What makes a good Medicaid managed care plan?
Oct 06, 2021 · Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
What are 3 different types of managed care plans?
Jul 02, 2021 · Medicare Managed Care plans are also known as Medicare Advantage plans, available through the Medicare Part C program. These plans are another way to get your Medicare Part A and Part B coverage (except for hospice care, which Part A covers). Some plans offer additional benefits, like routine vision care and prescription drug coverage. Types of …
What is the purpose of a managed care plan?
Mar 09, 2022 · The update to the CY 2021 guidance is now available below with the file names: CY2021 MA Enrollment and Disenrollment Guidance and CY2021 Cost Plan Enrollment and Disenrollment Guidance. All enrollments with an effective date on or after January 1, 2021, must be processed in accordance with the revised guidance requirements, including the new ...
What is the best health plan for Medicare?
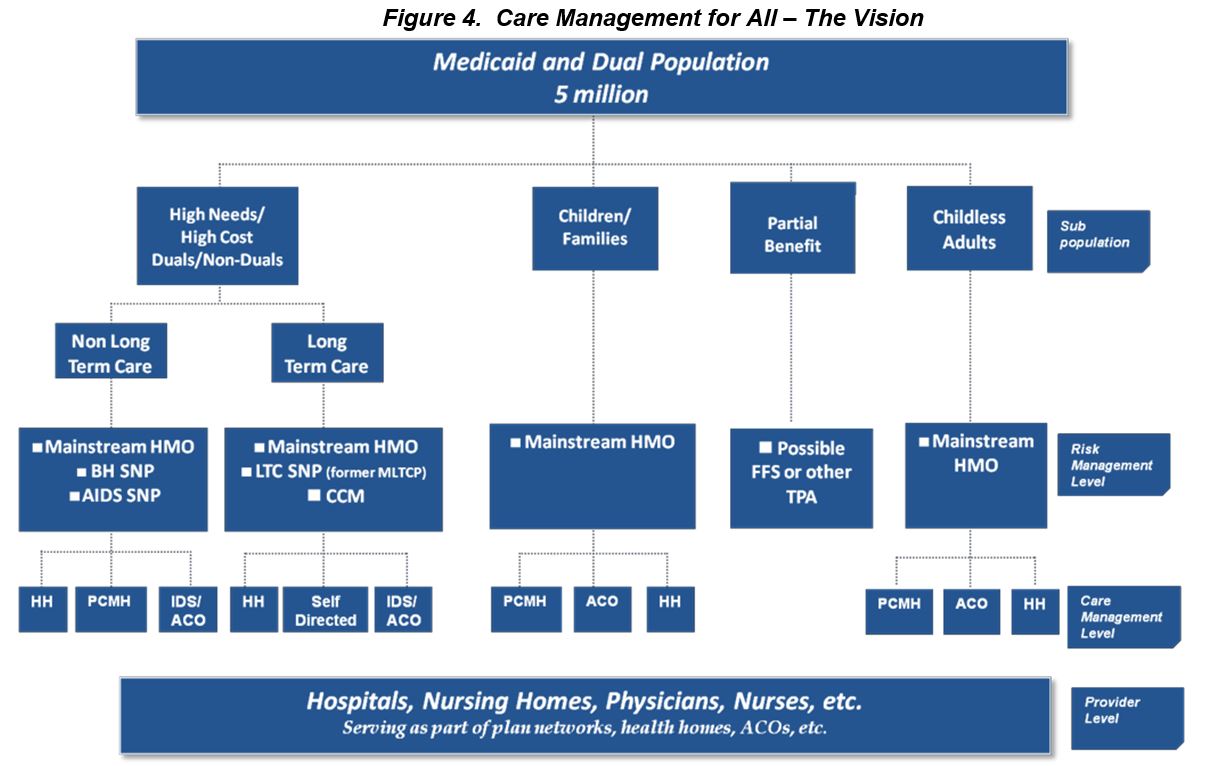
Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs) that accept a set per member per month (capitation) payment for these services. By contracting with various types of MCOs to deliver Medicaid program health care …

What is the difference between Medicare and managed Medicare?
Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare.Sep 9, 2020
What does managed care plan mean?
Managed care plans are a type of health insurance. They have contracts with health care providers and medical facilities to provide care for members at reduced costs. These providers make up the plan's network.Sep 20, 2018
What are advantages and disadvantages to having a Medicare managed plan?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
What is the difference between Medicare fee for service and Medicare managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
What is an example of a managed care plan?
A good example of a managed care plan is an HMO (Health Maintenance Organization). HMOs closely manage your care. Your cost is lowest with an HMO. You are limited to seeing providers in a small local network, which also helps keep costs low.
How does managed care work?
Under managed care, states sign contracts with "managed care organizations," or MCOs, that provide medical services through their own networks of doctors and hospitals. The state pays the MCO a fixed annual fee for each Medicaid patient. And the MCO takes responsibility for overseeing each person's care.May 31, 2011
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.Dec 21, 2021
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
Does Medicare covers dental work?
Medicare doesn't cover most dental care, dental procedures, or supplies, like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What is the most common form of managed care?
HMOThe most common type of managed care plan is the HMO. If you enroll in an HMO plan, you'll need to pick a primary care provider who will direct all your healthcare needs and refer you to specialists when appropriate. You are only covered if you go to medical providers and facilities who are in your network.
What are the three main payment mechanisms used in managed care?
What are the three main payment mechanisms managed care uses? In each mechanism who bears the risk. The three main types of payment arrangements with providers are: capitation, discounted fees, and salaries.
What is the biggest difference between Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.Oct 1, 2020
What is Medicare managed care?
Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare.
What is a Medigap plan?
A Medigap plan, also known as Medicare supplement insurance, is optional coverage you can add to original Medicare to help cover out-of-pocket costs. Medigap plans can help you pay for things like: coinsurance costs. copayments. deductibles. These aren’t a type of managed care plan.
How much does Medicare cost in 2021?
Most people receive Part A without paying a premium, but the standard Part B premium in 2021 is $148.50. The cost of your managed care plan will be on top of that $148.50.
What is Medicare Advantage?
Sometimes referred to as Medicare Part C or Medicare Advantage, Medicare managed care plans are offered by private companies. These companies have a contract with Medicare and need to follow set rules and regulations. For example, plans must cover all the same services as original Medicare.
Do you have to be enrolled in Medicare Part A and Part B?
You’ll need to be enrolled in both Medicare Part A and Part B to be eligible for a managed care plan. You can become eligible for parts A and B in a few ways:
What is PFFS in medical?
Private Fee-for-Service (PFFS). A PFFS is a less common type of managed care plan. PFFS plans don’t have networks. Instead, for a present price, you can see any doctor who contracts with Medicare. However, not all providers accept PFFS plans. Special Needs Plan (SNP).
What is the difference between HMO and POS?
The difference is that an HMO-POS plan allows you to get certain services from out-of-network providers — but you’ll likely pay a higher cost for these services than if you see an in-network provider. Private Fee-for-Service (PFFS). A PFFS is a less common type of managed care plan. PFFS plans don’t have networks.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is managed care plan?
Managed Care plans are different from Medicare Supplement (Medigap) plans. If you decide to stay with Original Medicare, another option you may have is to sign up for a Medicare Supplement (Medigap) plan to help pay for Original Medicare’s out-of-pocket costs.
What is an HMO plan?
HMO: A Health Maintenance Organization (HMO) plan has a network of doctors, hospitals, and providers that you must use to be covered by the plan. You’re typically not covered if you go out of network for care (except for emergency or urgent care).
What is Medicare Part A and Part B?
These plans are another way to get your Medicare Part A and Part B coverage (except for hospice care, which Part A covers). Some plans offer additional benefits, like routine vision care and prescription drug coverage.
Does Medigap pay for coinsurance?
Different Medigap plans pay for different amounts of those costs, such as copayments, coinsurance, and deductibles. *Out-of-network/non-contracted providers are under no obligation to treat Preferred Provider Organization (PPO) plan members, except in emergency situations.
What is Medicare Part B?
Medicare Part B covers individual and group therapy services to diagnose and treat mental illness. The Part B coverage usually requires a physician referral for mental health care and is based on a mental health diagnosis.
Who must provide acupuncture in MA?
The acupuncture provided by MA plans as a supplemental benefit must be provided by practitioners who are licensed or certified, as applicable, in the state in which they practice and are furnishing services within the scope of practice defined by their licensing or certifying state.
What is general nutrition education?
General nutritional education for all enrollees through classes and/or individual counseling may be provided as a supplemental benefit as long as the services are provided by practitioners who are practicing in the state in which s/he is licensed or certified, and are furnishing services within the scope of practice defined by their licensing or certifying state. (i.e., physician, nurse, registered dietician or nutritionist). The number of visits, time limitations, and whether the benefit is for classes and/or individual counseling must be defined in the PBP.
Does MA offer alternative therapies?
MA plans may offer alternative therapies as supplemental benefits. These alternative therapies must be provided by practitioners who are licensed or certified, as applicable, in the state in which they practice and are furnishing services within the scope of practice defined by their licensing or certifying state. MA plans are to provide a description of therapies offered in the PBP Notes section.
What is a non-SNP physical exam?
Non-SNP MA plans may offer as a supplemental benefit a physical exam that provides services beyond those services required to be provided in the Annual Wellness Visit. To be considered an Annual Physical Exam that qualifies as a supplemental benefit by CMS, the exam would be provided by a qualified physician or qualified non-physician practitioner, hereafter referred to as a practitioner. At a minimum, the exam would include a detailed medical/family history and the performance of a detailed head to toe assessment with hands-on examination of all the body systems. For example, the practitioner uses visual inspection, palpation, auscultation and 133 manual examination in his/her full examination to assess overall general health and detect abnormalities or signs that could indicate a disease process that should be addressed. We consider these components minimum elements and not an exhaustive list.
Does MA offer chiropractic care?
MA plans may choose to offer routine chiropractic services as a supplemental benefit as long as the services are provided by a state-licensed chiropractor practicing in the state in which he/she is licensed and is furnishing services within the scope of practice defined by that state’s licensure and practice guidelines. The routine services may include conservative management of neuromusculoskeletal disorders and related functional clinical conditions including, but not limited to, back pain, neck pain and headaches, and the provision of spinal and other therapeutic manipulation/adjustments.
What is post discharge reconciliation?
An MA plan may offer a post-discharge medication reconciliation as a supplemental benefit. For example, immediately following discharge (e.g., within the first week) from a hospital or SNF inpatient stay, MA plans may offer, as a supplemental benefit , the services of a qualified health care provider who, in cooperation with the enrollee’s physician, would review the enrollee’s complete medication regimen that was in place prior to admission and compare and reconcile with the regimen prescribed for the enrollee at discharge to ensure new prescriptions are obtained and discontinued medications are discarded. This reconciliation of the enrollee’s medications may be provided in the home and is designed to identify and eliminate medication side effects and interactions that could result in illness or injury.
How does managed care work?
The primary way in which managed care plans work is by establishing provider networks. A provider network serves plan members over a certain geographic area in which the health plan is available. The providers in these networks agree to offer their services at reduced costs. Your health plan pays more of the cost of your care if you see providers ...
What is managed care organization?
A managed care organization or MCO is a health care company or a health plan that is focused on managed care as a model to limit costs, while keeping quality of care high.
Why do doctors do regular check ups?
Regular check-ups help doctors identify health problems early, before they become major and costly. No-cost preventive care is a big incentive for plan members to try and maintain good health. Primary Care Providers (PCP): Your health plan may require you to choose a PCP if you don’t already have one.
What are some examples of managed care?
They are examples of managed care: Provider networks: Health insurance companies contract with groups of providers to offer plan members reduced rates on care and services. These networks can include doctors, specialists, hospitals, labs, and other health care facilities. Some health plans require you to use the plan’s provider network ...
Is a PPO more expensive than an HMO?
A PPO also costs a bit more than an HMO for that flexibility. Both types of plans are designed to help keep costs lower and quality high. Managed care is a type of health care model that is commonplace. Most common types of health plans have features of managed care that help keep costs in check and quality of care high.
What is a prior authorization?
Prior authorization: Most managed care plans require you to get approval before you have certain types of procedures or treatments done, or are prescribed certain types of specialty medications. This is called prior authorization, precertification, or preapproval, depending on your insurer. Part of managed care’s goal is to help ensure you are not ...
What is HMO insurance?
Health Maintenance Organization (HMO) manages care by requiring you to see network providers, usually for a much lower monthly premium. HMOs also often require you to see a PCP before going elsewhere, and do not cover you to see providers outside the network. Preventive care is covered at 100%.