What makes a good Medicaid managed care plan?
Jul 16, 2021 · Medicare managed care plans are an alternative option to Original Medicare. Otherwise known as Medicare Advantage plans, most are either HMOs or PPOs. However, there are other less common plan types available. Managed care plans provide additional benefits to Medicare Part A and Part B coverage.
What does managed care actually mean?
Nov 17, 2021 · A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) or POS (point of service) plans. These Medicare Advantage plans offer managed care that is coordinated between health care providers within a network.
How to apply for Medicaid Managed Care?
Sep 09, 2020 · Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare. They’re required to cover ...
What are the types of managed care?
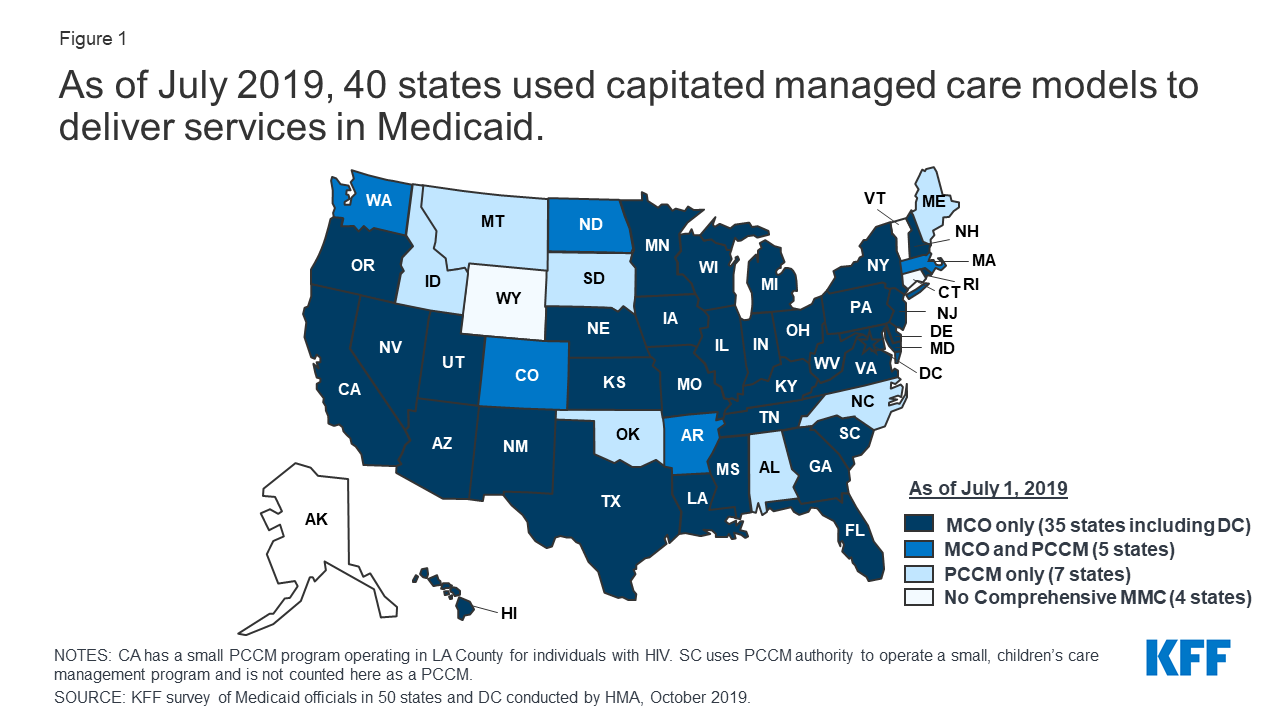
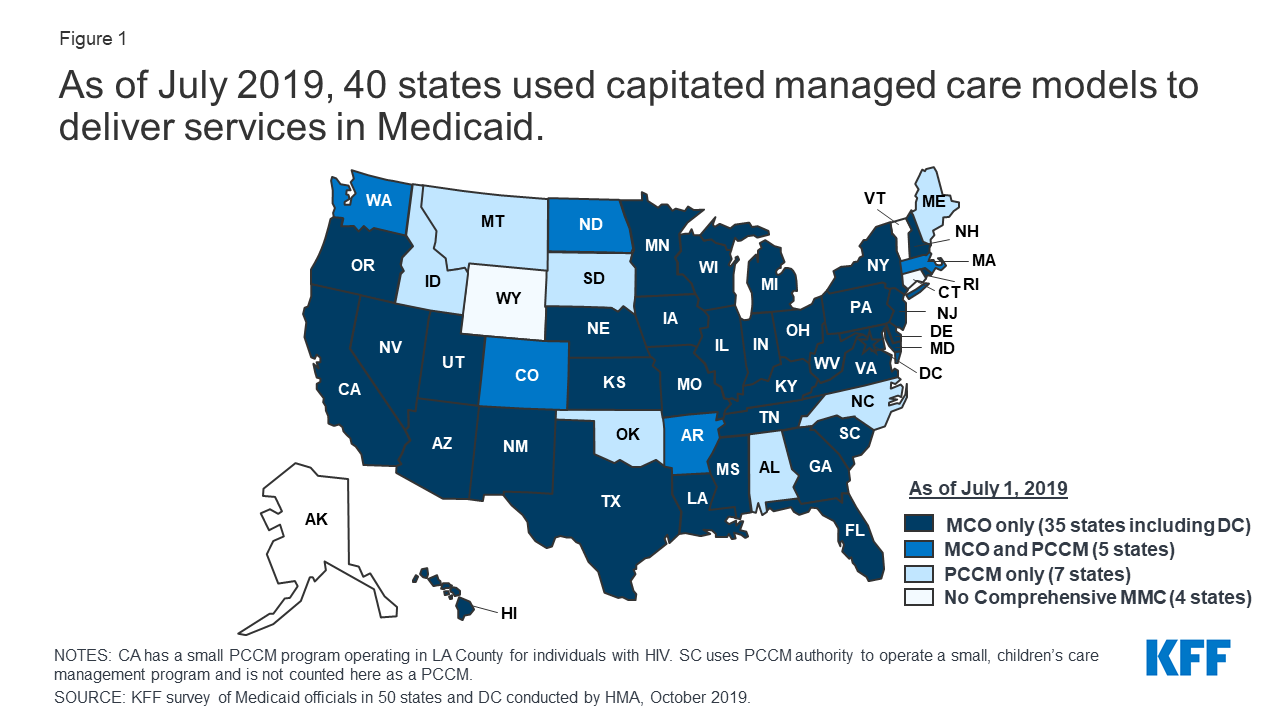
Managed Care is a health care delivery system organized to manage cost, utilization, and quality. Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs) that accept a set per member per month (capitation) …
What is the difference between Medicare and Medicare managed care?
Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare.Sep 9, 2020
What is an example of a managed care plan?
A good example of a managed care plan is an HMO (Health Maintenance Organization). HMOs closely manage your care. Your cost is lowest with an HMO. You are limited to seeing providers in a small local network, which also helps keep costs low.
What does managed care mean in healthcare?
Managed Care is a health care delivery system organized to manage cost, utilization, and quality.
What is the difference between Medicare fee for service and managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
How does managed care work?
Under managed care, states sign contracts with "managed care organizations," or MCOs, that provide medical services through their own networks of doctors and hospitals. The state pays the MCO a fixed annual fee for each Medicaid patient. And the MCO takes responsibility for overseeing each person's care.May 31, 2011
What is the purpose of managed care?
The purpose of managed care is to enhance the quality of healthcare for all patient populations. Managed care revolves around the collaboration of health insurance plans and healthcare providers. Managed Care includes healthcare plans that are used to manage cost, utilization, and quality.Dec 29, 2020
What are the benefits of managed care?
What Are the Advantages of Managed Care?It lowers the costs of health care for those who have access. ... People can seek out care from within their network. ... Information moves rapidly within a network. ... It keeps families together. ... There is a certain guarantee of care within the network.More items...•Jun 14, 2017
What are the two major forms of managed care?
The main types of managed health care plans include: Health maintenance organization (HMO) Preferred provider organization (PPO) Point of service (POS)
What is the most common form of managed care?
HMOThe most common type of managed care plan is the HMO. If you enroll in an HMO plan, you'll need to pick a primary care provider who will direct all your healthcare needs and refer you to specialists when appropriate. You are only covered if you go to medical providers and facilities who are in your network.
What is a managed care plan?
Managed care plans are a type of health insurance. They have contracts with health care providers and medical facilities to provide care for members at reduced costs. These providers make up the plan's network. How much of your care the plan will pay for depends on the network's rules.Sep 20, 2018
What are the three main payment mechanisms used in managed care?
What are the three main payment mechanisms managed care uses? In each mechanism who bears the risk. The three main types of payment arrangements with providers are: capitation, discounted fees, and salaries.
Which part of Medicare is the managed care option?
Terms in this set (10) Which part of Medicare is the managed care option? Part C is Medicare's managed care option. Medicare Advantage is the name of the program.
What are the benefits of Medicare managed care?
Benefits can include routine vision, dental and hearing services. Additionally, managed care plans offer prescription drug coverage. The cost of medications out-of-pocket can be financially exhausting. Medicare managed care plans can provide some relief.
What is managed care plan?
Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan. MA plans decide on rate amounts, making prices different from plan to plan. Processing payments are done through the private plan, not Medicare.
What is Medicare Advantage 2021?
Updated on March 19, 2021. Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
Does an indemnity plan have a provider network?
Members will receive reimbursement for medical expenses (up to a certain amount). Indemnity plans have no provider network, members can visit the doctor (s) of their choice. Contrarily, managed care plans have a network (s) of providers, with different plan options.
Does managed care plan limit doctors?
On the other hand, managed care plans may limit beneficiaries to only the doctors within the plan’s network. If having the freedom to see any healthcare provider of choice is important, remember that Advantage plans limit provider options. While traveling within the country, managed care pays for emergency services only.
Is Medicare Supplement the same as Managed Care?
Managed-care plans and Medicare Supplement plans are not the same. This misconception is common. Both provide additional benefits to Original Medicare. However, they serve two totally different purposes. Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
What is managed care network?
The networks of managed care plans often include pharmacies, which can help make ordering and filling prescriptions faster and easier for everyone involved . There’s less uncertainty about a beneficiary’s costs for care in a managed care plan, provided they stay within the assigned network for qualified services.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Can you use a primary care physician in a point of service plan?
But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
What is Medicare Part B?
Medicare Part B covers individual and group therapy services to diagnose and treat mental illness. The Part B coverage usually requires a physician referral for mental health care and is based on a mental health diagnosis.
Does MA offer alternative therapies?
MA plans may offer alternative therapies as supplemental benefits. These alternative therapies must be provided by practitioners who are licensed or certified, as applicable, in the state in which they practice and are furnishing services within the scope of practice defined by their licensing or certifying state. MA plans are to provide a description of therapies offered in the PBP Notes section.
Does MA offer chiropractic care?
MA plans may choose to offer routine chiropractic services as a supplemental benefit as long as the services are provided by a state-licensed chiropractor practicing in the state in which he/she is licensed and is furnishing services within the scope of practice defined by that state’s licensure and practice guidelines. The routine services may include conservative management of neuromusculoskeletal disorders and related functional clinical conditions including, but not limited to, back pain, neck pain and headaches, and the provision of spinal and other therapeutic manipulation/adjustments.
Is an indemnity plan a managed care plan?
Indemnity plans were popular before the advent of modern managed care plans, but they have been largely replaced by managed care plans over the last few decades, and the vast majority of privately insured Americans are in some form of managed care plan.
Is managed care part of Medicare?
Even in the Medicaid and Medicare systems, managed care is playing an increasingly large role: More than two-thirds of the people enrolled in Medicaid were covered under private Medicaid managed care plans as of 2017.
