Medicare beneficiary means a Tort Claimant or Unknown Tort Claimant who has received, applied for, or is eligible to receive Medicare or Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
What does Medicare spending per beneficiary mean?
Medicare Spending per Beneficiary (MSPB) below. Beneficiary populations eligible to be included in the MSPB Measure are made up of beneficiaries who were enrolled in both Medicare Parts A and B for the period 93 days prior to IPPS hospital admission until 30 days after discharge from a short-term acute care hospital stay, where the stay occurs
What benefits are covered by Medicare?
Medicare Part B provides coverage and benefits related to general medical care from doctors such as checkups, exams, and necessary durable medical equipment. In addition to the full coverage Medicare Part A and B provide, individuals can enroll in Medicare Part D and take advantage of the programs prescription drug benefits.
What if beneficiary is Medicaid recipient?
Medicaid recipients should contact a Medicaid planner as soon as possible upon knowledge they will be receiving, or have received, an inheritance. In fact, it is highly encouraged one do so prior to reporting the inheritance to the Medicaid agency. Professional Medicaid planners can assist Medicaid beneficiaries in many ways.
What state has the most Medicare recipients?
Top 10 States With the Highest Number of Medicare Beneficiaries
- California — 5 million
- Florida — 3.52 million
- Texas — 3.18 million
- New York — 3.09 million
- Pennsylvania — 2.35 million
- Ohio — 1.97 million
- Illinois — 1.90 million
- Michigan — 1.72 million
- North Carolina — 1.56 million
- New Jersey — 1.37 million

What does it mean to be a Medicare recipient?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What does Medicare beneficiary pay?
Beneficiaries are generally subject to coinsurance for Part A benefits, including extended inpatient stays in a hospital ($315 per day for days 61-90 and $630 per day for days 91-150 in 2015) or skilled nursing facility ($157.50 per day for days 21-100 in 2015).
How many beneficiaries does Medicare have?
Medicare served nearly 63 million beneficiaries in 2019. 62 percent were enrolled in Part A or Part B, and the rest (37 percent) were in Medicare Advantage (Part C). 74 percent were enrolled in Part D drug coverage, 13 percent had private drug coverage, and nearly 9 percent had no drug coverage.
How do I know if I am a Medicare recipient?
Your state's Medicaid office Visit Medicare.gov/contacts, or call 1-800-MEDICARE (1-800-633-4227) and say “Medicaid.” TTY: 1-877-486-2048.
How much do Medicare beneficiaries spend out of pocket on health care?
Medicare Beneficiaries' Spending for Health Care People covered by traditional Medicare paid an average of $6,168 for health care in 2018. They spent almost half of that money (47 percent) on Medicare or supplemental insurance premiums.
Is Medicare free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
How many Medicare beneficiaries are there in 2021?
As of October 2021, the total Medicare enrollment is 63,964,675. Original Medicare enrollment is 36,045,321, and Medicare Advantage and Other Health Plan enrollment is 27,919,354. This includes enrollment in Medicare Advantage plans with and without prescription drug coverage.
What was the purpose of offering Medicare Advantage to Medicare beneficiaries?
While original Medicare has plenty to offer, a market for high-performing, quality private health plans has emerged, giving insurers an incentive to provide optimal, reasonably priced coverage in the form of Medicare Advantage (MA) plans.
Are beneficiaries?
A beneficiary is the person or entity you name in a life insurance policy to receive the death benefit. You can name: One person.
Do you automatically get Medicare with Social Security?
You automatically get Medicare because you're getting benefits from Social Security (or the Railroad Retirement Board). Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
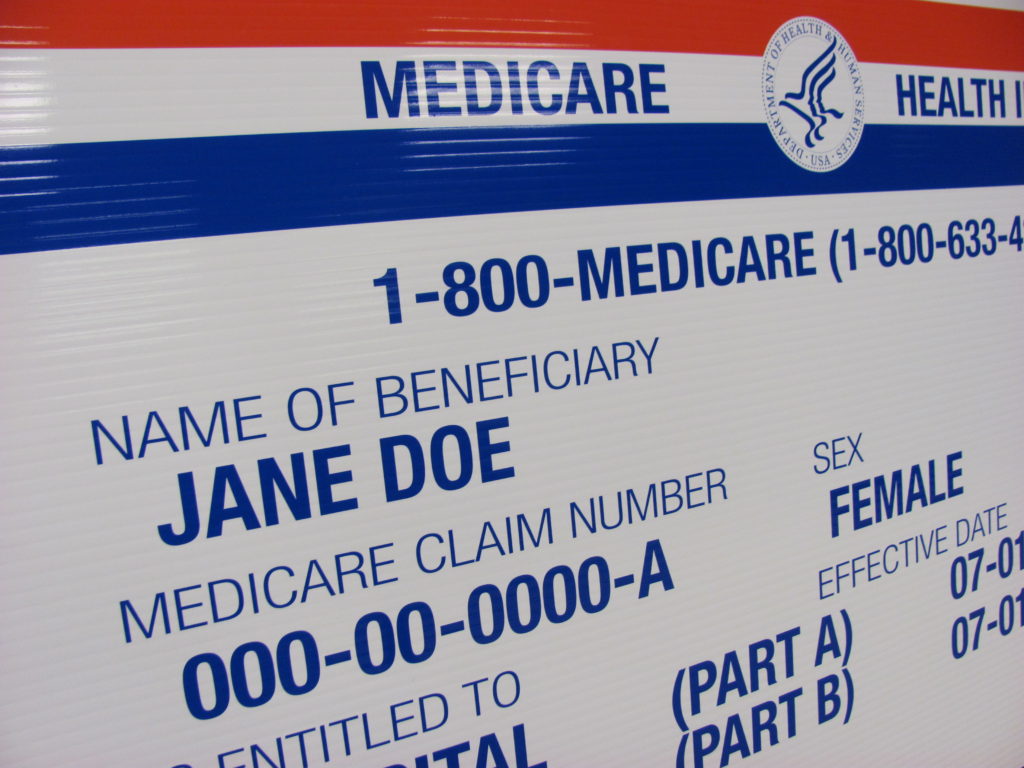
Is your Medicare number the same as your Social Security Number?
Your card has a Medicare Number that's unique to you — it's not your Social Security Number. This helps protect your identity. The card shows: You have Medicare Part A (listed as HOSPITAL), Part B (listed as MEDICAL), or both.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is Medicare beneficiary?
Medicare beneficiary means an individual who is entitled to benefits under medicare part A plan and enrolled under medicare part B plan or enrolled in both medicare part A and part B plan and who resides in the U.S. Medicare beneficiaries pay deductibles and 20 percent coinsurance for most services and equipment.
How long is a Medicare benefit period?
A Medicare beneficiary is entitled to 90 days of Part A coverage for inpatient hospital services for each spell of illness, 42 U.S.C.S. § 1395d [a] [1], which is referred to in the Medicare regulations as a benefit period. 42 CFR 409.61. A spell of illness or benefit period begins on the first day of admission to the hospital and ends on ...
When a health care provider bills Medicare, does it agree to accept the amount that Medicare will pay?
When a health services provider bills medicare, it agrees to accept the amount that medicare will pay, and that once medicare is billed a medicare beneficiary will not be charged either directly or indirectly for items or services that the beneficiary is entitled to have paid.
How many days of Medicare Part A coverage is there?
Whenever admitted to a hospital for a new spell of illness or benefit period, a beneficiary is entitled to another 90 days of Part A coverage. In addition, each Medicare beneficiary has a lifetime reserve of 60 days that the beneficiary may elect to use toward one or more hospital stays. 42 C.F.R. § 409.61 [a] [2].
What happens when Medicare beneficiaries have other health insurance?
When a Medicare beneficiary has other insurance (like employer group health coverage), rules dictate which payer is responsible for paying first. Please review the Reporting Other Health Insurance page for information on how and when to report other health plan coverage to CMS.
What is Medicare for seniors?
Medicare is a health insurance program designed to assist the nation's elderly to meet hospital, medical, and other health costs. Medicare is available to most individuals 65 years of age and older.
What is the CMS?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that manages Medicare. When a Medicare beneficiary has other health insurance or coverage, each type of coverage is called a "payer.". "Coordination of benefits" rules decide which one is the primary payer (i.e., which one pays first). To help ensure that claims are paid ...
How long does it take for Medicare to pay a claim?
When a Medicare beneficiary is involved in a no-fault, liability, or workers’ compensation case, his/her doctor or other provider may bill Medicare if the insurance company responsible for paying primary does not pay the claim promptly (usually within 120 days).
Does Medicare pay a conditional payment?
In these cases, Medicare may make a conditional payment to pay the bill. These payments are "conditional" because if the beneficiary receives an insurance or workers’ compensation settlement, judgment, award, or other payment, Medicare is entitled to be repaid for the items and services it paid.
Examples of Medicare beneficiary in a sentence
However, if the person is a Medicare beneficiary and, as a result of federal law, Medicare is secondary to the plan covering the person as a dependent and primary to the plan covering the person as other than a dependent, then the order of benefits between the two plans is reversed so that the plan covering the person as an employee, Member, policyholder, Subscriber, or retiree is the secondary plan and the other plan is the primary plan..
More Definitions of Medicare beneficiary
Medicare beneficiary. Any person who is a Medicare recipient of Part A or Part A and B and complies with the definition of beneficiary established in this article.
How to contact Medicare.org?
Call us at (888) 815-3313 — TTY 711 to speak with a licensed sales agent.
Does QMB cover Medicare?
It means that your state covers these Medicare costs for you, and you have to pay only for anything that Medicare normally does not cover. QMB does not supplement your Medicare coverage but instead ensures that you will not be precluded from coverage because you cannot afford to pay the costs associated with Medicare.
How To Get Help Paying Your Medicare Premiums And Other Costs
When you first sign up for Medicare, be prepared for some sticker shock. Because youve been paying Medicare taxes all through your working life, you may have assumed that once you retire, all your health care costs will be covered.
Applying For Supplementary Benefits
MSP enrolment must be complete for you to qualify for supplementary benefits. To complete MSP enrolment, submit the MSP Application for Enrolment form and obtain a Photo BC Services Card by visiting an Insurance Corporation of BC driver licensing office.
Applying For Extra Help
Extra Help enrollment is simple. If you are enrolled in Medicare and also receive Medicaid, SSI, or help with Part B premiums from an MSP, youll automatically receive Extra Help benefits.
Medicare Savings Program: Prescription Drug Coverage
While MSPs will help pay for Part A and/or Part B premiums, it does not pay for any costs related to prescription drugs.
Who Qualifies For Medicare Extra Help
You will automatically qualify for Medicare Extra Help if you have Medicare and also meetany of these conditions:
What Is Included In The Medicare Savings Programs Assets Definition
When determining your eligibility for MSP, the following resources are counted:
Specified Low Medicare Beneficiary
The SLMB program provides payment of Medicare Part B premiums only for individuals who would be eligible for the QMB program except for excess income. Income for this program must be more than 100% of the FPL, but not exceed 120% or 135% of the FPL. There is a standard $20 deduction from income, before it is compared to the Federal Poverty Level.
What information is on my Medicare card?
There is additional important information located on your Medicare card for you and your doctor. This includes your name and sex. Additionally, it states whether you have Medicare Part A (inpatient hospital) and Medicare Part B (outpatient medical), and lists the dates that Part A and B first started.
What is a B1 on Medicare?
There are several variations to the B code: B1 is for a husband of a primary beneficiary at age 62 or over. B2 is for a young wife with a child in her care,
What happens if you lose your Medicare card?
If you lose your Medicare card with your number on it, you can request that the Social Security Administration replace your card at no charge. The Medicare Beneficiary Identifier is for claims, billing and identification purposes.
What does it mean when you have an A on your Social Security card?
If you have an A on your card, it means that you are the primary beneficiary. That means you earned Medicare insurance based on your working history and tax credits.
What do the codes after my Social Security number mean?
After the Social Security number, there is a letter and sometimes a number. These codes all have different meanings.
How long does it take for Medicare to arrive in the mail?
After your replacement request, the card typically arrives in the mail in about 30 days, at no cost to the beneficiary. Social Security will mail your Medicare card to the address they have on file for you, so it is important to keep your information with them up to date.
What is a B3 wife?
B3 is for an aged wife over the age of 62 who is a second claimant. B5 is also a second claimant wife, but they are under the age of 62 and have a child in their care. B6 represents a divorced wife over the age of 62. BY is for a young husband with a child in his care.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
What is QMB insurance?
The QMB program pays: The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
Can QMB members pay for coinsurance?
Providers can’t bill QMB members for their deductibles , coinsurance, and copayments because the state Medicaid programs cover these costs. There are instances in which states may limit the amount they pay health care providers for Medicare cost-sharing. Even if a state limits the amount they’ll pay a provider, QMB members still don’t have to pay Medicare providers for their health care costs and it’s against the law for a provider to ask them to pay.
Does Medicare Advantage cover dual eligibility?
A Medicare Advantage Special Needs Plan for dual-eligible individuals could be a fantastic option. Generally, there is a premium for the plan, but the Medicaid program will pay that premium. Many people choose this extra coverage because it provides routine dental and vision care, and some come with a gym membership.
Is Medigap coverage necessary for QMB?
Medigap coverage isn’t necessary for anyone on the QMB program. This program helps you avoid the need for a Medigap plan by assisting in coverage for copays, premiums, and deductibles. Those that don’t qualify for the QMB program may find that a Medigap plan helps make their health care costs much more predictable.