What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.
Full Answer
Who pays primary Medicare?
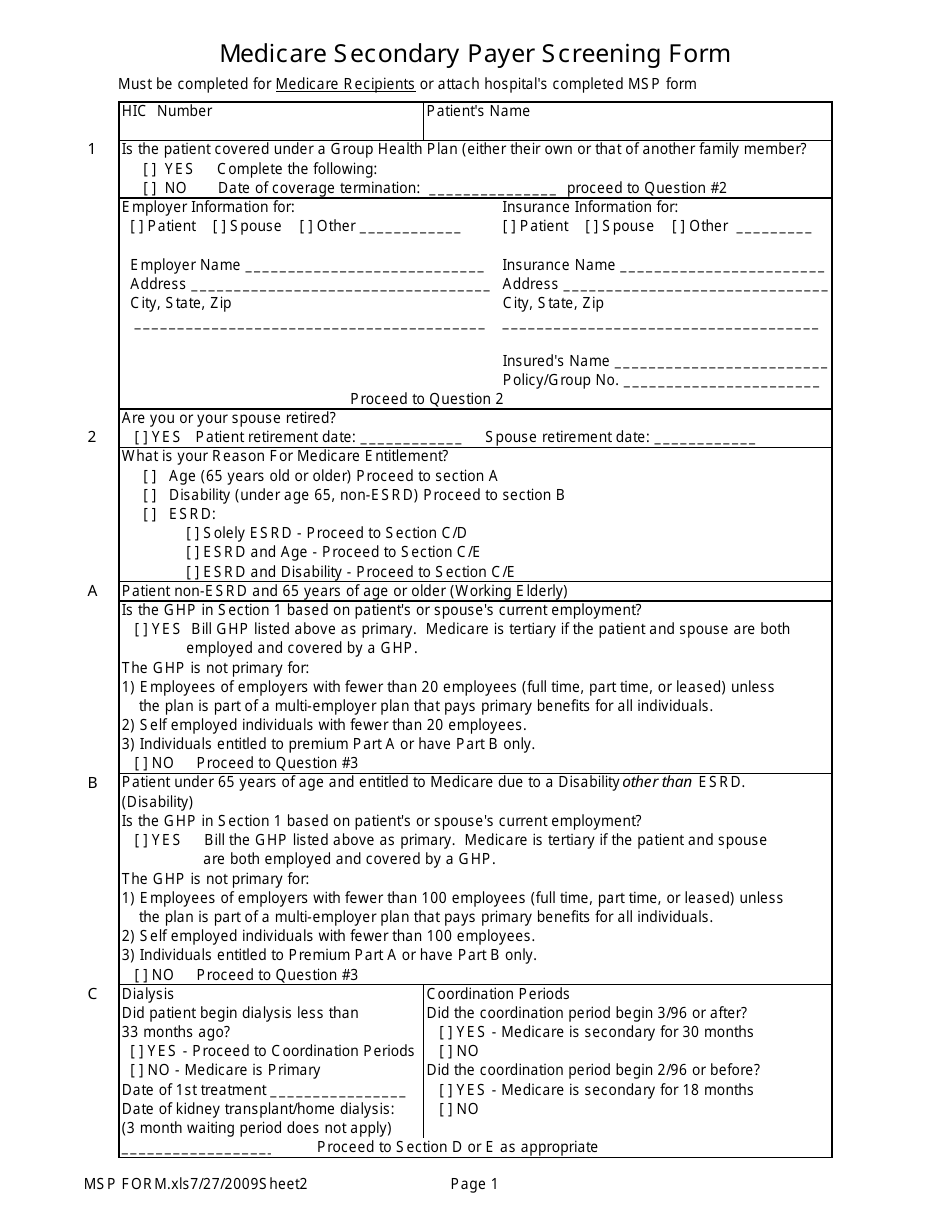
The “primary payer” pays what it owes on your bills first, then you or your health care provider sends the rest to the “secondary payer” (supplemental payer) to pay . In some rare cases, there may also be a “third payer .” Whether Medicare pays first depends on a number of things, including the situations listed on the next 4 pages .
What does insurances pay primary to Medicare?
Sep 13, 2021 · When you’re dual eligible for both Medicare and Medicaid, Medicare is your primary payer. Medicaid will not pay until Medicare pays first. Medicaid will not pay until Medicare pays first. If you’re dual-eligible and need assistance covering the costs of Part B and Part D, you could qualify for a Medicare Savings Program to assist you with these costs.
How to bill Medicare as secondary payer?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs.
Does Medi-Cal ever pay secondary if Medicare is primary?
Medicare is the primary payer for Medicare beneficiaries who are on employer plans if there are less than 20 employees. However, if the beneficiary is on an employer plan with 20 or more employees, that plan will serve as the primary payer,
Who is the primary payer of Medicare?
employerMedicare pays first . Medicare may pay second if both of these apply: Your employer (with fewer than 20 employees) joins other employers or employee organizations (like unions) to sponsor a multi-employer group health plan . At least one of the other employers has 20 or more employees .
Is Medicare always the primary payer?
), Medicare pays first. If you have Medicare due to ESRD, COBRA pays first and Medicare pays second during a coordination period that lasts up to 30 months after you're first eligible for Medicare. After the coordination period ends, Medicare pays first.
Who are the primary payers?
The insurance that pays first is called the primary payer. The insurance that picks up the remaining cost is the secondary payer. For example, if you had a X-ray bill of $100, the bill would first be sent to your primary payer, who would pay the amount agreed upon by your plan.
How do you know if Medicare is primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Does Medicare become primary at 65?
Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it's important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65.Mar 1, 2020
How do you determine which insurance is primary?
Primary insurance is a health insurance plan that covers a person as an employee, subscriber, or member. Primary insurance is billed first when you receive health care. For example, health insurance you receive through your employer is typically your primary insurance.Oct 8, 2019
Is Medicare Part B primary or secondary?
Your group insurance plan is the secondary insurer, so you should enroll in Medicare Part B before your group plan will pay its portion of the claim.
Does Medicare cover copay as secondary?
Usually, secondary insurance pays some or all of the costs left after the primary insurer has paid (e.g., deductibles, copayments, coinsurances). For example, if Original Medicare is your primary insurance, your secondary insurance may pay for some or all of the 20% coinsurance for Part B-covered services.
What does Medicare pay as secondary payer?
Medicare's secondary payment is $230, and the combined payment made by the primary payer and Medicare on behalf of the beneficiary is $680. The hospital may bill the beneficiary $70 (the $520 deductible minus the $450 primary payment).
What organization is responsible for overseeing Medicare?
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children's Health Insurance Program (CHIP).
Can you have Medicare and Humana at the same time?
Depending on where you live, you may be able to find a Medicare plan from Humana that suits your needs. Unlike Original Medicare (Part A and Part B), which is a federal fee-for-service health insurance program, Humana is a private insurance company that contracts with Medicare to offer benefits to plan members.
When a person has both Medicare and Medicaid insurance charges are submitted first to?
Medicaid is the payer of last resort, meaning it always pays last. When you visit a provider or facility that takes both forms of insurance, Medicare will pay first and Medicaid may cover your Medicare cost-sharing, including coinsurances and copays.
What is a small employer?
Those with small employer health insurance will have Medicare as the primary insurer. A small employer means less than 20 employees in the company. When you have small employer coverage, Medicare will pay first, and the plan pays second. If your employer is small, you must have both Part A and Part B. Having small employer insurance without ...
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
Key Takeaways
Medicare is the primary payer for beneficiaries who do not have other coverage through plans offered by employers, other groups, or unions, except under certain circumstances.
Can I have Medicare and Employer Health Insurance Together?
Yes, you can have both Medicare and employer health insurance together. When you have Medicare and other health insurance or coverage, you have more than one “payer.” In these instances, “coordination of benefits” rules will decide which payer pays first.
Does Medicare Cover Deductibles and Copays as Secondary Insurance?
The downside of having two insurance plans (group and Medicare) is that you pay two sets of premiums and deductibles. Your secondary insurance will not pay toward your primary health insurance deductible, and it’s likely you will still have to pay out-of-pocket costs.
Can I still use my Part A coverage even when I don't have Part B?
Yes, you can use Medicare Part A coverage even if you delay enrollment in Part B. However, unless you have other creditable coverage (like employer coverage) you should enroll in Part B, to avoid penalties in the future.
FAQs
Coordination of benefits (COB) is relevant for individuals with more than one primary payer. It is used to determine which insurance plan has the primary payment responsibility and the extent to which each plan covers an individual.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
Is Medicare the primary payer for workers compensation?
If you are covered under workers’ compensation due to a job-related injury or illness and are entitled to Medicare benefits, the workers’ compensation insurance provider will be the primary payer. There typically is no secondary payer in such cases, but Medicare may make a payment in certain situations.
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
What is the difference between Medicare and Medicaid?
Eligible for Medicare. Medicare. Medicaid ( payer of last resort) 1 Liability insurance only pays on liability-related medical claims. 2 VA benefits and Medicare do not work together. Medicare does not pay for any care provided at a VA facility, and VA benefits typically do not work outside VA facilities.
Is Medicare a secondary insurance?
When you have Medicare and another type of insurance, Medicare is either your primary or secondary insurer. Use the table below to learn how Medicare coordinates with other insurances. Go Back. Type of Insurance. Conditions.