20% deduction from Earned Income Standard deduction of $177 for households with 1 to 3 people and $184 for households with 4 or more people Dependent care deduction when needed for work, training, or education A deduction for elderly or disabled members medical expenses that exceed $35 a month
Full Answer
What is the Medicare income limit for Medicare?
There are no Medicare income limits that pertain to eligibility, but income can decide some monthly costs. Those with higher incomes must pay higher monthly premiums for two Medicare programs.
What is the maximum income to qualify for Medicaid as a couple?
For a married couple who is living together, the limit is $25,860. When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted.
What are the income guidelines for adult foster care?
Income guidelines for adult foster care are below. If one lives at home $1,224 / month. For income guidelines for adult foster care, see below. No set income limit. Income over $62 / month must be paid towards one’s cost of care. No set income limit. Income over $62 / month (per spouse) must be paid towards one’s cost of care. No set income limit.
What are the income limits for Medicare in 2022?
Healthline.com will update this article with 2022 plan information once it is announced by the Centers for Medicare & Medicaid Services (CMS). There are no income limits to receive Medicare benefits. You may pay more for your premiums based on your level of income.

What are the Medicare income brackets for 2020?
How much will I pay for premiums in 2022?Yearly income in 2020: singleYearly income in 2020: married, joint filing2022 Medicare Part B monthly premium≤ $91,000≤ $182,000$170.10> $91,00–$114,000> $182,000–$228,000$238.10> $114,000–$142,000> $228,000–$284,000$340.20> $142,000–$170,000> $284,000–$340,000$442.302 more rows•Nov 16, 2021
What is the highest income to qualify for Medicare?
Summary: There is no income limit for Medicare. But there is a threshold where you might have to pay more for your Medicare coverage. In 2022,Medicare beneficiaries with a modified adjusted gross income above $91,000 may have an income-related monthly adjustment (IRMAA) added to their Medicare Part B premiums.
What is the Medicare MAGI for 2021?
In 2021, the adjustments will kick in for individuals with modified adjusted gross income above $88,000; for married couples who file a joint tax return, that amount is $176,000. For Part D prescription drug coverage, the additional amounts range from $12.30 to $77.10 with the same income thresholds applied.
How do I calculate my income for Medicare?
Your MAGI is calculated by adding your AGI to any of your other income. This includes untaxed foreign income, non-taxable Social Security benefits, tax-exempt interest, and income from within the US territories not already included in your AGI. For most individuals, your MAGI will be the same as your AGI.
Does your income affect how much you pay for Medicare?
If you file your taxes as “married, filing jointly” and your MAGI is greater than $182,000, you'll pay higher premiums for your Part B and Medicare prescription drug coverage. If you file your taxes using a different status, and your MAGI is greater than $91,000, you'll pay higher premiums.
Is Medicare premium based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
What is the Medicare premium cost for 2021?
$148.50 forThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
How do I calculate Magi?
To calculate your MAGI:Add up your gross income from all sources.Check the list of “adjustments” to your gross income and subtract those for which you qualify from your gross income. ... The resulting number is your AGI.More items...
What year income is used to determine Medicare premiums?
We use your modified adjusted gross income (MAGI) from your federal income tax return to determine your income-related monthly adjustment amounts. Your MAGI is the total of your adjusted gross income and tax-exempt interest income.
How is household income calculated?
Household monthly income per person is calculated by taking the total gross household monthly income [1] divided by the total number of family members [2] living together.
Who is not eligible for Medicare?
Did not work in employment covered by Social Security/Medicare. Do not have 40 quarters in Social Security/Medicare-covered employment. Do not qualify through the work history of a current, former, or deceased spouse.
What are Medicare income limits?
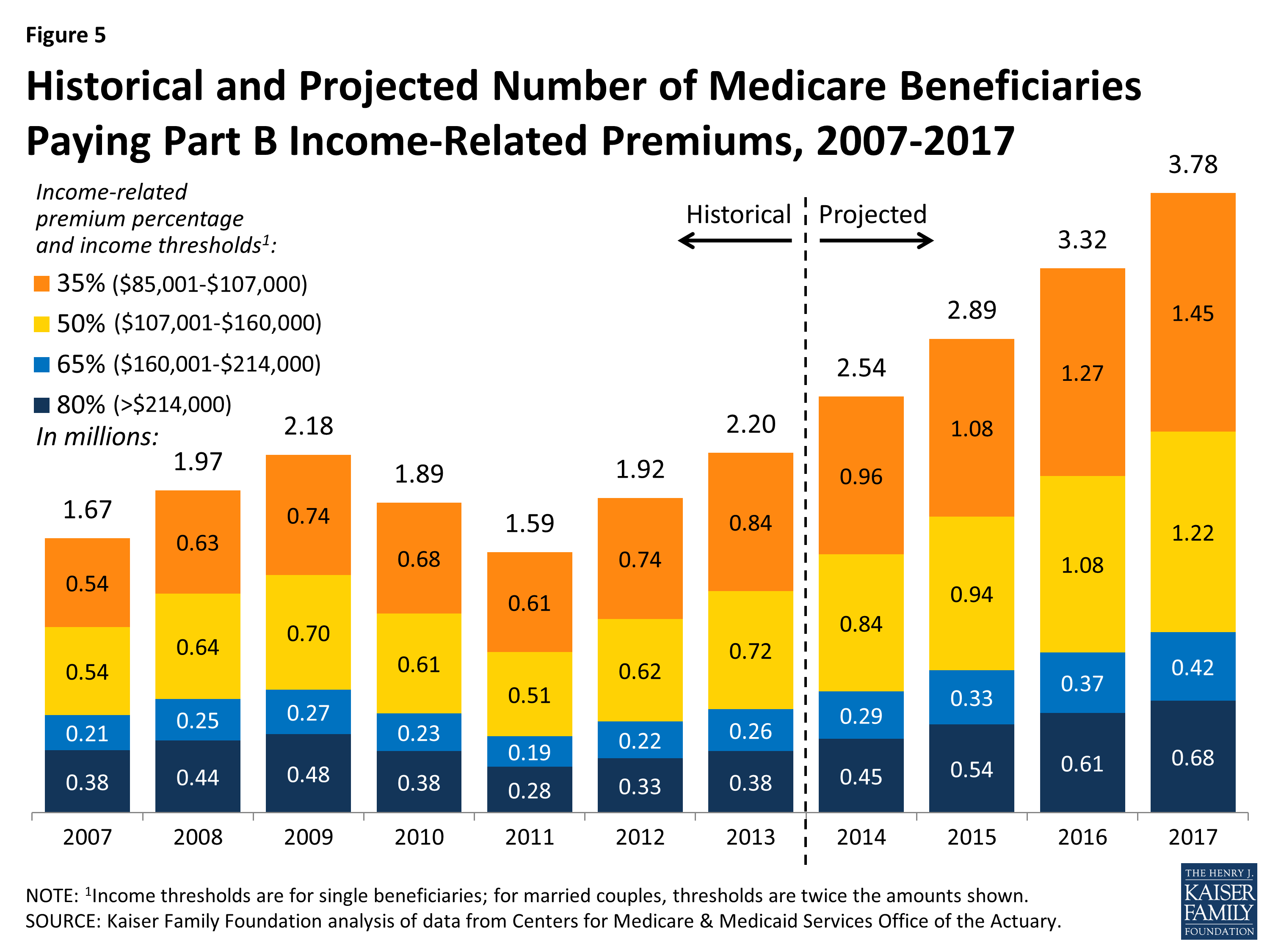
Medicare beneficiaries with incomes above a certain threshold are charged higher premiums for Medicare Part B and Part D. The premium surcharge is...
Why does Medicare impose income limits?
The higher premiums for Part B took effect in 2007, under the Medicare Modernization Act. And for Part D, they took effect in 2011, under the Affor...
Who is affected by the IRMAA surcharges and how does this change over time?
There have been a few recent changes that affect high-income Medicare beneficiaries: In 2019, a new income bracket was added at the high end of the...
Will there be a rate increase in 2022?
We don’t yet have concrete details from CMS. But the Medicare Trustees Report, which was published in late August, projects that the standard Part...
How much does Medicare pay for Part D?
If you earn more than $88,000 but less than $412,000, you’ll pay $70.70 on top of your plan premium. If you earn $412,000 or more, you’ll pay $77.10 in addition to your plan premium. Medicare will bill you for the additional Part D fee every month.
What is the income limit for QDWI?
You must meet the following income criteria if you want to enroll in your state’s QDWI program: Individuals must have a monthly income of $4,339 or less and a $4,000 resource limit. A married couple’s monthly income must be less than $5,833. A married couple’s resource limit must be less than $6,000.
What is SLMB in Medicare?
SLMB, or Specified Low-Income Medicare Beneficiary. If you earn less than $1,296 per month and have less than $7,860 in assets, you may be eligible for SLMB. Married couples must make less than $1,744 per month and have less than $11,800 in debt to qualify. This plan covers your Part B premiums.
What happens if you retire in 2020 and only make $65,000?
Loss of income from another source. If you were employed in 2019 and earned $120,000 but retired in 2020 and now only make $65,000 from benefits, you may want to challenge your IRMAA. To keep track of your income fluctuations, fill out the Medicare Income-Related Monthly Adjustment Amount – Life-Changing Event form.
How much do you have to pay in taxes if you make more than $412,000 a year?
If you earn more than $412,000 per year, you’ll have to pay $504.90 per month in taxes. Part B premiums will be cut off directly from your Social Security or Railroad Retirement Board benefits. Medicare will send you a fee every three months if you do not receive either benefit.
How much will Part D cost in 2021?
Through the Extra Help program, prescriptions can be obtained at a significantly reduced cost. In 2021, generic drugs will cost no more than $3.70, while brand-name prescriptions will cost no more than $9.20.
How much do you have to pay for Part B?
If this is the case, you must pay the following amounts for Part B: If you earn less than $88,000 per year, you must pay $148.50 per month. If you earn more than $88,000 but less than $412,000 per year, you must pay $475.20 per month.
What are the two Medicare programs that require higher monthly premiums?
Those with higher incomes must pay higher monthly premiums for two Medicare programs. These include Part B , which is the outpatient medical coverage of original Medicare, and Part D , the program that provides prescription drug coverage. This article discusses the parts of Medicare that higher premiums may, or may not, affect.
What is the standard rate for Medicare 2021?
The majority of people fall into the income range associated with the standard rate, which in 2021 is $148.50. This amount can change each year.
How does Medicare determine premiums?
To determine the premiums it assigns, Medicare uses someone’s federal tax return from the Internal Revenue Service (IRS). In figuring the premiums of beneficiaries for 2021, Medicare uses tax returns from 2019, which is the most recent year the IRS provides to Social Security. Most of the income thresholds for premium adjustments are subject ...
What is Medicare supplement insurance?
This plan combines the benefits of original Medicare parts A and B into one policy. Medigap, which is Medicare supplement insurance. This plan is available for purchase to a person with original Medicare. Private insurance companies administer both Medicare Advantage and Medigap plans.
How to appeal Medicare premium adjustment?
If an individual does not agree with Medicare’s decision about their income-related premium adjustment, they can file an appeal. To do this, a person may call Social Security at 800-772-1213. A deaf or partially deaf person may call 877-486-2048.
Does Medicare have to adjust premiums based on income?
Medicare bases the adjustments on a person’s modified adjusted gross income, which is the total of adjusted gross income and tax-exempt interest income.
Can income be high for Medicare?
A person’s income cannot be so high that it disqualifies them for Medicare. Even those who receive very high incomes may enroll. However, individuals with higher incomes pay higher premiums for parts B and D, but Medicare income limits that affect premium rates only affect a small percentage of people.
What is the Medicare Advantage spending limit?
Medicare Advantage (Medicare Part C) plans, however, do feature an annual out-of-pocket spending limit for covered Medicare expenses. While each Medicare Advantage plan carrier is free to set their own out-of-pocket spending limit, by law it must be no greater than $7,550 in 2021. Some plans may set lower maximum out-of-pocket (MOOP) limits.
How many reserve days do you get with Medicare?
Medicare limits you to only 60 of these days to use over the course of your lifetime, and they require a coinsurance payment of $742 per day in 2021. You only get 60 lifetime reserve days, and they do not reset after a benefit period or a calendar year.
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
What happens if you spend $6,550 out of pocket in 2021?
After you spend $6,550 out-of-pocket on covered drugs in 2021, you leave the donut hole coverage gap and enter the catastrophic coverage stage. Once you reach this stage, you only pay a small coinsurance or copayment for your covered drugs for the rest of the year.
What is Medicare Part B and Part D?
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
What is the income limit for extra help in 2021?
What Are the Income and Resource Limits for Extra Help in 2021? In 2021, the annual income limit for Extra Help for an individual is $19,140. For a married couple who is living together, the limit is $25,860. When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted.
How much does extra help save?
On average, Extra Help is estimated to save beneficiaries $5,000 in these costs per year. If you’re eligible for Medicaid or any of the following Medicare Savings Programs, you automatically qualify for Extra Help. Qualified Medicare Beneficiary (QMB)
Can you mail a color coded document to Medicare?
You can mail your color-coded document to your Part D plan to help verify the level of Extra Help for which you qualify. Those who are dual-eligible to receive Medicare and Medicaid qualify for full Extra Help.
Is food stamps counted as extra help?
When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted. Even if your income is higher than the limits, you should still apply for Extra Help if you think you qualify. Some scenarios where you’d still be eligible for Extra Help even though your income is over ...
How many credits can you earn on Medicare?
Workers are able to earn up to four credits per year. Earning 40 credits qualifies Medicare recipients for Part A with a zero premium.
What is the premium for Part B?
Part B premium based on annual income. The Part B premium, on the other hand, is based on income. In 2020, the monthly premium starts at $144.60, referred to as the standard premium.
How does Medicare affect late enrollment?
If you do owe a premium for Part A but delay purchasing the insurance beyond your eligibility date, Medicare can charge up to 10% more for every 12-month cycle you could have been enrolled in Part A had you signed up. This higher premium is imposed for twice the number of years that you failed to register. Part B late enrollment has an even greater impact. The 10% increase for every 12-month period is the same, but the duration in most cases is for as long as you are enrolled in Part B.
What is Medicare's look back period?
How Medicare defines income. There is a two-year look-back period, meaning that the income range referenced is based on the IRS tax return filed two years ago. In other words, what you pay in 2020 is based on what your yearly income was in 2018. The income that Medicare uses to establish your premium is modified adjusted gross income (MAGI).
Medicaid Income Limits by State
See the Medicaid income limit for every state and learn more about qualifying for Medicaid health insurance where you live. While Medicaid is a federal program, eligibility requirements can be different in each state.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
What are the expenses that go away when you receive Medicaid at home?
When persons receive Medicaid services at home or “in the community” meaning not in a nursing home through a Medicaid waiver, they still have expenses that must be paid. Rent, mortgages, food and utilities are all expenses that go away when one is in a nursing home but persist when one receives Medicaid at home.
Is income the only eligibility factor for Medicaid?
Medicaid Eligibility Income Chart by State – Updated Mar. 2021. The table below shows Medicaid’s monthly income limits by state for seniors. However, income is not the only eligibility factor for Medicaid long term care, there are asset limits and level of care requirements.