
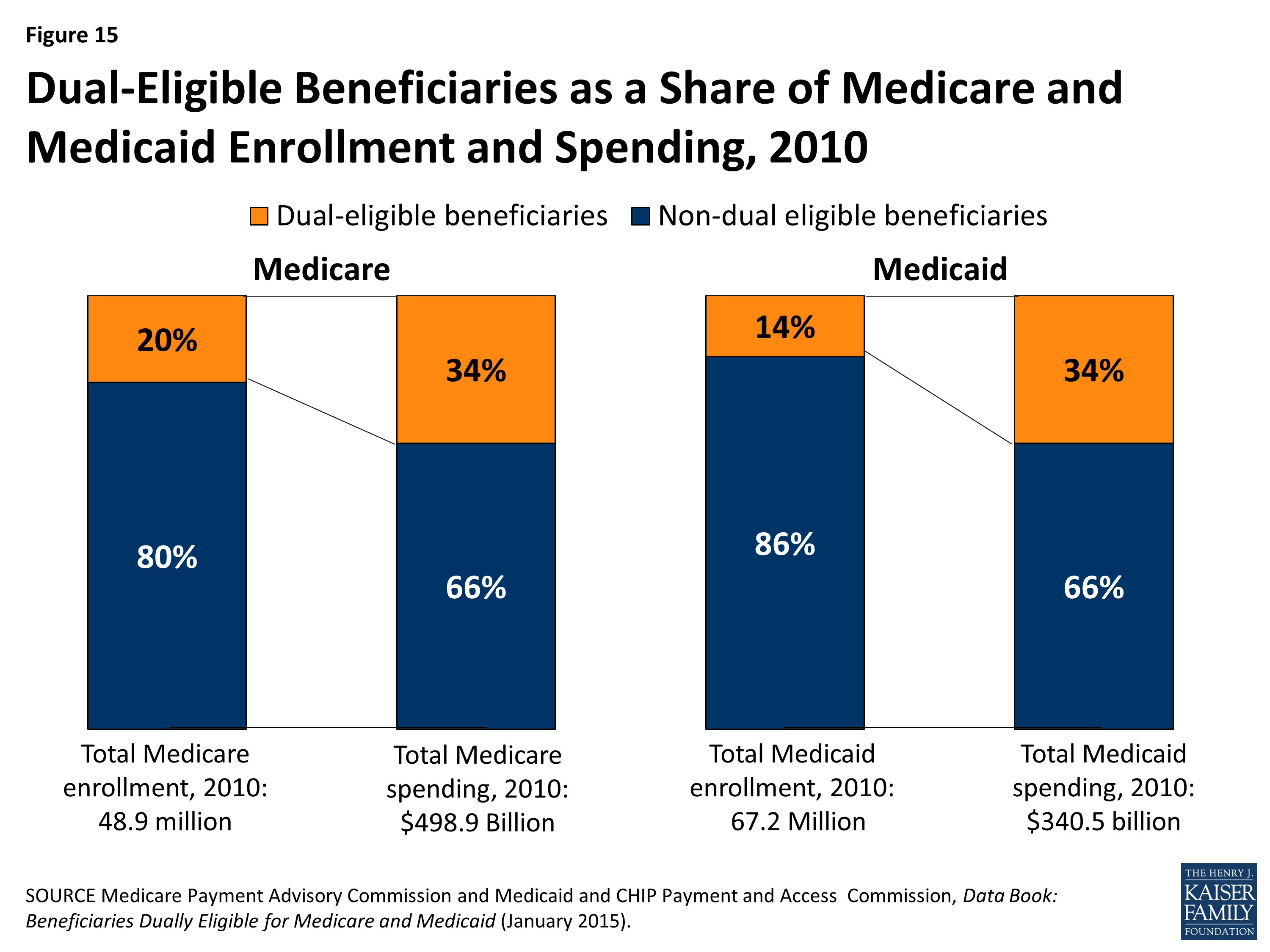
Dually eligible beneficiaries generally describe low-income beneficiaries enrolled in both Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How to pay for dual enrollment?
- Applicants must provide a letter of recommendation from his/her high school counselor or school officials for concurrent enrollment program participation. ...
- Students must maintain a ≥ 3.0 GPA in their high school studies to be eligible for this program.
- The maximum amount of UNTF assistance available annually is determined by the UNTF Board. ...
What are the benefits of dual enrollment?
The Difference
- Advanced Placement (AP)
- International Baccalaureate (IB)
- Dual Credit/Concurrent Credit
What is Medicare dual eligible and how do I qualify?
What type of coverage do you get if you are dual eligible for Medicare and Medicaid?
- Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
- Specified Low-Income Medicare Beneficiary (SLMB) Program. The SLMB program helps pay for Medicare Part B premiums.
- Qualifying Individual (QI) Program. ...
- Qualified Disabled Working Individual (QDWI) Program. ...
How do you become dual eligible for Medicare and Medicaid?
- Estate Recovery
- MAGI Conversion Plan
- Seniors & Medicare and Medicaid Enrollees
- Verification Plans
- Minimum Essential Coverage
- Spousal Impoverishment
- Medicaid Third Party Liability & Coordination of Benefits
- Medicaid Eligibility Quality Control Program
What does it mean if a Medicare patient is dual eligible?
Dually eligible beneficiaries are people enrolled in both Medicare and Medicaid who are eligible by virtue of their age or disability and low incomes.
Can I have dual coverage with Medicare?
If you qualify for both Medicare and Medicaid, you are considered "dual eligible." Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
What is a dual coverage?
If you are covered under two different dental insurance plans, then you have dual dental coverage. Dual dental coverage typically occurs when you have two jobs that each provide dental benefits, or you are covered by your spouse's dental plan in addition to your own.
What plan provides both Medicare and Medicaid coverage?
UnitedHealthcare Connected® for One Care (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How does two health insurances work?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
How does double health insurance work?
Dual coverage: You each sign up for coverage from your employer and you each cover each other, or the entire family, on your plan. This is called dual coverage. It will be more expensive to have two plans but it might provide more coverage in some cases.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
What is dual eligible?
Full dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income (SSI) benefits, which provide cash assistance for basic food ...
What is partial dual eligibility?
Partial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
What is the Medicare and Medicaid program?
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly. PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities. Some of the things that can be covered by PACE include: Adult day primary care. Dental care.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What is a dual SNP?
If you are Medicare dual eligible, you may qualify for a Medicare D-SNP (Dual Special Needs Plan), which is a type of Medicare Advantage plan. 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2.
What is an annual special enrollment period?
An annual Special Enrollment Period to enroll in a Part D plan or switch to a new one. Elimination of Part D late enrollment penalties. You automatically qualify for Extra Help if you are enrolled in Medicaid, Supplemental Security Income or a Medicare Savings Program.
What is dual enrollment in Medicare?
What is Dual Enrollment? Dual enrollment refers to the situation where a person can qualify to enroll in both, Medicare as well as Medicaid. It will include Part A, Part B and Part D portion of Medicare.
How many people are eligible for dual enrollment?
It is estimated that there are over 9 million people in the US who are qualified to get Dual enrollment. In most circumstances, Medicare is the main provider of health insurance. However, Medicaid was put in place to cover some of the things Medicare did not cover. Contents [ show]
What is Medicaid based on?
Eligibility into Medicaid is based on income calculated using the Modified Adjusted Gross Income (MAGI). This system decides what income is considered when calculating a person’s financial eligibility . Only the taxable amount of social security income is used to determine the financial status of the individual or family. MAGI takes a person’s adjusted gross income, taxable social security benefits, tax-exempt interest, and excluded foreign income to come up with the final determination.
What is the second most common disability?
Qualifying with a Disability. The second most common are young people who have disabilities and also come from low-income families. However, in order for young people to be qualified, they may need to go the extra mile to prove that they need it, compared to senior citizens.
What is overlap in Medicare?
An overlap occurs in many situations. This happens when a person is eligible for Medicare but still has an income that falls within the Medicaid guidelines. There are critical facts about dual enrollment in Medicare, in addition to facts about dual-enrollment in Medicaid.
How old do you have to be to qualify for medicare?
There are many resources for those eligible for Medicare. People either over age 64 or disabled aged 19 to 64 can qualify.
What is a QMB plan?
Qualified Medicare Beneficiary or QMB plan. Qualified Disabled Working Individual or QDWI plan. An individual who qualifies for Dual enrollment can choose their coverage according to the Medicare Advantage Plan. This means the dual plan will first be paid by Medicare.
What is dual eligibility?
You’re also considered a dual eligible beneficiary if you’re enrolled in Medicare Part A or Part B and receiving cost-sharing through a Medicare savings program (MSP). Below is table summarizing the benefits and eligibility criteria for each of the different MSPs in 2021: MSP. Benefits.
How many people are on Medicare and Medicaid?
According to Health Affairs, about 9.2 million people, representing about 16 percent of Medicare enrollees and about 15 percent of Medicaid enrollees, are enrolled in both Medicare and Medicaid. Keep reading to learn more about dual eligibility, benefits, and state-by-state differences.
What is the difference between Medicare and Medicaid?
Takeaway. Medicare is the federal health insurance program in the United States for people age 65 and older. Medicaid is a joint federal and state program to help people with limited resources or income pay for medical costs.
What is fee for service Medicaid?
fee-for-service Medicaid coverage. plans that include all Medicare and Medicaid benefits. Income and resource standards are defined by federal law for full Medicaid and the Medicare Savings Programs. At their discretion, states can effectively raise the federally mandated limits.
Is Medicare a dual beneficiary?
If you’re eligible for both Medicare and Medicaid, you’re considered a dual eligible beneficiary. Dual eligibility is typically determined by your age, any disabilities, and income.
Is Medicare free for older people?
It also covers people with certain disabilities and health conditions. Medicare is not free coverage — you’ll still pay deductibles, premiums, and copays for medical services.
Is dual eligibility covered by insurance?
If you’re a dual eligibility beneficiary, it’s likely that most of your healthcare costs are covered. The information on this website may assist you in making personal decisions about insurance, but it is not intended to provide advice regarding the purchase or use of any insurance or insurance products.
What Is Medicare?
Medicare is a federal health insurance program for older people (65 and over), younger people with disabilities, and individuals who have ESRD (End-Stage Renal Disease).
What Is Medicaid?
Medicaid is a federal government and state health care program for low-income individuals of any age in the U.S. This health insurance offers affordable health care options to people who can't afford to pay for medical items, services, and treatments.
What Is Dual Eligibility?
There are a variety of reasons why people may struggle to cover the costs of Medicare insurance.
Who Can Apply for Dual Eligibility?
To qualify for dual eligibility, you need to meet the enrollment criteria for both the Medicare and Medicaid program.
Part A and B Financial Help
Once you're dual eligible, you’ll be able to use your Medicaid to pay some or all of your Original Medicare premiums and health care costs.
Dual-Eligible Benefit Types
There are six types of dual-eligible beneficiaries. Each one has its own financial requirements to enroll and offers other relief from Medicare health care costs.
Dual Eligible and Medicare Advantage
Certain dual eligibles are still allowed to enroll for Medicare Advantage plans. These are called Special Needs Plans (SNPs) and are designed to cater to dual eligibles and other specific groups.
