
While an appeal generally involves a Medicare decision not to pay for an item or service, a complaint (also called a grievance) involves the quality of care or services you received from a Medicare provider or the Medicare plan. You can file grievances about virtually any aspect of Medicare. Click to see full answer
Who can assist with a Medicare appeal?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
Where to send Medicare Appeals?
- Circle the item (s) and/or services you disagree with on the MSN.
- Explain in writing why you disagree with the decision or write it on a separate piece of paper, along with your Medicare number, and attach it to the MSN.
- Include your name, phone number, and Medicare Number on the MSN.
How to appeal a denial of Medicare?
There are four steps in the appeal process:
- Molina Healthcare Standard and Expedited Appeal
- State Administrative Hearing
- Independent Review
- Health Care Authority (HCA) Board of Appeals Review Judge Decision
What is the appeal process for Medicare?
There are five levels of a Medicare appeal: (1) redetermination, (2) reconsideration, (3) hearing, (4) review, and finally (5) judicial review in federal district court. Each level of the appeal process has its own requirements and time limits for filing.
What does grievance and appeals mean?
Grievance: Concerns that do not involve an initial determination (i.e. Accessibility/Timeliness of appointments, Quality of Service, MA Staff, etc.) Appeal: Written disputes or concerns about initial determinations; primarily concerns related to denial of services or payment for services.
What is considered a Medicare grievance?
A complaint is about the quality of care you got or are getting. For example, you can file a complaint if you have a problem calling the plan, or you're unhappy with how a staff person at the plan treated you. You file an appeal if you have an issue with a plan's refusal to cover a service, supply, or prescription.
What are the five levels of the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
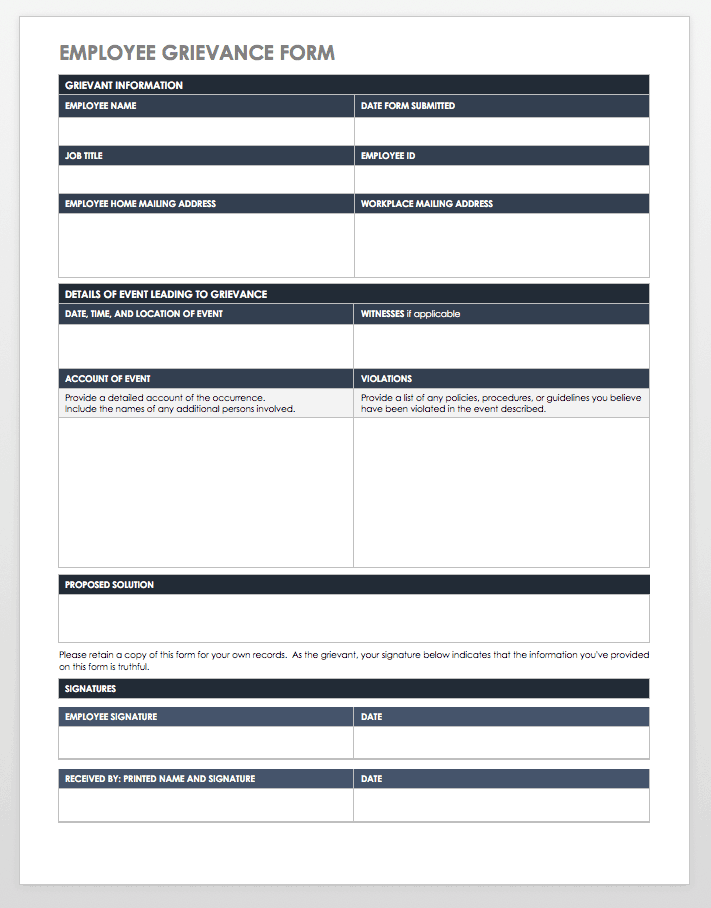
What does filing a grievance accomplish?
An effective grievance procedure provides employees with a mechanism to resolve issues of concern. The grievance procedure may also help employers correct issues before they become serious issues or result in litigation.
What is considered a grievance?
An employee grievance is a concern, problem, or complaint that an employee has about their work, the workplace, or someone they work with—this includes management. Something has made them feel dissatisfied, and they believe it is unfair and/or unjust on them.
What is a Medicare appeal?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
How often are Medicare appeals successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What are the six levels of appeals for Medicare Advantage plans?
Appealing Medicare DecisionsLevel 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
What is a first level appeal?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination.
What are grievances in healthcare?
Examples of grievance include: 1 Problems getting an appointment, or having to wait a long time for an appointment 2 Disrespectful or rude behavior by doctors, nurses or other plan clinic or hospital staff
What are some examples of grievances?
Examples of grievance include: Problems getting an appointment, or having to wait a long time for an appointment. Disrespectful or rude behavior by doctors, nurses or other plan clinic or hospital staff.
What is the role of each Medicare plan?
Each plan must provide meaningful procedures for timely resolution of both standard and expedited grievances between enrollees and the Medicare health plan or any other entity or individual through which the Medicare health plan provides health care services.
What is a MOON in Medicare?
Medicare Outpatient Observation Notice (MOON) Hospitals and CAHs are required to provide a MOON to Medicare beneficiaries (including Medicare Advantage health plan enrollees) informing them that they are outpatients receiving observation services and are not inpatients of a hospital or critical access hospital (CAH).
What is a CMS model notice?
CMS model notices contain all of the elements CMS requires for proper notification to enrollees or non-contract providers, if applicable. Plans may modify the model notices and submit them to the appropriate CMS regional office for review and approval. Plans may use these notices at their discretion.
When does a plan issue a written notice?
A plan must issue a written notice to an enrollee, an enrollee's representative, or an enrollee's physician when it denies a request for payment or services. The notice used for this purpose is the:
How long does it take to appeal a Medicare Advantage plan?
You may file an appeal within sixty (60) calendar days of the date of the notice of the initial coverage decision. For example, you may file an appeal for any of the following reasons: your Medicare Advantage health plan refuses to cover or pay for services you think your Medicare Advantage health plan should cover.
How long does it take to file a grievance for a drug claim?
You may file a grievance within ninety (90) calendar days for Part C/Medical and sixty (60) calendar days for Part D after the problem happened. You may file a Part C/medical grievance at any time. Grievances regarding your drug benefit (Part D) must be filed within sixty (60) days after the problem happened.
What is the process of determining if a drug is covered?
An initial coverage decision about your Part D drugs is called a "coverage determination.", or simply put, a "coverage decision.".
What is the process of making appeals?
The process for coverage decisions and making appeals deals with problems related to your benefits and coverage for prescription drugs , including problems related to payment. This is the process you use for issues such as whether a drug is covered or not and the way in which the drug is covered.
What to do if you disagree with a pharmacy's coverage decision?
If you disagree with this coverage decision, you can make an appeal. In general, if you bring your prescription to a pharmacy and the pharmacy tells you the prescription isn't covered under your plan, that isn't a coverage determination. You need to call or write to us to ask for a formal decision about the coverage.
Can someone else file a grievance for you?
Someone else may file the grievance for you on your behalf. You may appoint an individual to act as your representative to file the grievance for you by following the steps below: Provide your Medicare Advantage health plan with your name, your and a statement, which appoints an individual as your representative.
Is a syringe covered by Medicare?
Depending on how this drug is used, it may be covered by either Medicare Part B (doctor and outpatient health care) or Medicare Part D (prescription drugs). Your doctor may need to provide the plan with more information about how this drug will be used to make sure it's correctly covered by Medicare.
Coverage Determination (Part D)
A Coverage Determination (Part D) is a request you submit to us that asks us to decide if a Part D drug prescribed for you can be covered by your plan and/or if the amount you are required to pay is appropriate. You can also use this type of determination to ask for coverage restrictions to be waived.
Organization Determination (Part C)
An Organization Determination (Part C) is a request you submit to us that asks us to decide if a Part C medical service is covered by your plan and/or if the amount you're required to pay is appropriate.
Appoint a representative
You can authorize an individual to act on your behalf. Just download and complete the Appointment of Representative form below. Both you and your representative will need to sign the form.
Legal information about appeals and grievances
For detailed information on how to file a grievance, see Chapter 9 in your Evidence of Coverage (EOC) document. If you don't have Part D coverage, please see Chapter 7 of your EOC document.
