What is the Medicare deductible and how does it work?
How Does the Medicare Deductible Work? Your deductible is the amount of money you have to pay for your prescriptions and healthcare before Original Medicare, other insurance, or your prescription drug plan starts paying for your healthcare expenses.
When do Medicare deductibles change?
The government determines if Medicare deductibles will either rise or stay the same annually. Medicare announces Part A & Part B deductible changes each year around the end of October or the beginning of November.
What is a Medicare benefit period?
What Is A Benefit Period? In Medicare Part A, which is hospital insurance, a benefit period begins the day you go into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row. If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again.
When do you pay your health insurance deductible?
Many homeowners and car insurance policies charge a deductible whenever you file a claim. A health insurance deductible is usually charged once for the plan year. Starting January 1 or whenever your plan year begins, you pay your health care costs up to the deductible amount.

What is a deductible period?
A deductible is a set amount you may be required to pay out of pocket before your plan begins to pay for covered costs. Not every health plan has a deductible, and this amount may vary by plan. Every year, it starts over, and you'll need to reach the deductible again for that year before your plan benefits start.
Does Medicare deductible start over every year?
Medicare deductibles are reset each year and the dollar amount may be subject to change. Both Medicare Parts A and B have deductibles that must be met before Medicare starts paying. Medicare Advantage, Medigap and Part D plans are all sold by private insurance companies that set their own deductibles.
What is Medicare deductible this year 2022?
The 2022 Medicare deductible for Part B is $233. This reflects an increase of $30 from the deductible of $203 in 2021. Once the Part B deductible has been paid, Medicare generally pays 80% of the approved cost of care for services under Part B.
What does Medicare consider a calendar year?
The Medicare Part D plan year runs from January 1st through December 31st of each year, so the plan year runs for a calendar year rather than 365 days from the date of your initial enrollment (or Initial Enrollment Period).
What is the 3 day rule with Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
How do I know if my Medicare deductible has been met?
CMS mails your Medicare Summary Notice once a quarter. And, it doesn't provide important details about the Part B deductible. It will simply indicate if you've met the deductible.
Are Medicare premiums tax deductible in 2021?
Yes, your monthly Medicare Part B premiums are tax-deductible. Insurance premiums are among the many items that qualify for the medical expense deduction. Since it's not mandatory to enroll in Part B, you can be “rewarded” with a tax break for choosing to pay this medical expense.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
What is the annual deductible for Medicare Part B?
$233Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
What is deductible per calendar year?
Calendar-year deductible is an amount payable by an insured during a calendar year before a group or individual health insurance policy begins to pay for medical expenses.
What is the difference between benefit year and calendar year?
A plan on a calendar year runs from January 1–December 31. Items like deductible, maximum out-of-pocket expense, etc. will reset every January 1. All Individual and Family plans are on a calendar year. A plan on a contract year (also called benefit year) runs for any 12-month period within the year.
What is the Medicare Deductible for 2022?
A deductible refers to the amount of money you must pay out of pocket for covered healthcare services before your health insurance plan starts to p...
Does Original Medicare Have Deductibles?
Original Medicare is composed of Medicare Part A and Medicare Part B. Both parts of Original Medicare have deductibles you will have to pay out of...
Do You Have to Pay a Deductible with Medicare?
You’ve probably heard the one about death and taxes. If you have Original Medicare, you can add deductibles to that list.
Key Takeaways
Parts A and B of Original Medicare have deductibles you must meet before Medicare will pay for healthcare.
What is the Medicare Deductible for 2022?
A deductible refers to the amount of money you must pay out of pocket for covered healthcare services before your health insurance plan starts to pay. A deductible can be based upon a calendar year, upon a plan year or — as is unique to Medicare Part A — upon a benefit period.
Does Original Medicare Have Deductibles?
Original Medicare is composed of Medicare Part A and Medicare Part B. Both parts of Original Medicare have deductibles you will have to pay out of pocket before your plan starts to pay for your healthcare.
Medicare Advantage (Part C) Deductibles
Medicare Advantage (Part C) is an alternative type of Medicare plan that is purchased through a private insurer. Not every Part C plan is available throughout the country. Your state, county and zip code will determine which plans are available for you to choose from in your area.
Medicare Part D Deductibles
Medicare Part D is prescription drug coverage. People are often surprised to learn that Part D is not included in Original Medicare. This is understandable since prescription medications are very often integral to health.
Medicare Supplement Plan Deductible Coverage
Medicare Supplement Insurance is also known as Medigap. Medigap is supplemental insurance sold by private insurers. It is designed to fill in the cost “gaps” for people who have Original Medicare.
Do You Have to Pay a Deductible with Medicare?
You’ve probably heard the one about death and taxes. If you have Original Medicare, you can add deductibles to that list.
What Is a Deductible?
A deductible is the amount of money that you must pay out of your own pocket for covered care before your plan coverage kicks in.
Medicare Part A Deductible
Medicare Part A covers inpatient care received at a hospital, skilled nursing facility or other inpatient facility.
What Is the Maximum Cost of Medicare Part B?
Medicare Part B does come with a premium cost. The monthly premium prices are set annually and depend on your annual income. Premium costs start at $170.10 per month. The maximum cost of Medicare Part B premiums is $578.30 per month in 2022, and that's for individuals reporting half a million dollars or more in income in 2020.
Medicare Part C (Medicare Advantage) Deductible
Medicare Part C plans, otherwise known as Medicare Advantage plans, are an alternative way to get Original Medicare benefits, often with additional coverage.
Medicare Part D Deductible
Medicare Part D plans cover prescription medications. Like Medicare Advantage, plans Medicare Part D plans are sold by private insurers and thus there is no standard deductible.
Medicare Supplement Deductibles by Plan
There are 10 standardized Medicare Supplement plans (also called Medigap) available in most states, and two of those plans offer a high-deductible option. Medigap Plan F and Plan G have high-deductible options that include an annual deductible of $2,490 in 2022.
How much does Medicare cover if you have met your deductible?
If you already met your deductible, you’d only have to pay for 20% of the $80. This works out to $16. Medicare would then cover the final $64 for the care.
What is the Medicare Part B deductible for 2020?
The Medicare Part B deductible for 2020 is $198 in 2020. This deductible will reset each year, and the dollar amount may be subject ...
How much is Medicare Part B 2020?
The Medicare Part B deductible for 2020 is $198 in 2020. This deductible will reset each year, and the dollar amount may be subject to change. Every year you’re an enrollee in Part B, you have to pay a certain amount out of pocket before Medicare will provide you with coverage for additional costs.
How much is a broken arm deductible?
If you stayed in the hospital as a result of your broken arm, these expenses would go toward your Part A deductible amount of $1,408. Part A and Part B have their own deductibles that reset each year, and these are standard costs for each beneficiary that has Original Medicare. Additionally, Part C and Part D have deductibles ...
What happens when you reach your Part A or Part B deductible?
What happens when you reach your Part A or Part B deductible? Typically, you’ll pay a 20% coinsurance once you reach your Part B deductible. This coinsurance gets attached to every item or service Part B covers for the rest of the calendar year.
Does Medicare Advantage have coinsurance?
They can offer coverage for some of the expenses you’ll have as a Medicare beneficiary like deductibles and coinsurance. An alternative to Original Medicare, a Medicare Advantage, or Medicare Part C, plan will offer the same benefits as Original Medicare, but most MA plans include additional coverage.
How much is Medicare Part B deductible?
Medicare Part B also employs a deductible. Unlike Part A, Part B has an annual deductible. In 2019, the annual Part B deductible is $185. That means you’re responsible for non-inpatient bills up to that amount.
How much is the 2019 deductible?
Your deductible for each period in 2019 is $1364. That means you’ll be charged up to that amount for any services provided during your inpatient stay at the hospital. The same deductible applies for each benefit period if you’re admitted as an inpatient at a skilled nursing facility for a period of time.
What does Medicare Part A cover?
Medicare Part A (Hospital Insurance) helps cover inpatient care in hospitals or skilled nursing facilities, in hospice, or home health care. For example, if you have an infected appendix and you are admitted to the hospital for a surgeon to perform an appendectomy, Part A will help cover the costs during your stay, ...
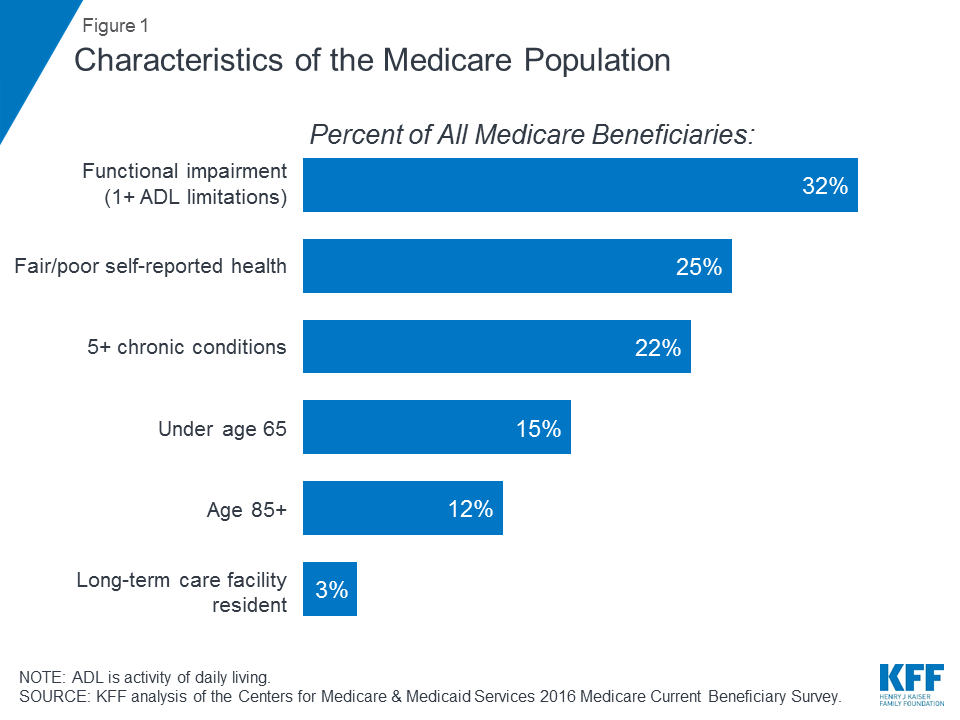
What is Medicare for seniors?
Medicare is the primary hospital and medical insurance coverage for tens of millions of Americans aged 65 or older or under 65 who qualify due to disabilities.
When does the benefit period start?
Your benefit period starts when you get admitted. When you get discharged, a countdown begins. If you go 60 days without receiving more inpatient care, you start a new benefit period. Your deductible goes back into effect for each benefit period.
Is it reasonable for Medicare to know about deductibles?
Any cost above what appears in their normal budget poses a risk to their financial security. Given those circumstances, it is reasonable for Medicare recipients to want to know about what, if any, kind of deductibles apply to their Medicare coverage.
What is Medicare benefit period?
Medicare benefit periods mostly pertain to Part A , which is the part of original Medicare that covers hospital and skilled nursing facility care. Medicare defines benefit periods to help you identify your portion of the costs. This amount is based on the length of your stay.
How long does Medicare benefit last after discharge?
Then, when you haven’t been in the hospital or a skilled nursing facility for at least 60 days after being discharged, the benefit period ends. Keep reading to learn more about Medicare benefit periods and how they affect the amount you’ll pay for inpatient care. Share on Pinterest.
How much coinsurance do you pay for inpatient care?
Days 1 through 60. For the first 60 days that you’re an inpatient, you’ll pay $0 coinsurance during this benefit period. Days 61 through 90. During this period, you’ll pay a $371 daily coinsurance cost for your care. Day 91 and up. After 90 days, you’ll start to use your lifetime reserve days.
What facilities does Medicare Part A cover?
Some of the facilities that Medicare Part A benefits apply to include: hospital. acute care or inpatient rehabilitation facility. skilled nursing facility. hospice. If you have Medicare Advantage (Part C) instead of original Medicare, your benefit periods may differ from those in Medicare Part A.
Why is it important to check deductibles each year?
It’s important to check each year to see if the deductible and copayments have changed, so you can know what to expect. According to a 2019 retrospective study. Trusted Source. , benefit periods are meant to reduce excessive or unnecessarily long stays in a hospital or healthcare facility.
How much is Medicare deductible for 2021?
Here’s what you’ll pay in 2021: Initial deductible. Your deductible during each benefit period is $1,484. After you pay this amount, Medicare starts covering the costs. Days 1 through 60.
How long does Medicare Advantage last?
Takeaway. Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
How long does Medicare Part A deductible last?
At the beginning of each benefit period, the Medicare Part A deductible must be paid by beneficiaries. A benefit period extends from the day a patient is admitted to the hospital until the final day treatment is received. If a beneficiary goes 60 days in a row without receiving treatment, the benefit period restarts and a deductible will have ...
How long does Medicare cover a room?
After the initial Part A deductible has been paid by the beneficiary during the first 60 days, Medicare will cover all other costs associated with a room, meals, doctor and nursing services, treatment, and exams. If a beneficiary needs to stay in the hospital beyond 150 days, or returns to the hospital with less than 60 days between visits ...
What is Medicare for seniors?
Medicare was designed with the goal of providing all senior citizens in America with reliable and affordable health care coverage. The program also strives to provide senior citizens with quality coverage and while the program eliminates many costs associated with health care for seniors, the system still has premiums, co-insurances, ...
Does Medicare Part A require a deductible?
The other portion of health care that Medicare Part A covers generally doesn’t require a deductible to be paid first. After a certain period of time, beneficiaries who require a stay in a skilled nursing facility will have to pay out of pocket for their stay. These costs include:
Does Medicare pay for hospice?
The only out of pocket costs associated with Part A coverage for home health services and hospice stays involve premiums for medication and durable medical goods. Medicare strives to pay for as much of the cost involved in a senior citizens health care as possible, but the system does have deductibles that must be met first before full coverage ...
How long does Medicare Part A deductible last?
In this case, it only applies to Medicare Part A and resets (ends) after the beneficiary is out of the hospital for 60 consecutive days. There are instances in which you can have multiple benefit periods within a calendar year. This means you’ll end up paying a Part A deductible more than once in 12 months.
How does Medicare benefit period work?
How Do Medicare Benefit Periods Work? It’s important to understand the difference between Medicare’ s benefit period from the calendar year. A benefit period begins the day you’re admitted to the hospital or skilled nursing facility. In this case, it only applies to Medicare Part A and resets ...
What is the deductible for Medicare 2021?
Yearly Medicare Deductibles. The calendar-year deductible is what you must pay before Medicare pays its portion, but you will still have coverage until you reach your deductible. In 2021, the deductible for Part A costs $1,484, while Part B’s deductible is $203.
How long does Medicare cover inpatient care?
Part A covers inpatient hospital care, skilled long-term facility, and more, for up to 90 days. But if you ever need to extend your hospital stay, Medicare will cover 60 additional days, called lifetime reserve days. For instance, if your hospital stay lasts over 120 days, you will have used 30 lifetime reserve days.
How many Medigap plans are there?
One way to avoid paying for deductibles is by purchasing Medicare Supplement, also called a Medigap plan. There are 12 Medigap plans, letters A-N. Each plan varies by price and benefits. All Medigap plans, with the exception of Plan A, cover the Part A deductible.
How many lifetime reserve days can you use?
For instance, if your hospital stay lasts over 120 days, you will have used 30 lifetime reserve days. Please note that you’ll pay a coinsurance of $742 for each lifetime reserve day you use. You can only use your lifetime reserve days once.
Do Medicare Advantage plans have a benefit period?
The Medicare Advantage plans that use benefit periods are typically for skilled nursing facility stays. A large majority of Medicare Advantage plans do not use benefit periods for hospital stays. Most beneficiaries pay a copayment for the first few days. Afterward, you’re required to pay the full amount for each day.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.