Medicare helps make health coverage more affordable. Medicare sets an amount to pay a doctor or hospital, called the Medicare-approved amount. When you see a doctor or stay in a hospital that accepts Medicare, they will charge for a service.
What are the advantages and disadvantages of Medicare?
What Are the Pros of a Medicare Advantage Plan?
- Additional Benefits. As mentioned above, Medicare Advantage plans can provide additional benefits that are not found in Original Medicare.
- Out-Of-Pocket Protection. ...
- Coordinated Care. ...
- Plan Selection. ...
- Customized Coverage. ...
How can you tell if someone has Medicare?
- individual was no longer serving as a volunteer outside of the United States;
- organization no longer has tax-exempt status; or
- individual no longer has health insurance that provides coverage outside of the United States.
How do you find out if you have Medicare?
- The Social Security Administration is a partner agency with the Centers for Medicare and Medicaid. ...
- Medicare is the agency that runs Medicare. ...
- The Centers for Medicare and Medicaid or CMS is the federal agency that has responsibility for the entire public healthcare system for Americans of all ages. ...
What are the basics of Medicare?
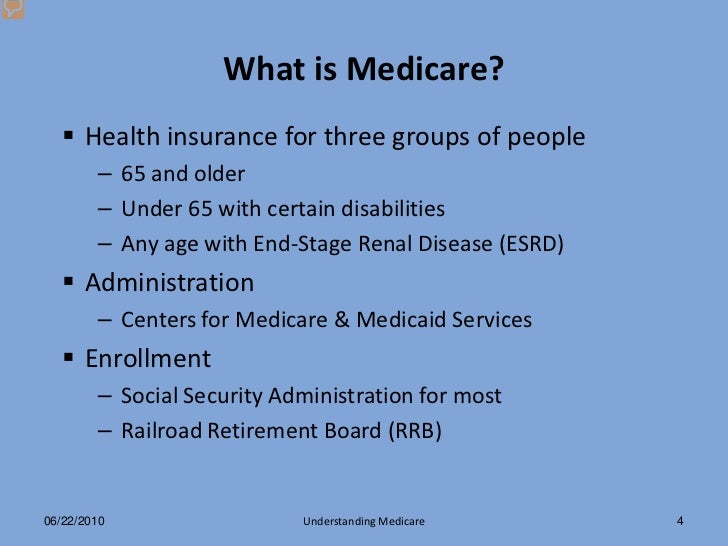
medicare is a government-sponsored health insurance program for american citizens and permanent legal residents (of at least five years in a row) who are 65 years old or more, or who qualify by disability or certain conditions, such as end-stage renal disease (permanent kidney failure requiring continuous dialysis treatment or a kidney …

What does Medicare focus on?
Medicare covers a variety of clinical preventive services, including influenza, pneumococcal, and hepatitis B vaccinations; mammography, colorectal, cervical, and prostate cancer screening; glaucoma screening; bone mass measurement; diabetes self-management training; diabetes supplies and services; and medical ...
What type of care does Medicare provide?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
How does Medicare work in simple terms?
Medicare is our country's health insurance program for people age 65 or older and younger people receiving Social Security disability benefits. The program helps with the cost of health care, but it doesn't cover all medical expenses or the cost of most long-term care.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Which type of care is not covered by Medicare?
does not cover: Routine dental exams, most dental care or dentures. Routine eye exams, eyeglasses or contacts. Hearing aids or related exams or services.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Why is Medicare important to the elderly?
Medicare coverage is especially important to low-income elderly people because they are in poorer health than higher income elderly people and have few financial assets to draw on when faced with high medical costs.
Does Medicare cover long-term care?
Medicare doesn't cover long-term care (also called custodial care) if that's the only care you need. Most nursing home care is custodial care, which is care that helps you with daily living activities (like bathing, dressing, and using the bathroom).
Medicare Eligibility, Applications, and Appeals
Find information about Medicare, how to apply, report fraud, and submit complaints.What help is available?Medicare is the federal health insurance...
Voluntary Termination of Medicare Part B
You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 to the Social Secur...
Medicare Prescription Drug Coverage (Part D)
Part D of Medicare is an insurance coverage plan for prescription medication. Learn about the costs for Medicare drug coverage.EligibilityPrescript...
Replace Your Medicare Card
You can replace your Medicare card in one of the following ways if it was lost, stolen, or destroyed:Log into your MyMedicare.gov account and reque...
Medicare Coverage Outside the United States
Medicare coverage outside the United States is limited. Learn about coverage if you live or are traveling outside the United States.Original Medica...
What is Medicare Advantage?
Medicare Advantage, also known as Medicare Part C, is a type of health plan offered by private insurance companies that provides the benefits of Parts A and Part B and often Part D (prescription drug coverage) as well. These bundled plans may have additional coverage, such as vision, hearing and dental care.
What is not covered by Medicare?
The biggest potential expense that’s not covered is long-term care, also known as custodial care. Medicaid, the federal health program for the poor, pays custodial costs but typically only for low-income people with little savings. Other common expenses that Medicare doesn’t cover include:
How long do you have to sign up for Medicare Part B?
You can avoid the penalty if you had health insurance through your job or your spouse’s job when you first became eligible. You must sign up within eight months of when that coverage ends.
What are the most common medical expenses that are not covered by Medicaid?
The biggest potential expense that’s not covered is long-term care, also known as custodial care . Medicaid, the federal health program for the poor, pays custodial costs but typically only for low-income people with little savings. Hearing aids and exams for fitting them. Eye exams and eyeglasses.
Does Medicare Part A cover hospice?
Part A also helps pay for hospice care and some home health care. Medicare Part A has a deductible ($1,484 in 2021) and coinsurance, which means patients pay a portion of the bill. There is no coinsurance for the first 60 days of inpatient hospital care, for example, but patients typically pay $371 per day for the 61st through 90th day ...
Is Medicare the same as Medicaid?
No. Medicare is an insurance program, primarily serving people over 65 no matter their income level. Medicare is a federal program, and it’s the same everywhere in the United States. Medicaid is an assistance program, serving low-income people of all ages, and patient financial responsibility is typically small or nonexistent.
Does Medicare cover eye exams?
Medicare also doesn’t cover eye exams for eyeglasses or contact lenses. Some Medicare Advantage Plans (Medicare Part C) offer additional benefits such as vision, dental and hearing coverage. To find plans with coverage in your area, visit Medicare’s Plan Finder.
Medicare Eligibility, Applications, and Appeals
Find information about Medicare, how to apply, report fraud and complaints.
Voluntary Termination of Medicare Part B
You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 ( PDF, Download Adobe Reader) to the Social Security Administration (SSA). Visit or call the SSA ( 1-800-772-1213) to get this form.
Medicare Prescription Drug Coverage (Part D)
Part D of Medicare is an insurance coverage plan for prescription medication. Learn about the costs for Medicare drug coverage.
Replace Your Medicare Card
You can replace your Medicare card in one of the following ways if it was lost, stolen, or destroyed:
Medicare Coverage Outside the United States
Medicare coverage outside the United States is limited. Learn about coverage if you live or are traveling outside the United States.
Do you have a question?
Ask a real person any government-related question for free. They'll get you the answer or let you know where to find it.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
What is covered by Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents.
Who pays payroll taxes?
Payroll taxes paid by most employees, employers, and people who are self-employed. Other sources, like these: Income taxes paid on Social Security benefits. Interest earned on the trust fund investments. Medicare Part A premiums from people who aren't eligible for premium-free Part A.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
How is Medicare funded?
Medicare is funded through the Hospital Insurance Trust Fund and the Supplementary Medical Insurance Trust Fund.
Get involved with Medicare
Get involved with Medicare to help us define, design, and deliver care. Join a Technical Expert Panel, comment on proposed rules, and follow Medicare news.
Contact Medicare
How to contact the Centers for Medicare & Medicaid Services (CMS) by phone, TTY, or mail.
Plain writing
Information about CMS's efforts to write content so you can understand.
Information in other languages
Languages include: American Sign Language, Spanish, Chinese, Vietnamese, Korean, Russian, Tagalog, French, Haitian Creole, Italian, Polish, Hindi, Cambodian, Hmong, Laotian, Samoan, Tongan.
Accessibility & Nondiscrimination Notice
Learn about the Centers for Medicare & Medicaid Services' (CMS) accessibility and nondiscrimination policies. Learn how to file a complaint if you believe you've been subjected to discrimination in a CMS program or activity.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.