What is the criteria for ESRD?
End-stage renal disease usually occurs when kidney function is less than 15% of typical kidney function. As a part of kidney disease staging, your provider also might test whether you have protein in your urine.Oct 12, 2021
How long does ESRD Medicare last?
When a patient has a kidney transplant, ESRD-based Medicare coverage continues for 36 months after the month of the successful transplant.
What is the difference between CKD and ESRD?
If left untreated, CKD can progress to kidney failure and early cardiovascular disease. When the kidneys stop working, dialysis or kidney transplant is needed for survival. Kidney failure treated with dialysis or kidney transplant is called end-stage renal disease (ESRD).
Are all patients with ESRD covered by Medicare?
Not all individuals with ESRD are eligible for Medicare. In addition to ESRD, one of the following criteria must be met: 1. The individual must meet the required work credits under Social Security, Railroad Retirement or as a government employee 2.
When is ESRD Medicare primary?
If you have ESRD and need dialysis (also known as 'hemodialysis'), your Medicare coverage starts the first day after the 3rd full month of dialysis in a clinic.
When does Medicare start for ESRD?
Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. This 4-month waiting period will start even if you haven't signed up for Medicare.
Can you code ESRD and CKD together?
Per the Official Guidelines for Coding and Reporting, Section I.C. 14a. 1, If both a stage of CKD and ESRD are documented, the coding professional would assign code N18. 6 (ESRD) only.Sep 27, 2018
Is chronic kidney disease stage 5 the same as ESRD?
The final stage of chronic kidney disease (CKD) is referred to as stage 5 CKD, end-stage kidney disease (ESKD), and end-stage renal disease (ESRD). At this stage, your kidneys are about to fail, or you're already in kidney failure.
Is Stage 5 kidney disease the same as ESRD?
Stage 5 kidney disease, or end stage renal disease (ESRD), occurs when your estimated glomerular filtration rate (eGFR) falls below 15, indicating that your kidneys are failing or close to failing.
Why was ESRD added to Medicare?
Congress changed the Medicare ESRD Program on June 13, 1978 (PL 95-292) to improve cost-effectiveness, ensure quality of care, encourage kidney transplantation and home dialysis, and increase program accountability.Jun 18, 2012
Do dialysis patients qualify for Medicare?
People who need dialysis are not eligible to sign up for Medicare (Parts A and B) until the day they begin dialysis. Once they sign up, Medicare will be effective at the beginning of their fourth month of dialysis and will start paying for their treatment if they choose in-center hemodialysis.Sep 27, 2016
How Much Does Medicare pay for dialysis?
Medicare costs for dialysis treatment and supplies If you have Original Medicare, you'll continue to pay 20% of the Medicare-approved amount for all covered outpatient dialysis-related services, including those related to self-dialysis. Medicare will pay the remaining 80%.Aug 6, 2021
How long does it take for Medicare to start if you have ESRD?
If you’re eligible for Medicare based on ESRD and don’t sign up right away, your coverage could start up to 12 months before the month you apply.
How to contact ESRD?
Call your ESRD Network for more information. You can also call us at 1-800-MEDICARE (1-800-633-4227) to get: Your ESRD Network's contact information. More information about getting dialysis in a disaster or emergency. If you have a Medicare Advantage Plan or other Medicare health plan:
How long does it take for Medicare to cover a transplant?
If your transplant is delayed more than 2 months after you’re admitted to the hospital (for the transplant or for health care services you need before your transplant), Medicare coverage can begin 2 months before your transplant.
How does Medicare Advantage work?
Medicare Advantage Plans are a type of Medicare health plan offered by a private company that contracts with Medicare to provide all your Part A and Part B benefits. Most Medicare Advantage Plans also offer drug coverage.
When does Medicare start for permanent kidney failure?
How other coverage works with Medicare. If you’re eligible for Medicare only because of permanent kidney failure, your coverage usually can’t start until the fourth month of dialysis (also known as a “waiting period”).
When does Medicare start covering kidney transplants?
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
When does Medicare start paying for dialysis?
Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. This 4 month waiting period will start even if you haven’t signed up for Medicare. Example: if you start dialysis on July 1, your coverage will begin on October 1, even if you don’t sign up for Medicare until December 1.
When does Medicare start ESRD?
When you enroll in Medicare based on ESRD and you’re on dialysis, Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. For example, if you start dialysis on July 1, your coverage will begin on October 1.
When does Medicare start covering kidney transplants?
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
What is assignment in Medicare?
Assignment—An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare cover home dialysis?
Medicare Part B covers training for home dialysis, but only by a facility certifed for dialysis training. You may qualify for training if you think you would benefit from home dialysis treatments, and your doctor approves. Training sessions occur at the same time you get dialysis treatment and are limited to a maximum number of sessions.
Does Medicare cover dialysis for children?
Your child can also be covered if you, your spouse, or your child gets Social Security or RRB benefits, or is eligible to get those benefits.Medicare can help cover your child’s medical costs if your child needs regular dialysis because their kidneys no longer work, or if they had a kidney transplant.Use the information in this booklet to help answer your questions, or visit Medicare.gov/manage-your-health/i-have-end-stage-renal-disease-esrd/children-end-stage-renal-disease-esrd. To enroll your child in Medicare, or to get more information about eligibility, call or visit your local Social Security oce. You can call Social Security at 1-800-772-1213 to make an appointment. TTY users can call 1-800-325-0778.
Does Medicare cover pancreas transplant?
If you have End-Stage Renal Disease (ESRD) and need a pancreas transplant, Medicare covers the transplant if it’s done at the same time you get a kidney transplant or it’s done after a kidney transplant.
What is ESRD 2021?
February 2021. Medicare for People with End-Stage Renal Disease (ESRD) Under the direction of CMS, the ESRD Network program is a national network of 18 ESRD Networks, responsible for each U.S. state, territory, and the District of Columbia.
When does Medicare start for end stage renal disease?
Medicare for People with End-Stage Renal Disease (ESRD) Medicare coverage usually starts on the 1st day of the 4th month of a regular course of dialysis. Coverage can begin the first month of a regular course of dialysis treatments if you meet all of these conditions:
What is Medicare materials?
The materials are for information givers/trainers who are familiar with the Medicare Program, and who use the information for their presentations.
Key Takeaways
Original Medicare (Parts A and B) covers most of the treatment you’ll need with end-stage renal disease (ESRD), including medical services and supplies in hospitals, doctors’ offices and at home.
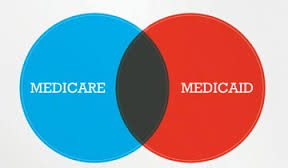
Does Medicare Cover ESRD?
Original Medicare as well as Medicare Advantage covers end-stage renal disease.
Do you have to Sign Up for Medicare if you have ESRD?
You need both Parts A and B of Original Medicare to take advantage of the extensive coverage offered by Medicare. Having both Parts A and B also opens up the option to switch to a Medicare Advantage plan, which replaces Original Medicare while providing at least the same coverage as Parts A and B.
Is Medicare Primary for ESRD?
If you are eligible for Medicare because of ESRD but continue with your group health plan, Medicare would pay secondary to your primary group health plan insurance during your 30-month coordination period.
How do I get Medicare for End-stage Renal Disease?
Medicare coverage usually starts on the first day of the fourth month of your dialysis treatments. Still, the waiting period begins even if you haven’t yet signed up for Medicare, and your coverage can be retroactive.
FAQs
Yes, Medicare covers kidney transplants as long as the surgery is performed at a Medicare-approved hospital. Medicare will cover you for 36 months after the month you receive a kidney transplant. After that time, you will not be covered by Medicare to pay for your immunosuppressive drugs.
What is ESRD in Medicare?
End stage renal disease (ESRD) is also known as permanent kidney failure. With this condition, your kidneys can no longer function on their own and you need regular dialysis or a kidney transplant. Medicare provides medical coverage for eligible people of all ages with ESRD.
When will ESRD be available for Medicare?
If you want to switch from original Medicare to a Medicare Advantage plan, you will be able to do so during the annual open enrollment period, which takes place from October 15 through December 7.
How long does ESRD last?
If you only have Medicare because you have ESRD, your coverage will end 12 months after you stop dialysis treatment or 36 months after you have a kidney transplant.
How long do you have to be on dialysis to qualify for Medicare?
citizens or permanent residents who have lived here for at least 5 continuous years. Your eligibility for Medicare will begin 3 months after the date you start regular dialysis or receive a kidney transplant.
Does Medicare cover all medications?
Some medications not covered under original Medicare are covered by Medicare Part D. Part D is an optional prescription drug plan you can purchase from an insurance company. Not all Part D plans cover the same medications, although every plan is required to provide a standard level of coverage established by Medicare.
Does Medicare Part C cover prescriptions?
Medicare Part C. If you have Medicare Advantage (Part C), your plan will cover at least everything that original Medicare does. It may also cover prescription medications that are not covered by Medicare Part B. Part C plans usually require that you use in-network providers and pharmacies.
Does Medicare cover ESRD?
Medicare covers people of all ages who have ESRD, including children. To be eligible, you must be on regular dialysis or have had a kidney transplant. Dialysis and kidney transplants are covered under Medicare. Even with Medicare, out-of-pocket costs for ESRD treatments and medications may be high, but there are additional coverage options.
What is Medicare for seniors?
Medicare Program. Medicare is the federal health insurance program for people age 65 and older or people with certain disabilities.
What is Medicare for people 65 and older?
What is Medicare Program? Medicare is health insurance for people 65 or older, people under 65 with certain disabilities, and people of any age with End-Stage Renal Disease (ESRD) (permanent kidney failure requiring dialysis or a kidney transplant). When you first enroll in Medicare, you’ll have Original Medicare, unless you make another choice.
Is Medicare for people over 65?
Look up helpful websites and phone numbers. Medicare is health insurance for people 65 or older, people under 65 with certain disabilities, and people of any age with End-Stage Renal Disease (ESRD) (permanent kidney failure requiring dialysis or a kidney transplant).
How long is the ESRD coordination period?
Note: The 30-month coordination period applies to people with ESRD Medicare only. If you have Medicare due to age or disability before developing an ESRD diagnosis, the normal rules for Medicare’s coordination with other insurances apply. If your ESRD Medicare coverage ends and later resumes, you start a new 30-month coordination period ...
When does Medicare become primary?
Instead, you will have to wait to enroll until the General Enrollment Period (GEP) and will likely face gaps in coverage and a late enrollment penalty. Once your 30-month coordination period ends , Medicare automatically becomes primary and your GHP coverage secondary.
What happens if you delay Medicare enrollment?
If you choose to delay ESRD Medicare enrollment, you should turn down both Part A and Part B. This is because if you enroll in Part A and delay Part B, you lose your right to enroll at any time during the 30-month coordination period.
Can you end Cobra after enrolling in ESRD?
Additional rules for coordinating ESRD Medicare and COBRA. If you have COBRA first and then enroll in ESRD Medicare, your employer can choose to end your COBRA coverage—though not all employers end COBRA after you enroll in ESRD Medicare. Speak to your employer before making enrollment decisions.
Does Medicare cover ESRD?
ESRD care is typically expensive, and Medicare may cover your cost-sharing (deductibles, copayments, coinsurances). If you enroll in ESRD Medicare at the start of your 30-month coordination period, Medicare should automatically become the primary payer once the period is over.
Does X have to enroll in Medicare?
X does not enroll in Medicare until June 2018, but his 30-month coordination period still began on December 1, 2017. You may want to enroll in ESRD Medicare even though your GHP pays primary during the 30-month coordination period. ESRD care is typically expensive, and Medicare may cover your cost-sharing (deductibles, copayments, coinsurances).
Does ESRD pay for GHP?
Your GHP coverage must pay first, and ESRD Medicare may pay second for your health care costs. If you do not have other insurance, ESRD Medicare will pay primary as soon as you enroll. The 30-month coordination period begins when eligibility for ESRD Medicare begins, even if you haven’t signed up for ESRD Medicare yet.
