay Medicare with QMB?
People with QMB are excused, by law, from paying Medicare cost-sharing, and providers are prohibited from charging them. [2] . All cost-sharing (premiums, deductibles, co-insurance and copayments) related to Parts A and B is excused, meaning that the individual has no liability . The state has responsibility for these payments for QMBs regardless ...
Can advocates work with states to increase the state's cost sharing payment to the full Medicare rate?
Advocates can work with their states to increase the state's cost-sharing payment to the full Medicare rate. Perhaps it is time for Congress to revisit the question of whether limited cost-sharing payments adversely impact beneficiaries.
Do states have to pay Medicare premiums?
States can, but are not required to, pay premiums for Medicare Advantage plans' basic and supplemental benefits; states do have responsibility for MA co-payments for Part A and B services. The State's responsibility, however, is limited.
What is Medicare Cost-Sharing?
When you use Medicare, you share the cost of your care by paying premiums, deductibles, copayments, co-insurance, and out-of-pocket maximums. If you receive a paycheck, part of your check will be set aside for Medicare. You pay for the program when you work and pay again when you use it.
We Explain Cost-Sharing Terms
Cost-Sharing includes your cost of premiums, deductibles, copayments, co-insurance, and out-of-pocket maximums. You share the cost of your medical services with your insurance company.
What is cost sharing in Medicaid?
Cost Sharing. States have the option to charge premiums and to establish out of pocket spending (cost sharing) requirements for Medicaid enrollees. Out of pocket costs may include copayments, coinsurance, deductibles, and other similar charges.
Can you charge out of pocket for coinsurance?
Certain vulnerable groups, such as children and pregnant women, are exempt from most out of pocket costs and copayments and coinsurance cannot be charged for certain services.
Does Medicaid cover out of pocket charges?
Prescription Drugs. Medicaid rules give states the ability to use out of pocket charges to promote the most cost-effective use of prescription drugs. To encourage the use of lower-cost drugs, states may establish different copayments for generic versus brand-name drugs or for drugs included on a preferred drug list.
Can you get higher copayments for emergency services?
States have the option to impose higher copayments when people visit a hospital emergency department for non-emergency services . This copayment is limited to non-emergency services, as emergency services are exempted from all out of pocket charges. For people with incomes above 150% FPL, such copayments may be established up to the state's cost for the service, but certain conditions must be met.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What is cost sharing?
What is cost-sharing? Cost-sharing refers to the patient’s portion of costs for healthcare services covered by their health insurance plan. The patient is responsible to pay cost-sharing amounts out-of-pocket.
How much will Medicare cost share in 2021?
Medicare Advantage plans cannot require members to pay cost-sharing in excess of $7,550 in 2021, although many plans have cost-sharing limits below this (note that the out-of-pocket limits for Medicare Advantage plans do not include the cost of prescription drugs, which are covered separately and have separate — and unlimited — cost-sharing).
What is out of pocket medical insurance?
But under private health insurance or Medicaid, “out-of-pocket costs” generally only refer to cost-sharing incurred when a person has medical claims (even though premiums are also paid out-of-pocket).
Does the ACA cover grandfathered plans?
The ACA’s limits on out-of-pocket costs only applies to in-network services that fall within the umbrella of essential health benefits. And it does not apply to grandmothered or grandfather ed plans, or to plans that aren’t regulated by the ACA at all, such as short-term health insurance.
Is health insurance a cost sharing amount?
Health insurance premiums – the monthly payments you must make to keep your coverage in force, regardless of whether or not you use a healthcare service – are not considered cost-sharing amounts.
Can you be higher on out of pocket limits?
Many plans have out-of-pocket limits below this level, but they cannot be higher. Once your cost-sharing amounts have reached your plan’s maximum out-of-pocket limit for the year, the health insurance plan will pay 100% of your remaining covered costs that year. The ACA’s limits on out-of-pocket costs only applies to in-network services ...
Does Medicare have a cap on cost sharing?
Original Medicare does not have a cap on cost-sharing amounts, although most enrollees have supplemental coverage (from an employer, Medicaid, or a Medigap plan) that covers some or all of their cost-sharing expenses.
What happens if Medicare pays $80?
If the state's payment were $90, the state would pay the difference between Medicare's payment and the state’s payment, or $10.
Can advocates work with states to increase the state's cost sharing payment to the full Medicare rate?
Advocates can work with their states to increase the state’s cost-sharing payment to the full Medicare rate. Perhaps it is time for Congress to revisit the question of whether limited cost-sharing payments adversely impact beneficiaries.
Does Medicaid cover dual eligibles?
State Medicaid agencies have legal obligations to pay Medicare cost -sharing for most " dual eligibles" – Medicare beneficiaries who are also eligible for some level of Medicaid assistance . Further, most dual eligibles are excused, by law, from paying Medicare cost-sharing, and providers are prohibited from charging them. [1] .
Is dual eligible Medicare?
But the particulars are complex in traditional Medicare and become even more complex when a dual eligible is enrolled in a Medicare Advantage (MA) plan. [2] It may be helpful to think of dual eligibles in two categories: those who are Qualified Medicare Beneficiaries (QMBs) (with or without full Medicaid coverage) and those who receive full ...
Does Medicaid require cost sharing?
In addition to this obligation, the Medicaid statute authorizes – but does not require – states to pay providers Medicare cost-sharing for at least some non-QMB dual eligibles. [5] . It appears from the language of the statute that such payment could include cost-sharing for services not covered in the state Medicaid program.
Can you pay premiums for MA plans?
States can, but are not required to, pay premiums for MA plans' basic and supplemental benefits. The "Balance Billing" Q & A referenced above answers the question, "May a provider bill a QMB for either the balance of the Medicare rate or the provider's customary charges for Part A or B services?".
Does Medicare pay for a claim?
In the traditional Medicare program, a provider files a claim with Medicare, then Medicare, after it has paid its portion, sends the claim to Medicaid for payment of the beneficiary’s cost-sharing. However, if a beneficiary is in an MA plan, the provider does not bill Medicare; the provider bills the plan or receives a capitated payment from ...