
Medicare calculates the penalty by multiplying 1% of the "national base beneficiary premium" ($32.74 in 2020) times the number of full, uncovered months you didn't have Part D or creditable coverage. The monthly premium is rounded to the nearest $.10 and added to your monthly Part D premium.
Full Answer
What is the Part B premium penalty for Medicare Part B?
Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B. (Even though you weren't covered a total of 27 months, this included only 2 full 12-month periods.)
Does my income level affect my Medicare Part A premiums?
Your income level has no bearing on the amount you will pay for Medicare Part A (hospital insurance). Part A premiums (if you are required to pay them) are based on how long you worked and paid Medicare taxes. Most Part A beneficiaries qualify for premium-free Part A coverage.
How much is the monthly premium for Medicare Part A?
Monthly Premium. : Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $422 each month in 2018 ($437 in 2019). If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $422 ($437 in 2019).
What happens if I don't have Medicare Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B. And, the penalty increases the longer you go without Part B coverage.
What is the income penalty for Medicare?
If your MAGI for 2020 was less than or equal to the “higher-income” threshold — $91,000 for an individual taxpayer, $182,000 for a married couple filing jointly — you pay the “standard” Medicare Part B rate for 2022, which is $170.10 a month.
How is Medicare penalty calculated?
Medicare calculates the penalty by multiplying 1% of the "national base beneficiary premium" ($33.37 in 2022) times the number of full, uncovered months you didn't have Part D or creditable coverage. The monthly premium is rounded to the nearest $. 10 and added to your monthly Part D premium.
How do I avoid Medicare Part B penalty?
You can sign up later without penalty, as long as you do it within eight months after your other coverage ends. If you don't qualify to delay Part B, you'll need to enroll during your Initial Enrollment Period to avoid paying the penalty.
How is Medicare Part B penalty calculated?
Calculating Lifetime Penalty Fees Calculating your Part B penalty is fairly straightforward. You simply add 10% to the cost of your monthly premium for each year-long period you didn't have Medicare. It's simple to get a snapshot of what you will have to pay each month.
Can Medicare penalties be waived?
You may qualify to have your penalty waived if you were advised by an employee or agent of the federal government – for example by Social Security or 1-800-MEDICARE – to delay Part B. Asking for the correction is known as requesting equitable relief.
How are part a penalties calculated?
How is the Part A late enrollment penalty calculated? If you do have to pay premiums for Part A, the late enrollment penalty is 10 percent of either $274 or $499, added to that monthly premium.
Why is there a Medicare penalty?
Medicare charges several late-enrollment penalties. They're meant to discourage you from passing up coverage, then getting hit with costly medical bills. To avoid higher Medicare premiums, you need to know about these penalties and take steps to avoid them.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
At what income level do Medicare premiums increase?
For example, when you apply for Medicare coverage for 2022, the IRS will provide Medicare with your income from your 2020 tax return. You may pay more depending on your income. In 2022, higher premium amounts start when individuals make more than $91,000 per year, and it goes up from there.
Does Medicare Part B premium change every year based on income?
Remember, Part B Costs Can Change Every Year The Part B premium is calculated every year. You may see a change in the amount of your Social Security checks or in the premium bills you receive from Medicare. Check the amount you're being charged and follow up with Medicare or the IRS if you have questions.
What happens if my Medicare Part B lapses?
If you've disenrolled from or cancelled your Medicare Part B coverage, you may have to pay a costly late enrollment penalty to reenroll. This is especially true if you have a gap in coverage.
Is there a cap on Medicare Part D Penalty?
The Part D penalty has no cap. For example: The national average premium is $33.37 a month in 2022. If you went 29 months without creditable coverage, your penalty would be $9.70.
What is a hold harmless on Medicare?
If you pay a higher premium, you are not covered by “hold harmless,” the rule that prevents most Social Security recipients from seeing their benefit payment go down if Medicare rates go up. “Hold harmless” only applies to people who pay the standard Part B premium and have it deducted from their Social Security benefit.
What is the Medicare Part B rate for 2021?
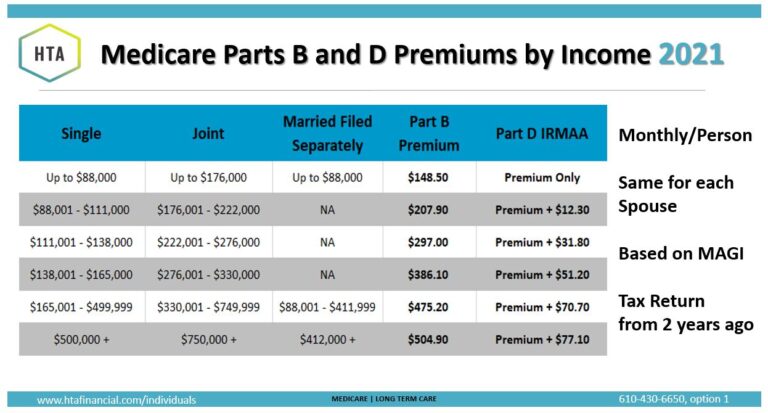
If your MAGI for 2019 was less than or equal to the “higher-income” threshold — $88,000 for an individual taxpayer, $176,000 for a married couple filing jointly — you pay the “standard” Medicare Part B rate for 2021, which is $148.50 a month.
What is Medicare premium based on?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That’s your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS. To set your Medicare cost for 2021, Social Security likely relied on the tax return you filed in 2020 that details your 2019 ...
Does Medicare Part D increase with income?
Premiums for Medicare Part D (prescription-drug coverage), if you have it , also rise with higher incomes .
Can you ask Social Security to adjust your premium?
You can ask Social Security to adjust your premium if a “life-changing event” caused significant income reduction or financial disruption in the intervening tax year — for example, if your marital status changed , or you lost a job , pension or income-producing property. You’ll find detailed information on the Social Security web page “Medicare ...
Do you pay Medicare Part B if you are a high income beneficiary?
If you are what Social Security considers a “higher-income beneficiary,” you pay more for Medicare Part B, the health-insurance portion of Medicare. (Most enrollees don’t pay for Medicare Part A, which covers hospitalization.) Medicare premiums are based on your modified adjusted gross income, or MAGI. That’s your total adjusted gross income ...
How much is the 2021 Medicare Part B deductible?
The 2021 Part B deductible is $203 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
When will Medicare Part B and Part D be based on income?
If you have Part B and/or Part D benefits (which are optional), your premiums will be based in part on your reported income level from two years prior. This means that your Medicare Part B and Part D premiums in 2021 may be based on your reported income in 2019.
What is Medicare Part B based on?
Medicare Part B (medical insurance) premiums are based on your reported income from two years prior. The higher premiums based on income level are known as the Medicare Income-Related Monthly Adjustment Amount (IRMAA).
Does Medicare have a 0 premium?
Some Medicare Advantage plans even feature $0 monthly premiums, though $0 premium plans may not be available in all locations. Find out if a $0 premium plan is available where you live by calling to speak with a licensed insurance agent.
Does Medicare Advantage cover Part A?
Did you know that a Medicare Advantage plan covers the same benefits that are covered by Medicare Part A and Part B (Original Medicare)? Did you know that some Medicare Advantage plans also offer benefits not covered by Original Medicare?
Who sells Medicare Part C?
Medicare Part C plans (also called Medicare Advantage) and Medicare Supplement Insurance plans (also called Medigap) are sold by private insurance companies. The cost of plans can vary from one provider to the next.
Does income affect Medicare Part A?
Medicare Part A costs are not affected by your income level. Your income level has no bearing on the amount you will pay for Medicare Part A (hospital insurance). Part A premiums (if you are required to pay them) are based on how long you worked and paid Medicare taxes.
How much does Medicare premium go up if you have Part B?
If you get hit with the late enrollment penalty, your premium may go up 10 percent for each full year that you could have had Part B, but didn’t. That means you can get hit more than once! Visit medicare.gov to see what your Part B premium is.
What is the Part D penalty?
Part D penalty. The government requires everyone on Medicare to have creditable prescription drug coverage (Part D coverage that’s at least as good as Medicare’s standard). Let’s say you’re about to turn 65 and become eligible for Medicare.
How long can you go without prescription coverage?
If you go without creditable prescription drug coverage for 63 days in a row (or more) after you sign up for Medicare, you may have to pay a late enrollment penalty. This penalty is added to your monthly Part D premium and you’ll have to pay it for as long as you have a Medicare drug plan.
How often do you have to pay Medicare Part B?
Whether you stick with Original Medicare only or choose to buy a private plan, you must continue to pay your Medicare Part B premium each month. Your premium is based on your income. The government sets these amounts each year, which means they may change from one year to the next. If you get hit with the late enrollment penalty, your premium may go up 10 percent for each full year that you could have had Part B, but didn’t. That means you can get hit more than once! Visit medicare.gov to see what your Part B premium is.
What is extra help for Medicare?
The Medicare Savings Programs and Extra Help program can provide financial help for various health care or prescription drug costs. Your income and assets determine if you’re eligible. Assets include cash, savings and investment and vacation property.
How long do late payment penalties last?
Unlike a one-time fee for a late payment on your credit card, these penalties last forever! Take the time to make sure you don’t get dinged. The graphic below sums up these penalties and offers tips for avoiding them.
Does Medicaid cover Minnesota?
Medicaid (called Medical Assistance in Minnesota) can help pay for Medicare premiums, deductibles, copays and/or coinsurance. Medicaid may cover services Original Medicare doesn’t. For example, Medicaid can cover care in a designated nursing facility if you don’t have money, assets or long-term care insurance to pay for it.
What happens if you don't get Social Security?
If the amount is greater than your monthly payment from Social Security, or you don’t get monthly payments, you’ll get a separate bill from another federal agency , such as the Centers for Medicare & Medicaid Services or the Railroad Retirement Board.
What happens if you file taxes as married filing jointly?
If you file your taxes as “married, filing jointly” and your MAGI is greater than $176,000, you’ll pay higher premiums for your Part B and Medicare prescription drug coverage. If you file your taxes using a different status, and your MAGI is greater than $88,000, you’ll pay higher premiums (see the chart below, Modified Adjusted Gross Income (MAGI), for an idea of what you can expect to pay).
What is the number to call for Medicare prescriptions?
If we determine you must pay a higher amount for Medicare prescription drug coverage, and you don’t have this coverage, you must call the Centers for Medicare & Medicaid Services (CMS) at 1-800-MEDICARE ( 1-800-633-4227; TTY 1-877-486-2048) to make a correction.
What happens if your MAGI is greater than $88,000?
If you file your taxes using a different status, and your MAGI is greater than $88,000, you’ll pay higher premiums (see the chart below, Modified Adjusted Gross Income (MAGI), for an idea of what you can expect to pay).
How to determine 2021 Social Security monthly adjustment?
To determine your 2021 income-related monthly adjustment amounts, we use your most recent federal tax return the IRS provides to us. Generally, this information is from a tax return filed in 2020 for tax year 2019. Sometimes, the IRS only provides information from a return filed in 2019 for tax year 2018. If we use the 2018 tax year data, and you filed a return for tax year 2019 or did not need to file a tax return for tax year 2019, call us or visit any local Social Security office. We’ll update our records.
How to determine 2021 income adjustment?
To determine your 2021 income-related monthly adjustment amounts, we use your most recent federal tax return the IRS provides to us. Generally, this information is from a tax return filed in 2020 for tax year 2019. Sometimes, the IRS only provides information from a return filed in 2019 for tax year 2018. If we use the 2018 tax year data, and you filed a return for tax year 2019 or did not need to file a tax return for tax year 2019, call us or visit any local Social Security office. We’ll update our records.
What happens if you amend your tax return?
If you amended your tax return, and it changes the income we count to determine the income-related monthly adjustment amounts (your MAGI), let us know. Social Security needs to see a copy of the amended tax return you filed and your acknowledgment receipt from IRS. We’ll update our records with the information you provide, and correct or remove your income-related monthly adjustment amounts, as appropriate.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
How long do you have to pay late enrollment penalty?
In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage. Learn more about the Part D late enrollment penalty.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How many income brackets does Social Security have?
The Social Security Administration (SSA) sets four income brackets that determine your (or you and your spouse’s) IRMAA. SSA determines if you owe an IRMAA based on the income you reported on your IRS tax return two years prior, meaning two years before the year that you start paying IRMAA.
How does the SSA determine if you owe an IRMAA?
SSA determines if you owe an IRMAA based on the income you reported on your IRS tax return two years prior, meaning two years before the year that you start paying IRMAA. The income that counts is the adjusted gross income you reported plus other forms of tax-exempt income.
What happens if you pay IRMAA?
If you are expected to pay IRMAA, SSA will notify you that you have a higher Part B premium.
