Deemed status is given by Centers for Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
When did the Joint Commission lose its deemed status?
The Medicare Improvements for Patients and Providers Act of 2008 removed the deemed status of the Joint Commission and directed it to re-apply to CMS to seek continued authority to review hospitals for CfC and CoP. ^ Joint Commission (August 1, 2014).
What is the difference between Joint Commission and CMS?
However, if a national accrediting organization such as the Joint Commission has and enforces standards that meet the federal CoPs, CMS may grant the accrediting organization "deeming" authority and "deem" each accredited health care organization as meeting the Medicare and Medicaid certification requirements.
What does deemed status mean for health care organizations?
The health care organization would have "deemed status" and would not be subject to the Medicare survey and certification process because it has already been surveyed by the accrediting organization. Accreditation is voluntary and seeking deemed status through accreditation is an option, not a requirement.
What is the Joint Commission in healthcare accreditation?
National accrediting agencies, such as the Joint Commission, serve to evaluate healthcare organizations and ensure that safety and quality of care are adequate. What is the Joint Commission?
What is Joint Commission accreditation?
The Joint Commission’s accreditation and certification programs are widely relied upon by at least one agency in each state, across multiple provider types, in making licensure decisions, as well as for participation in a state’s Medicaid program. The most common form of state reliance on accreditation is to accept The Joint Commission’s survey process in lieu of the state agency conducting a routine licensure inspection. In addition, some state regulations will mandate accreditation as a condition of licensure or certification. The Joint Commission actively monitors state legislative and regulatory activities to identify additional opportunities for state reliance on Joint Commission accreditation and certification, and maintains a website listing the state regulations that contain such provisions.
How to check federal deemed status?
Federal deemed status by calling The Joint Commission at 630-792-5799.
Is Joint Commission survey included in annual cost report?
CMS has determined that fees for Joint Commission surveys may be included in a health care organization’s costs on its annual cost report for those organizations required to file cost reports.
What is considered a CMS?
Deemed Status for Medicare and Medicaid Providers. The Centers for Medicare and Medicaid Services (CMS) requires long-term care facilities to meet certain federal standards, known as the requirements of participation, in order to begin or continue to participate in and receive payment from the Medicare and Medicaid programs.
What are the penalties for not complying with CMS standards?
If a state survey agency determines during an inspection that a facility is not compliant with these standards, then CMS may impose penalties such as civil money penalties, suspension of payment for all new admissions, and/or directed plans of correction on the non-compliant facility.
Can a health care organization be accredited?
National accrediting organizations may grant health care organizations accreditation if the health care organization completes a voluntary process where they are surveyed by the accrediting organization's staff and the staff determine that the entity provides quality services.
Can CMS terminate a facility?
Should a facility continue to be found non-compliant with the requirements of participation, CMS may terminate the facility's participation in the Medica re and Medica id programs.
Can long term care facilities be deemed?
Long-term care facilities are not currently eligible to receive deemed status. However, recent actions by CMS to clairfy and strengthen oversight of accrediting organizations (in a proposed rule released in April 2013) have led some advocates to believe that CMS is considering expanding the role of accrediting organizations by granting them deeming authority for long-term care facilities. Allowing private accrediting organizations to determine the quality of care and quality of life residents are receiving would undoubtedly compromise resident safety and result in poorer care and greater instances of abuse and neglect in long-term care facilities.
Who is the Joint Commission?
The Joint Commission is designated by the Centers for Medicare and Medicaid Services (CMS) as an approved accreditor for home health and hospice agencies seeking Medicare certification, and can provide accreditation and Medicare certification simultaneously through its survey process.
What is Joint Commission accreditation?
Joint Commission accreditation has been approved by many states as an option for organizations seeking initial licensure and re-licensure. This recognition applies to a wide variety of home and community-based providers offering services such as home health, hospice, pharmacy, and personal care.
When does a home infusion therapy provider have to be accredited?
Any home infusion therapy supplier that wishes to obtain Medicare reimbursement for the nursing component of that service must be accredited by January 1, 2021. The Joint Commission has been awarded deeming authority by CMS and is now accepting applications for accreditation.
Does CMS have a final decision?
CMS, not The Joint Commission, grants the final decision for Medicare certification. System accreditation awards a single accreditation decision to a Home Care “system”, usually a large organization, composed of a corporate office or a main site, and multiple sites that share a common governance structure and corporate management.
Is CMS accreditation voluntary?
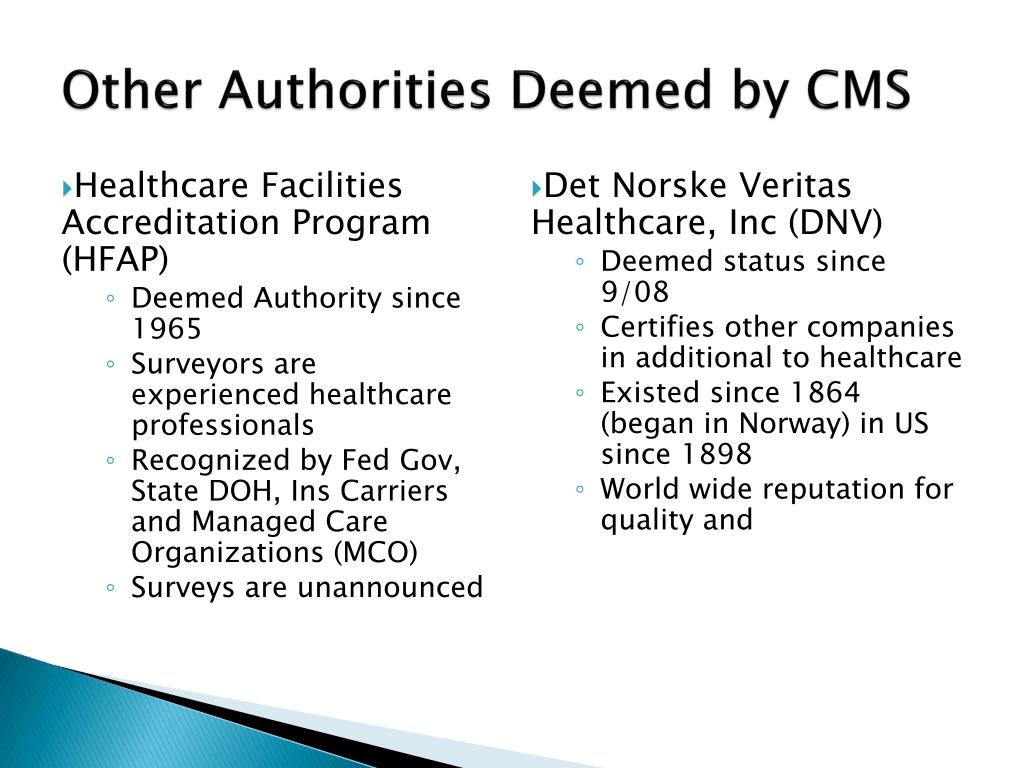
Accreditation is voluntary and seeking deemed status through accreditation is an option, not a requirement . Organizations seeking CMS approval may choose to be surveyed either by an accrediting body, such as the Joint Commission, DNV, and HFAP, or by state surveyors on behalf of CMS.
Does CMS deem a health care organization?
However, if a national accrediting organization such as the Joint Commission has and enforces standards that meet the federal CoPs, CMS may grant the accrediting organization "deeming" authority and "deem" each accredited health care organization as meeting the Medicare and Medicaid certification requirements. The health care organization would have "deemed status" and would not be subject to the Medicare survey and certification process because it has already been surveyed by the accrediting organization.
How many hospitals were eligible for CMS funding in 1994?
In 1994 about 5000 hospitals were eligible to receive CMS funding as a result of being reviewed by the Joint Commission. The Medicare Improvements for Patients and Providers Act of 2008 removed the deemed status of the Joint Commission and directed it to re-apply to CMS to seek continued authority to review hospitals for CfC and CoP.
What are the two types of organizations that can review a health care provider?
Two kinds of organizations can review a health care provider to check for compliance with these conditions - either a state level agency acting on behalf of CMS, or a national accreditation agency like the Joint Commission.
Why are the standards for care for nursing homes distributed?
The standards for care for nursing homes were distributed as a result of the Nursing Home Reform Act. Outpatient clinics cannot receive deemed status. A consequence of this is that the CMS payment systems can be more complicated at small clinics than at large hospitals for the same procedures. Conditions for Coverage and Conditions ...
What is the Joint Commission?
An independent, nonprofit organization, The Joint Commission is the nation’s oldest and largest standards-setting and accrediting body in health care.
When did the Joint Commission start accreditation?
The Joint Commission launched its Ambulatory Care Accreditation Program in 1975 and currently accredits more than 2,200 freestanding ambulatory care organizations. Joint Commission surveyors are experts in their field.
When was the Joint Commission founded?
Founded in 1951 , The Joint Commission seeks to continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value.
Is CMS accreditation voluntary?
Accreditation is voluntary and seeking deemed status through accreditation is an option. Organizations seeking deemed status may choose to be surveyed either by an accrediting organization or state surveyors on behalf of CMS. All deemed status surveys are unannounced.