An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can file an appeal if Medicare or your plan denies: A request for a health care service, supply, item, or prescription drug that you think you should be able to get
What are the levels of Medicare appeal?
There are five levels in the Medicare claims appeal process:
- Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim.
- Level 2: An Independent Organization. ...
- Level 3: Office of Medicare Hearings and Appeals (OMHA). ...
- Level 4: The Medicare Appeals Council. ...
- Level 5: Federal Court. ...
What is the Medicare appeal process?
What is the process for filing an appeal?
- You’ve received an official notice. There are a few different notices you might receive from Medicare that would set off an appeal. ...
- Initiating an appeal. You’ll need to appeal within 120 days of receiving notice for the noncovered service. ...
- Levels of appeal. There are five levels of the Medicare appeal process. ...
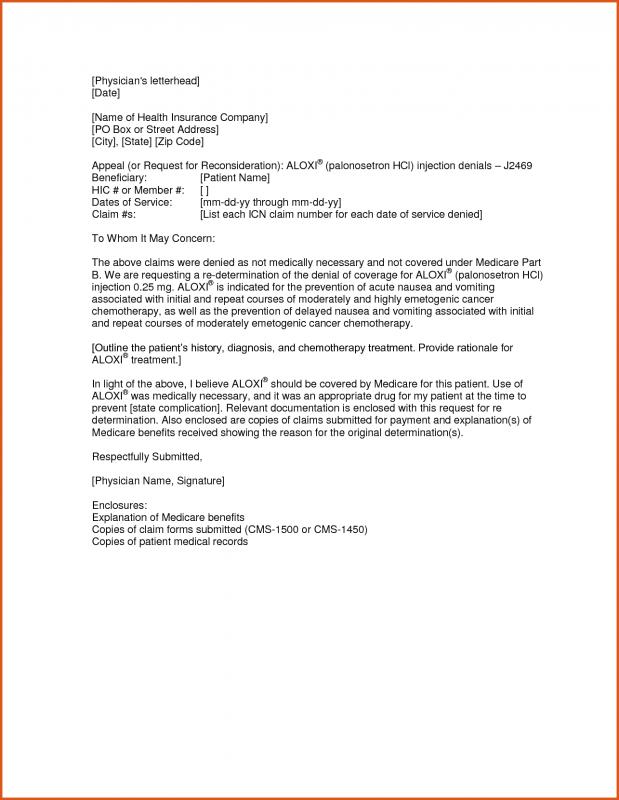
How to properly compose Medicare appeal letter and its sample?
Sample Appeal Letter A. Please accept this letter as [patient's name] appeal to [insurance company name] decision to deny coverage for [state the name of the specific procedure denied]. It is my understanding based on your letter of denial dated [insert date] that this procedure has been denied because: [quote the specific reason for the denial ...
How does the Medicare appeals process work?
To increase your chance of success, you may want to try the following tips:
- Read denial letters carefully. ...
- Ask your healthcare providers for help preparing your appeal. ...
- If you need help, consider appointing a representative. ...
- Know that you can hire legal representation. ...
- If you are mailing documents, send them via certified mail. ...
- Never send Medicare your only copy of a document. ...
- Keep a record of all interactions. ...

What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
What are the five levels of the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What is the first step in the Medicare appeals process?
If you disagree with the Medicare contractor's decision on your claim, you have the right to file an appeal. The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
What happens if Medicare denies a claim?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
What is the purpose of the appeals process is it an effective process?
The first thing to understand is what the purpose of the appeals process actually is. Rather than being a re-trying of your case, it is a judicial review of the decision of the trial court that heard it initially. A judge will review all the relevant facts and determine if a harmful legal error occurred.
When benefits in a Medicare policy are denied a patient has the right to appeal to quizlet?
Judicial Review. The final level of appeal for Medicare is to request a Judicial Review in Federal District Court. The threshold for review in federal district court in 2016 is $1,460.00 and is calculated each year and may change.
What are the four levels of Medicare appeals?
First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA) Fourth Level of Appeal: Review by the Medicare Appeals Council.
Can you be denied Medicare coverage?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What is the purpose of the appeals process in medical billing?
The medical billing appeals process is the process used by a healthcare provider if the payer (insurance company)or the patient disagrees with any item or service provided and withholds reimbursement payment.
What is Medicare appeal?
It helps to provide evidence that supports your appeals case from a doctor or other provider. There might be times when Medicare denies your coverage for an item, service, or test. You have the right to formally disagree with this decision and encourage Medicare to change it. This process is called a Medicare appeal.
Why do you appeal Medicare?
Reasons for appeal. Appeals process. Takeaway. You’ll receive a notice when Medicare makes any decisions about your coverage. You can appeal a decision Medicare makes about your coverage or price for coverage. Your appeal should explain why you don’t agree with Medicare’s decision. It helps to provide evidence that supports your appeals case ...
Why is Medicare denying my coverage?
There are a few reasons Medicare might deny your coverage, including: Your item, service, or prescription isn’t medically necessary.
What is a fast appeal?
In a few cases, you’ll file what’s called a fast appeal. Fast appeals apply when you’re notified that Medicare will no longer cover care that’s: at a hospital. at a skilled nursing facility. at a rehabilitation facility. in hospice.
How long does it take to get a decision from Medicare?
You’ll hear a decision about your appeal within 60 days.
What is level 3 appeal?
At level 3, you’ll have the chance to present your case to a judge. You’ll need to fill out a request form detailing why you disagree with your level 2 decision. Your appeal will only be elevated to level 3 if it reaches a set dollar amount. Office of Medicare Hearings and Appeals review.
How many levels of appeals are there?
The appeals process has five levels. Each level is a different review process with a different timetable. You’ll need to request an appeal at each level. If your appeal is successful at the first level, or if you agree with Medicare’s reasoning for denying your appeal, you can stop there. However, if your appeal was denied ...
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is a fast appeal?
If waiting for a decision would affect a person’s health, they can ask for a fast appeal. An example of the need for a fast decision might be if someone is an inpatient in a hospital or SNF and they are concerned that the facility is discharging them too soon.
What happens if Medicare denies coverage?
If Medicare denies coverage of an item or service, an individual has the right to appeal the decision. People must provide proof with a claim and submit this to Medicare with an application form.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Who can help you file an appeal for Medicare?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the