When to use RT and rtlt modifiers?
The right (RT) and left (LT) modifiers must be used when billing two of same item or accessory on the same date of service and the items are being used bilaterally. Current instructions for billing products to be used bilaterally instruct suppliers to use the RTLT modifier on the same claim line and indicate two (2) units of service.
What are some examples of Revenue Codes in medical billing?
Examples of Revenue Codes- 1) – 0450- Emergency Room Service 2) – 0290- Durable medical equipment Revenue codes in medical billing used in hospital billing or institutional claim and used on UB-04 only.
Why is Medicare not accepting the [50] modifier?
Some payors don't accept the [50] modifier, but want RT / LT instead. Medicare usually wants Modifier 50 and billed on 1 line, the quantity is one but you double the price. If you bill it on separate lines and do not double the price they usually pay wrong. Their manual states you can do either way, modifier 50 on one line or RT/LT.

What is RT in medical coding?
rightThe right (RT) and left (LT) modifiers must be used when billing two of same item or accessory on the same date of service and the items are being used bilaterally.
Does Medicare accept RT and LT modifiers?
If the service is submitted using a modifier 50 or the RT/LT or two units of service, then Medicare will allow the fee schedule for both services. Apply the multiple surgery rules prior to applying the multiple payment reduction rules.
How does risk adjustment work?
Risk adjustment accomplishes this by transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. The goal of the risk adjustment program is to encourage insurers to compete based on the value and efficiency of their plans rather than by attracting healthier enrollees.
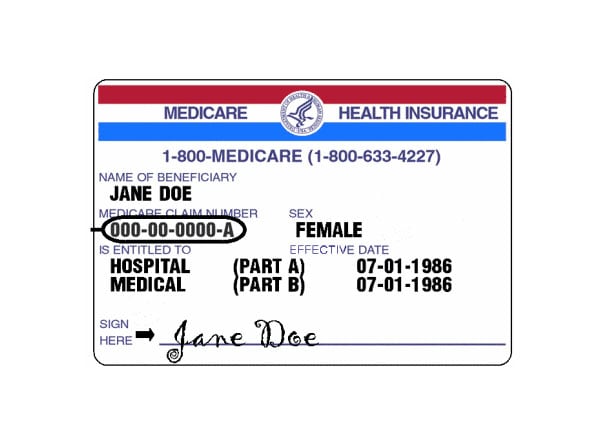
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is a RT modifier used for?
Right side (used to identify procedures performed on the right side of the body). Refer to the Medicare Physician Fee Schedule database (MPFSDB) to determine if HCPCS modifier RT is applicable to a particular procedure code.
Does modifier 59 go before RT?
Contributor. different shoulders, modifiers RT and LT should be used, not modifier 59. LT and RT have not effect on the actual processing of the claim for payment, because they are informational.
How does risk adjustment benefit patients?
In its simplest terms, risk adjustment ensures that the health conditions, health status, and demographics of the beneficiaries in a Medicare Advantage or an Affordable Care Act plan are accurately documented—and that the health plans managing those beneficiaries are adequately compensated for that management.
How does risk adjustment affect patients?
Risk adjustment modifies payments to all insurers based on an expectation of what the patient's care will cost. For example, a patient with type 2 diabetes and high blood pressure merits a higher set payment than a healthy patient, for example.
What is a Medicare risk score?
Using the Medicare risk adjustment factor system a “risk score” is chosen for each beneficiary according to the patient's demographics, health status, and other clinical factors. The beneficiary's risk score depicts the patient's predicted health costs compared to those of an average beneficiary.
What is Medicare Part C called?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
What are the 2 types of Medicare plans?
Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). You can join a separate Medicare drug plan to get Medicare drug coverage (Part D). You can use any doctor or hospital that takes Medicare, anywhere in the U.S.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
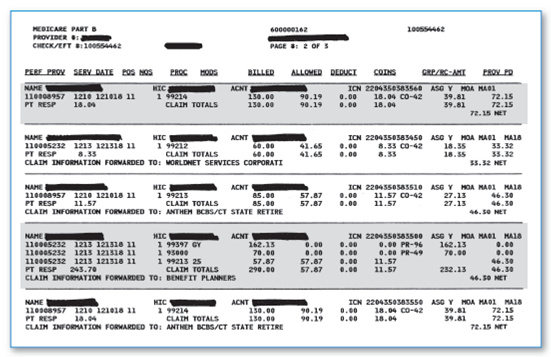
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.
Instructions
Used to identify procedures performed on right side of body. Refer to Medicare Physician Fee Schedule database (MPFSDB) to determine if HCPCS modifier RT is applicable to a particular procedure code
Correct Use
When body contains a right and left anatomical part of body and a service is performed on right anatomical part
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Language quoted from the Centers for Medicare & Medicaid Services (CMS) National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
Article Guidance
The following coding and billing guidance is to be used with its associated Local Coverage Determination.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How many lines are RT and LT?
Rt and LT are anatomic modifiers and you are allowed only one anatomic modifier per line item so use two lines when reporting RT and LT. Technically RT and LT are for facility outpatient and ASC use however many payers do accept them for physician claims due to the clarity they provide.
Does United Health Care recognize modifier 50?
They do recognize modifier 50 for reimbursement reasons. It is just an informational modifier. United Health Care still wants Modifier 50 per their website: "Modifier 50identifies the same procedures that are performed as a bilateral service.
Can Medicare pay modifier 50 on one line?
Medicare usually wants Modifier 50 and billed on 1 line, the quantity is one but you double the price. If you bill it on separate lines and do not double the price they usually pay wrong. Their manual states you can do either way, modifier 50 on one line or RT/LT. But also, watch out, they do have some LCD's/LMRP's that direct you to a certain way.
Does Medicare pay with modifier 50?
Medicare guidelines will tell you to bill with modifier 50 for bilateral procedures. However, I found that the normally pay incorrectly with the 50 modifier. I always use the LT and RT modifiers for all insurance companies.