CMS created the Preclusion List with three main goals:
- To ensure that problematic prescribers do not receive payment for prescribing Part D drugs
- To reduce burdens on Part D and Medicare Advantage providers while maintaining program integrity
- To replace Medicare Advantage’s enrollment requirements
What is the preclusion list for Medicare Advantage?
Preclusion List What is the Preclusion List? A list of providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. Why was the list created? To replace the Medicare Advantage (MA) and prescriber enrollment requirements.
What is the preclusion list and why is it important?
CMS Preclusion List . Quick Reference Guide NOTE: Part D sponsors and MA plans should not begin requesting access to the Preclusion List until September 1, 2018. ... EIDM is the system that connects you to all the Centers for Medicare & Medicaid Services (CMS) applications with one central user ID. The EIDM user authentication process prevents
When will the CMS preclusion list be published?
Nov 09, 2021 · The Preclusion List names providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. The Preclusion List applies only to Medicare Advantage items and services or Part D drugs for Medicare beneficiaries.
What is the preclusion list for Part D?
Preclusion List Frequently Asked Questions (FAQs) General . 1. What is the Preclusion List? The Preclusion List is comprised of any individual or entity that meets the following criteria: • Is currently revoked from Medicare, are under an active reenrollment bar, and CMS has determined that the underlying conduct that led to the revocation is
What is the difference between preclusion and exclusion?
The Preclusion List and exclusion file overlap in the sense that excluded providers will be on the preclusion list, but precluded providers who are not excluded will not be on the exclusion file. Therefore, if a plan finds a provider on the OIG exclusion file, the plan is not required to check the Preclusion List.Jan 27, 2020
Where can I find the CMS preclusion list?
You will need an EIDM user ID to access the Preclusion List. Go to the CMS Enterprise Portal at https://portal.cms.gov and choose “New User Registration.” > Use the drop-down menu to choose “Preclusion List” as your application.
Who can access the preclusion list?
CMS approved healthcare plansPreclusion List File 23. Who is able to access the Preclusion List? Only CMS approved healthcare plans, with a valid Health Plan ID, can gain access to the Preclusion List.Dec 16, 2020
What is a CMS exclusion list?
The CMS Preclusion List is a registry of all health care providers, suppliers, and prescribers who are precluded from receiving reimbursement for Part C Medicare Advantage items and services or Part D drugs that are provided or prescribed to Medicare beneficiaries.May 26, 2021
Is the CMS preclusion list public?
Because the CMS Preclusion List is not publicly available, it can be difficult for organizations to screen against it. Although individuals and entities on the list receive a notification, healthcare organizations and entities also need this information to avoid hiring precluded providers.Nov 9, 2021
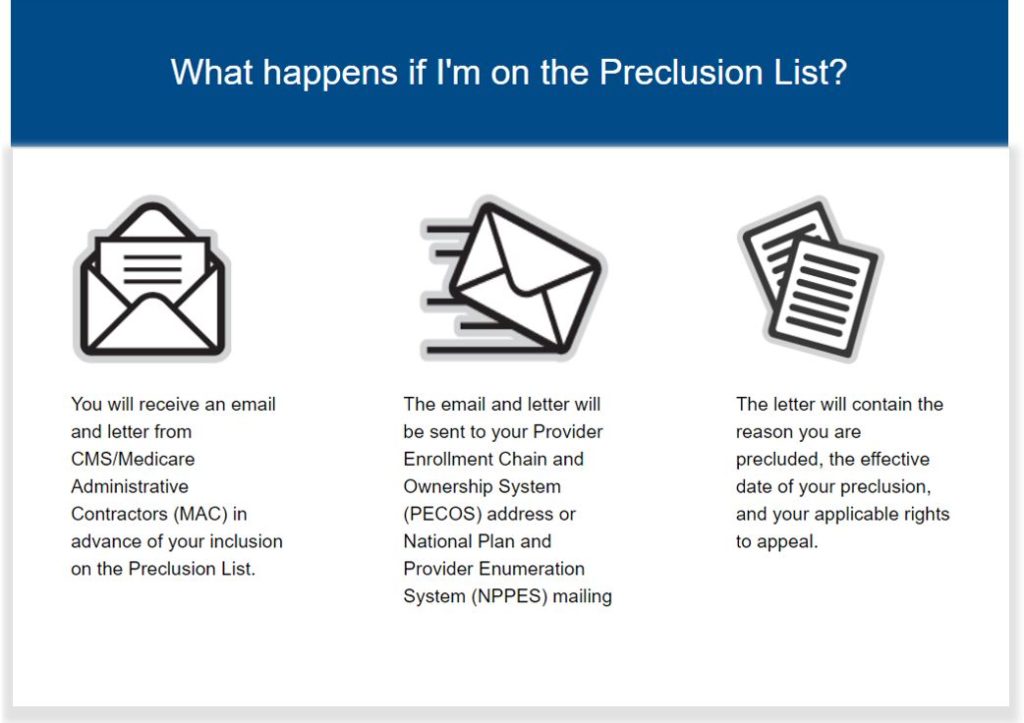
What is a preclusion letter?
The Preclusion List is a list generated by CMS that contains the names of prescribers, individuals, and or entities that are unable to receive payment for Medicare Advantage (MA) items and service and or Part D drugs prescribed or provided to Medicare beneficiaries.Feb 13, 2019
What is a Medicare revocation?
Medicare billing privileges can be revoked for twenty-two enumerated reasons, including non-compliance with Medicare enrollment requirements, felony convictions, and failure to respond to requests for medical records.Mar 1, 2021
What is a MA organization?
MA organization means a public or private entity organized and licensed by a State as a risk-bearing entity (with the exception of provider-sponsored organizations receiving waivers) that is certified by CMS as meeting the MA contract requirements.
What does Exclusion List mean?
Exclusion List 101 an overview. In a nutshell, the OIG's LEIE (Exclusion List) is where individuals and entities currently excluded from participation in Medicare, Medicaid and all other Federal health care programs, can be found.
What is an exclusion list?
What are Exclusion Lists? In simplest terms, a government exclusion list is a roster of individuals and organizations that are not eligible to participate in federal or state contracts due to criminal behavior or misconduct. These lists are maintained by state or federal agencies and updated regularly.Jan 11, 2021
Why would someone be on the Sam exclusion list?
Basically, if you owe the government money or have violated certain federal laws, this easily could result in exclusion, but anytime a government agency suspects that an entity or people within that entity have acted in an unethical manner, they might decide to push for your exclusion from receiving future government ...Jan 30, 2019
What is a preclusion list?
According to the Centers for Medicare and Medicaid (CMS), the Preclusion List is a list of providers and prescribers who are precluded from receiving payment for Medicare Advantage (MA) items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. The Preclusion List applies only to Medicare Advantage items ...
When did the CMS preclusion list go into effect?
When Did the New Preclusion List Go into Effect? The CMS Preclusion List was announced in April 2018, but the first provider list was published and notices were sent in January 2019. MA plans had until January 31, 2019 to remove providers from their plans.
Can you receive Medicare if you are on the preclusion list?
Individuals and entities who are listed on the Medicare Preclusion List cannot receive money from Medicare, so organizations need to screen their providers against this list regularly to make sure they are not billing charges from providers that are not eligible.
When will the CMS release the preclusion list?
In an effort to provide MA and Part D plans more time to process new providers and reinstatements received on the Preclusion List, CMS will publish the Preclusion List by the 25th of each month or the last Monday of the month, whichever is earlier, for the following month. These changes will be implemented with the Preclusion List published in September 2019 (i.e., CMS will publish the September Preclusion List on August 26th as August 25th falls on a weekend).
How long does a Medicare reenrollment bar last?
The re-enrollment bar becomes effective 30 days from the date of issuance of the initial determination letter and lasts a minimum of 1 year, but not greater than 10 years, depending on the severity of the basis for revocation. In addition, CMS may impose a re-enrollment bar of up to 20 years if the provider or supplier is being revoked from Medicare for the second time.
Does CMS base preclusion date on OIG?
CMS will not base the preclusion date on the OIG exclusion date. The preclusion date is based on the publication date. The Preclusion List and exclusion file overlap in the sense that excluded providers will be on the Preclusion List if they meet the following criteria:
Do Medicare plans have to update the preclusion list?
Yes. As stated in the November 2, 2018 HPMS guidance memo, “CMS recommends that Medicare plans and Part D plans follow the same process for monthly updates to the Preclusion List as they did for the initial list. The plans will have 30 days to review the Preclusion List for updates and should notify the impacted enrollees as soon as possible, but no later than 30 days from the posting of the updated list.” However, since the subsequent Preclusion Lists will be full files, Medicare plans and Part D plans are not required to resend monthly notices to the same beneficiaries when the same precluded provider appears on the monthly list. CMS will provide the claim rejection and payment denial date for all newly added providers each month.
Does CMS require a sponsor to notify a prescriber of a beneficiary?
No. The regulation states that a sponsor must ensure reasonable efforts are made to notify the prescriber of a beneficiary who was sent a notice. CMS does not view reasonable efforts as including notifying these types of providers.
Is the MA preclusion list required for non-contracting providers?
Yes, effective January 1, 2020, the regulation will formally require application of the preclusion list to non-contracted MA providers. However, CMS stated in the preamble to CMS-4182-F that plans should begin applying these requirements, including beneficiary notification, to non-contracted providers as a best practice.
Is a provider on the preclusion list a coverage request?
The issue of the provider being on the preclusion list is not a coverage request. Therefore, clinical appropriateness should not be reviewed, and, there would not be a reason for an authorization to be put in place for a Part D drug.
What is a Medicare MCMG?
The Medicare Communications and Marketing Guidelines (MCMG) discuss requirements applicable to all communication activities and materials, as well as additional requirements only applicable to marketing activities and materials. The beneficiary letter is designated as a communication material and as such, this means that all activities and materials are aimed at prospective and current enrollees, and are within the scope of the regulations at 42 C.F.R. Parts 417, 422, and 423.
Is a beneficiary notice required for a 2018 HPMS guidance memo?
Yes. The beneficiary notice attached to the November 2, 2018 HPMS guidance memo is a sample notice. Plans are not required to use this version for the required beneficiary notice, however, the letters should include the information specified in the sample notice.
Do Medicare plans have to update the preclusion list?
Yes. As stated in the November 2, 2018 HPMS guidance memo, “CMS recommends that Medicare plans and Part D plans follow the same process for monthly updates to the Preclusion List as they did for the initial list. The plans will have 30 days to review the Preclusion List for updates and should notify the impacted enrollees as soon as possible, but no later than 30 days from the posting of the updated list.” However, since the subsequent Preclusion Lists will be full files, Medicare plans and Part D plans are not required to resend monthly notifies to the same beneficiaries when the same precluded provider appears on the monthly list.
Can a CMS plan access the preclusion list?
Only approved CMS healthcare plans, with a valid Health Plan ID, can gain access to the Preclusion List. For instructions on how to access the Preclusion List visit
Does CMS base preclusion date on OIG?
CMS will not base the preclusion date on the OIG exclusion date. The preclusion date is based onthe publication date. The Preclusion List and exclusion file overlap in the sense that excludedproviders will be on the Preclusion List if they meet the following criteria:
What is a preclusion list?
What is the Preclusion List? The Preclusion List is a list generated by CMS that contains the names of prescribers, individuals, and or entities that are unable to receive payment for Medicare Advantage (MA) items and service and or Part D drugs prescribed or provided to Medicare beneficiaries. II.
What is Engaged in Behavior for which CMS could have revoked the prescriber, individual or entity to
Engaged in behavior for which CMS could have revoked the prescriber, individual or entity to the extent applicable if they had been enrolled in Medicare, and CMS determines that the underlying conduct that would have led to the revocation is detrimental to the best interests of the Medicare program.
How much money will Medicare save in 2019?
And to. “To replace the Medicare Advantage (MA) and prescriber enrollment requirements.”. By doing this, CMS believes that it will save $34.4 million dollars in 2019.
When will Medicare Part D be denied?
The first list of providers that were to be precluded were published and were sent notice on January 1, 2019. However, beginning April 1, 2019 Part D sponsors will become required to reject any prescriptions for Medicare Part D drugs that are prescribed by an individual or entity that is on the Preclusion List. Medicare Advantage (MA) plans will also become required to deny payments for any healthcare service or item that was provided by and individual or entity that is on the Preclusion List.
Is the preclusion list restricted?
Unfortunately, access to the Preclusion List is Extremely Restricted. However, under certain circumstances, we here at Exclusion Screening, LLC can provide guidance and help. Contact us [email protected], give us a call at (800)-294-0952, or fill out the form below for a free consultation and quote.
Can you end up on the Medicare preclusion list?
The first one way is if you: “Are currently revoked from Medicare, are under an active reenrollment bar, and CMS has determined that the underlying conduct that led to the revocation is detrimental to the best interests of the Medicare program”.
When was the CMS preclusion list published?
Since the CMS Preclusion list was announced in April 2018, and then published in January 2019, there has been confusion and questions regarding the list, its differences from the OIG Exclusion List, the size of the list, and who has access.
What is OIG exclusion list?
1. Overview. The OIG Exclusion List is a registry of individuals and entities that have been excluded from participation in Federal health care programs. Exclusion may be mandatory in nature or permissive, depending based on the underlying adverse action.
What is the CMS preclusion list?
On January 1, 2019, the Centers for Medicare & Medicaid Services (CMS) introduced a new tool for Medicare plans – the CMS Preclusion List. A previous article posted in 2018 provides an excellent overview of the new policy and process. The Preclusion List, updated monthly, provides the name of providers and prescribers who are precluded ...
When was the preclusion list issued?
Per the Final Rule issued by CMS on April 16, 2019 , the Preclusion List offered the most effective means of reducing the burden of the MA and Part D provider/prescriber enrollment requirements without compromising Medicare’s financial integrity by shifting focus toward providers and prescribers that pose an elevated risk to Medicare beneficiaries.
Why is OIG not required to check the CMS preclusion list?
OIG exclusions are imposed due to criminal behavior and as such are part of the CMS Preclusion List criteria. Therefore, if a plan finds a provider in the OIG LEIE, the plan is not required to check the CMS Preclusion List. > However, there are other providers who are precluded by CMS from participation in a Medicare plan ...
Does Medicare Preclusion List eliminate the requirement that Medicare Advantage and Part D plans validate their providers monthly against the OIG'
> Use of the CMS Medicare Preclusion List does not eliminate the requirement that Medicare Advantage and Part D plans validate their providers monthly against the OIG’s Exclusion List, which is the List of Excluded and Ineligible Entities (“LEIE”). This list is updated monthly by the OIG to reflect exclusions from participation and payment under Medicare or Medicaid contracts due to criminal behavior.
Does Medicare preclude TIN?
It should be noted that CMS precludes individuals and entities at the Tax Identification Number (TIN) level. Therefore, individuals and entities will not appear on the preclusion list unless ALL Medicare enrollments under their TIN are revoked or inactive.
Does Medicare Part D have fraud protection?
These include: > Medicare Part D does not have three key tools to protect against pharmacy fraud that are available in other parts of Medicare: pharmacy enrollment, revocation, and preclusion.
Can pharmacies continue to bill Part D?
Without a requirement that prevents payment, precluded pharmacies can continue to bill and be paid by Part D even after these pharmacies are proven to be detrimental to the program. In her January 2020 response, Seema Verma, CMS Administrator, concurred with a commitment to explore the feasibility of each recommendation.