
A coverage determination is the first decision made by your Medicare drug plan (not the pharmacy) about your Benefits , including these: Whether a certain drug is covered Whether you have met the requirements to get a requested drug How much you pay for a drug Whether to make an exception to a plan rule when you request it
- Whether a certain drug is covered
- Whether you have met the requirements to get a requested drug
- How much you pay for a drug
- Whether to make an exception to a plan rule when you request it
What if Medicare denies coverage?
Understanding a Medicare denial letter
- Reasons for coverage denial. It is beneficial for an individual to understand why they have received a Medicare denial letter. ...
- Different types of denial letter. Medicare issues several types of denial letters. ...
- Appeals. ...
- Levels of appeal. ...
- Additional support. ...
- Summary. ...
What are local coverage determinations?
- What item or service you need
- Why the LCD is incorrect
- Why you’re challenging the LCD
What is the definition of coverage determination?
Coverage Determinations. A coverage determination is any decision made by the Part D plan sponsor regarding: Receipt of, or payment for, a prescription drug that an enrollee believes may be covered; A tiering or formulary exception request (for more information about exceptions, click on the link to "Exceptions" located on the left hand side of ...
What is the Order of benefit determination rules?
The order in which the various Plans that cover you pay a claim is called order of benefit determination or coordination of benefits. It follows strict industry and, in some cases, federal rules. 1. Medicaid and Tricare (military insurance) are always secondary to everything. Tricare used to be called CHAMPUS and some places still call it that.
What does coverage determination by Medicare indicate?
A National Coverage Determination (NCD) is a nationwide determination of whether Medicare will pay for an item or service.
What is determination of coverage?
A coverage determination is a decision about whether a drug prescribed for you will be covered by us and the amount you'll need to pay, if any. If a drug is not covered or there are restrictions or limits on a drug, you may request a coverage determination.
How does national coverage determination work?
National coverage determinations (NCDs) are made through an evidence-based process, with opportunities for public participation. In some cases, CMS' own research is supplemented by an outside technology assessment and/or consultation with the Medicare Evidence Development & Coverage Advisory Committee (MEDCAC).
What does the Medicare national coverage determination manual provide?
A national coverage determination (NCD) is a United States nationwide determination of whether Medicare will pay for an item or service. It is a form of utilization management and forms a medical guideline on treatment.
How is the Medicare approved amount determined?
The Medicare-approved amount is the amount of money that Medicare will pay a health care provider for a medical service or item. After you meet your Medicare Part B deductible ($233 per year in 2022), you will typically pay a percentage of the Medicare-approved amount for services and items covered by Medicare Part B.
How long does it take to get a local Coverage Determination?
The LCD will become effective a minimum of 45 days after the final LCD is published on the MCD. Unless extended by the MAC issuing the LCD, the effective date of the LCD is the 46thcalendar day after the notice period began.
What are national and local coverage determinations?
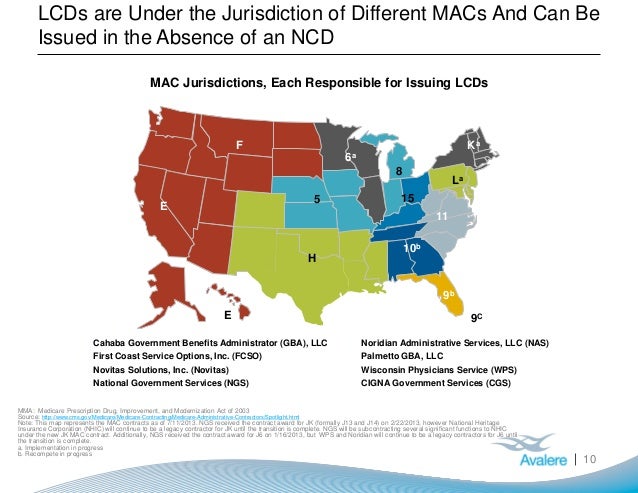
What is an LCD? An LCD, as defined in §1869(f)(2)(B) of the Social Security Act (SSA), is a determination by a Medicare Administrative Contractor (MAC) regarding whether or not a particular item or service is covered on a contractor–wide basis in accordance with section 1862(a)(1)(A) of the Act.
What is the difference between LCD and NCD for Medicare?
When a contractor or fiscal intermediary makes a ruling as to whether a service or item can be reimbursed, it is known as a local coverage determination (LCD). When CMS makes a decision in response to a direct request as to whether a service or item may be covered, it's known as a national coverage determination (NCD).
What is LCD in medical billing?
An LCD is a determination by a Medicare Administrative Contractor (MAC) whether to cover a particular service on a. Coverage criteria is defined within each LCD , including: lists of CPT /HCPCs codes, codes for which the service is covered or considered not reasonable and necessary.
What is the purpose of national coverage determinations quizlet?
What is the purpose of National Coverage Determinations? To explain CMS policies on when Medicare will pay for items or services.
What does NCD mean in healthcare?
Noncommunicable diseases (NCDs), also known as chronic diseases, tend to be of long duration and are the result of a combination of genetic, physiological, environmental and behavioural factors.
What is CMS approval?
CMS approvals are issued at a local level by the Medicare Administrative Contractor (MAC) or are reviewed an approved through a centralized process by CMS. Studies approved through the centralized process are listed here.
What is a coverage determination?
A coverage determination is the decision process used to receive access to medications or medical procedures that may not usually covered by Medicare.
What is the process of filing for a medical coverage determination?
The process of filing for a coverage determination usually involves filling out some forms and allowing your physician or specialist to review them.
Why is Medicare denial of coverage?
One of the most common reasons for denial of a coverage determination is if alternative treatment options exist. If they do, especially if they are covered by Medicare, you will almost always have to try these methods before your coverage determination request will be considered.
What happens if you get denied coverage?
If a request is denied in part, you may only receive coverage for some of the items in your request. If your request is denied and you are also denied on appeal, you will be left with few options to have your case heard again.
Is cosmetic surgery covered by Medicare?
For example, while things like cosmetic surgery are not covered by original Medicare, a surgical procedure that is usually considered cosmetic may be eligible for coverage after a coverage determination finds that the procedure is required for sustained health.
Does Medicare cover prescription drugs?
Medicare recipients often wonder if a specific prescription drug is covered or if a particular medical procedure will be paid for by their Medicare plans. In order to get these answers, you can simply review your plan’s formulary for prescription medications or review the coverage options under Medicare Part A and Part B.
What is a Part D coverage determination?
A coverage determination is any decision made by the Part D plan sponsor regarding: Receipt of, or payment for, a prescription drug that an enrollee believes may be covered;
How to request a standard or expedited coverage determination?
An enrollee, an enrollee's prescriber, or an enrollee's representative may request a standard or expedited coverage determination by filing a request with the plan sponsor. Standard or expedited requests for benefits may be made verbally or in writing. Standard requests for payment must be made in writing, unless the plan sponsor accepts requests ...
What is a prior authorization?
A requirement that an enrollee try another drug before the plan sponsor will pay for the requested drug and the enrollee disagrees with the requirement; or. A decision whether an enrollee has, or has not, satisfied a prior authorization or other utilization management requirement.
What Is the Medicare Determination Process?
Original Medicare is meant to cover items, treatments and services that are medically necessary. A nine-month process determines the final decision. The first phase of the process lasts six months.
National Coverage Determinations (NCDs)
A national coverage determination (NCD) decides coverage for a treatment or service that applies to the entire nation. An NCD is also determined through a nine-month process.
What is a local coverage determination?
What’s a "Local Coverage Determination" (LCD)? LCDs are decisions made by a Medicare Administrative Contractor (MAC) whether to cover a particular item or service in a MAC’s jurisdiction (region) in accordance with section 1862 (a) (1) (A) of the Social Security Act. MACs are Medicare contractors that develop LCDs and process Medicare claims.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. , or both. You need the item (s) or service (s) determined not covered by the LCD.
What is MAC in Medicare?
MACs are Medicare contractors that develop LCDs and process Medicare claims. The MAC’s decision is based on whether the service or item is considered reasonable and necessary.
Acupuncture for Chronic Low Back Pain
CMS will cover acupuncture for chronic low back pain under section 1862 (a) (1) (A) of the Social Security Act. Up to 12 visits in 90 days are covered for Medicare beneficiaries under the following circumstances:
Decision Memo for Chimeric Antigen Receptor (CAR) T-cell Therapy for Cancers
The Centers for Medicare & Medicaid Services (CMS) covers autologous treatment for cancer with T-cells expressing at least one chimeric antigen receptor (CAR) when administered at healthcare facilities enrolled in the FDA risk evaluation and mitigation strategies (REMS) and used for a medically accepted indication as defined at Social Security Act section 1861 (t) (2) i.e., is used for either an FDA-approved indication (according to the FDA-approved label for that product), or for other uses when the product has been FDA-approved and the use is supported in one or more CMS-approved compendia..
Vagus Nerve Stimulation (VNS) for Treatment Resistant Depression (TRD) (CAG-00313R2)
CMS is finalizing changes to the vagus nerve stimulation (VNS) NCD (160.18) for VNS for treatment resistant depression (TRD) that will expand Medicare coverage. The scope of this reconsideration is limited to VNS for TRD.
Magnetic Resonance Imaging (MRI) (CAG-00399R4)
CMS determined the evidence is sufficient to conclude that magnetic resonance imaging (MRI) for Medicare beneficiaries with an implanted pacemaker (PM), implantable cardioverter defibrillator (ICD), cardiac resynchronization therapy pacemaker (CRT-P), or cardiac resynchronization therapy defibrillator (CRT-D) is reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member under certain circumstances..
Next Generation Sequencing (NGS) for Medicare Beneficiaries with Advanced Cancer (CAG-00450N)
The Centers for Medicare & Medicaid Services (CMS) has determined that Next Generation Sequencing (NGS) as a diagnostic laboratory test is reasonable and necessary and covered nationally, when performed in a CLIA-certified laboratory, when ordered by a treating physician and when all of the qualifying requirements are met.
Implantable Cardioverter Defibrillators
The Centers for Medicare & Medicaid Services (CMS) has determined that the evidence is sufficient to conclude that the use of implantable cardioverter defibrillators (ICDs, also referred to as defibrillators) is reasonable and necessary for the treatment of illness or injury or to improve the functioning of a malformed body member.
Leadless Pacemakers
TCMS covers leadless pacemakers as part of clinical research studies. The study must meet certain criteria and be approved by CMS and the Food and Drug Administration (FDA).The leadless pacemaker eliminates some causes of complications with traditional pacing systems. This summarizes CMS transmittal 201.
What Is a Medicare NCD?
An NCD defines coverage for a particular item (e.g., a brace or hearing aid) or service (e.g., therapy or screenings) nationwide. For example, a Medicare national coverage decision might specify coverage restrictions based on certain clinical conditions, prerequisite treatments and other factors.
What Is a Medicare LCD?
An LCD defines Medicare coverage for items and services for which no NCD exists. For example, there might be a local coverage determination for a new service or an item for which Medicare hasn’t yet published an national coverage determination.
Is There One Place I Can Go to Find Information About NCDs and LCDs?
Yes. The Medicare Coverage Database includes both LCDs and NCDs that are currently in place. Medicare provides a guide to help beneficiaries navigate the database.
What Should I Keep in Mind When Reading an NCD or LCD?
It’s easy to become overwhelmed when reading an NCD or LCD because they usually include a lot of clinical language. The “coverage guidance” is an important one to read, because that will explain any indications, limitations or medical necessity for a given service or item.
Can I Challenge an NCD or LCD?
Yes. If you don’t agree with an LCD or NCD, you can challenge it if you have Medicare Part A or B (or both) and you need the item or service not covered by the NCD or LCD.
What is coverage determination?
A coverage determination is the first decision made by your Medicare drug plan (not the pharmacy) about your. benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. , including these: Whether a certain drug is covered.
What is EOC in Medicare?
Medicare prescription drug coverage appeals. Your plan will send you information that explains your rights called an " Evidence of Coverage " (EOC). Call your plan if you have questions about your EOC. You have the right to ask your plan to provide or pay for a drug you think should be covered, provided, or continued.
How many levels of appeals are there for Medicare?
Your Medicare drug plan will send you a written decision. If you disagree with this decision, you have the right to appeal. The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level.
What is formulary in medical terms?
formulary. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list. .
