Hepatocellular Carcinoma
The most common form of liver cancer often seen in people with chronic liver diseases like cirrhosis.
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
What is Medicare Advantage risk adjustment?
Feb 01, 2020 · Risk Adjustment and Hierarchical Condition Category (HCC) coding is a payment model mandated by the Centers for Medicare and Medicaid Services (CMS) in 1997. CMS requires documentation in the person's medical record by a qualified health care provider to support the submitted diagnosis.
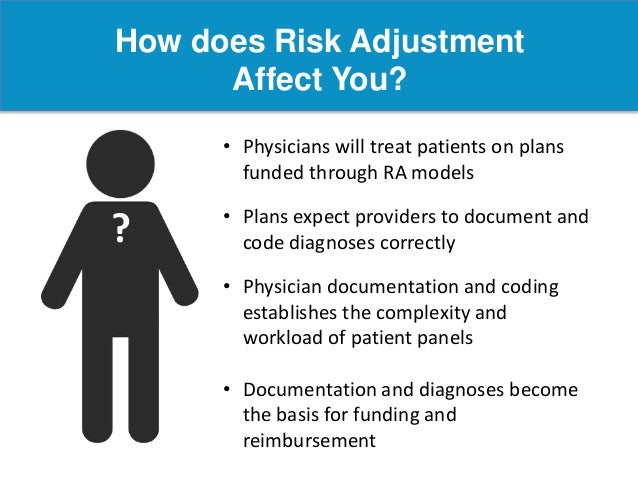
What are risk adjustment factors?
What is Risk Adjustment? An actuarial tool used to predict health care cost A process involving diagnosis reporting to measure a patient’s health status Diagnosis codes are used to adjust potential risks Risk Adjustment is a method to evaluate and measure all patients on a equal scale – levels the playing field
What is healthcare risk adjustment?
Nov 12, 2018 · In 2003, the Centers for Medicare and Medicaid Services (CMS) implemented Risk Adjustment Factors (RAF) and Hierarchical Condition Category (HCC) coding to identify individuals with serious and/or chronic illnesses and assign them a risk factor score that is based on a combination of demographic information and reported diagnoses.
What does CMS HCC mean in medical terms?
The goal of risk adjustment is to enable more accurate comparisons across TINs that treat beneficiaries of varying clinical complexity, by removing differences in health and other risk factors that impact measured outcomes but are not under the TIN’s control. This fact sheet summarizes what risk adjustment is and how it is being

What is a Medicare risk adjustment?
Risk adjustment is a statistical method that seeks to predict a person's likely use and costs of health care services. It's used in Medicare Advantage to adjust the capitated payments the federal government makes to cover expected medical costs of enrollees.Feb 17, 2022
What is risk adjustment in coding?
Risk adjustment is a process of collecting all diagnosis codes from patient charts and using these illnesses (along with their comorbidities and complications) to determine the ICD codes, which drive risk. Diagnosis codes are a good starting point for analyzing known conditions and speculating on potential risks.
What is risk adjustment coding in healthcare?
Risk adjustment is a methodology that equates the health status of a person to a number, called a risk score, to predict healthcare costs. The “risk” to a health plan insuring members with expected high healthcare use is “adjusted” by also insuring members with anticipated lower healthcare costs.Mar 8, 2021
What are the 3 main risk adjustment models?
The HHS risk adjustment methodology consists of concurrent risk adjustment models, one for each combination of metal level (platinum, gold, silver, bronze, and catastrophic) and age group (adult, child, infant). This document provides the detailed information needed to calculate risk scores given individual diagnoses.Apr 6, 2018
Why is Medicare risk Adjustment important?
In its simplest terms, risk adjustment ensures that the health conditions, health status, and demographics of the beneficiaries in a Medicare Advantage or an Affordable Care Act plan are accurately documented—and that the health plans managing those beneficiaries are adequately compensated for that management.
Why is risk adjustment coding important?
Why is HCC coding important? Hierarchical condition category coding helps communicate patient complexity and paint a picture of the whole patient. In addition to helping predict health care resource utilization, RAF scores are used to risk adjust quality and cost metrics.
What does HCC mean after a medical diagnosis?
Hierarchical Condition CategoriesHCCs, or Hierarchical Condition Categories, are sets of medical codes that are linked to specific clinical diagnoses. Since 2004, HCCs have been used by the Centers for Medicare and Medicaid Services (CMS) as part of a risk-adjustment model that identifies individuals with serious acute or chronic conditions.
What does CMS HCC mean after a diagnosis?
The CMS hierarchical condition categories (CMS-HCC) model, implemented in 2004, adjusts Medicare capitation payments to Medicare Advantage health care plans for the health. expenditure risk of their enrollees. Its intended use is to pay plans appropriately for their. expected relative costs.
How often do HCC codes need to be reported?
Active diagnoses that are risk-adjusted and affect HCC scores should be submitted at least annually after Jan. 1 to be considered for risk adjustment purposes. Non-risk-adjusted codes are submitted only when addressed or considered with an encounter.Nov 9, 2018
Which coding guidelines are followed in risk adjustment coding?
Risk adjustment coding leaders should monitor for the following common coding errors:Reporting only the primary or principal diagnosis.Coding rule-out, possible, or probable diagnosis codes from outpatient records.Coding resolved or historical conditions as current (e.g., MI or CVA)
What is the difference between CMS HCC and HHS HCC?
Type of Spending—The CMS-HCCs are configured to predict non-drug medical spending. The HHS-HCCs predict the sum of medical and drug spending. Also, the CMS-HCCs predict Medicare provider payments while the HHS-HCCs predict commercial insurance payments.
What is Medicaid risk adjustment?
Medicaid risk adjustment identifies the demographics of an enrollee and uses different values of risk score calculation for disabled individuals, adults, and children. The Medicaid risk adjustment model is concurrent in that the current year’s diagnoses affect the current year’s risk score.
What is risk adjustment contract?
Remember that the risk adjustment contract is between the program agency (state or federal government) and the health plan. If payments based on diagnoses are not supported in a RADV, the program agency will recoup overpayments from the health plan, not the provider.
What is the purpose of capturing diagnoses in an HCC model?
The purpose of capturing diagnoses in an HCC model is to offer an accurate assessment of the patient’s health status, and correct reporting of diagnosis codes is essential to this process. Not every one of the more than 70,000 diagnosis codes available in the ICD-10-CM code set maps to an HCC to be used in HCC risk score calculation; only conditions that are costly to manage from a medical or prescription drug treatment perspective are likely to be found in the risk adjustment model’s HCC crosswalk.
What is a risk score?
A risk score is the numeric value an enrollee in a risk adjustment program is assigned each calendar year based on demographics and diagnoses (HCCs). The risk score of an enrollee resets every January 1 and is officially calculated by the state or government entity overseeing the risk adjustment program the member is enrolled in. Another term for risk score is risk adjustment factor (RAF), sometimes referred to as RAF score.
What is Medicaid Chronic Illness and Disability Payment System?
Medicaid Chronic Illness and Disability Payment System (CDPS) is the risk adjustment payment methodology states use for Medicaid beneficiaries who enroll in a Managed Care Organization (MCO). While each state has its own set of eligibility criteria, in general, Medicaid (the federal branch of CMS partnering with states) provides health coverage for qualified low-income families and children, pregnant women, the elderly, and people with disabilities. Medicaid beneficiaries may enroll or disenroll at any time. Applying for Medicaid can be done on the Marketplace exchange.
What is the formula used to compare a plan's risk score to the average across all plans?
According to the National Health Council, CMS applies a formula to compare each plan’s average risk score to the average across all plans. Typically, if a plan’s risk score is higher than the average risk score for all plans in their state, the plan gets additional money called a transfer payment.
When was commercial risk adjustment created?
Commercial risk adjustment was created by the Patient Protection and Affordable Care Act (ACA) of 2010 and implemented in 2014. This type of payment model serves individuals and small groups who purchase insurance through the online insurance exchange called the Health Insurance Marketplace.
What is risk adjustment factor?
Using the Medicare risk adjustment factor system a “risk score” is chosen for each beneficiary according to the patient’s demographics, health status, and other clinical factors. The beneficiary’s risk score depicts the patient’s predicted health costs compared to those of an average beneficiary.
What does a higher category risk score mean?
Higher category risk scores represent higher anticipated healthcare costs. For example, a diabetes diagnoses, including complications, has a higher risk score and in turn greater anticipated Medicare risk and healthcare costs than diabetes without complications. HCCs are a grouping of clinically related diagnosis with similar associated cost to ...
What is an HCC in Medicare?
HCCs are a grouping of clinically related diagnosis with similar associated cost to the healthcare system. Only those ICD codes that map to an HCC category are used in the risk adjustment processing system. Not every diagnosis will “risk adjust,” or map to an HCC in the Medicare risk adjustment model. Some illnesses and injuries may not be ...
What are HCCs?
Hierarchical Condition Categories are a set of clinical codes that correspond to specific medical diagnoses. Used by the Centers for Medicare and Medicaid Services since 2004, HCCs apply a risk-adjustment model that identifies patients with chronic or serious conditions.
What is Risk Adjustment?
Risk adjustment applies a methodology to assign a risk score to the health status of a person, projecting the healthcare costs that may be incurred. This way, adjustments are made to patients with anticipated lower healthcare costs as well as predicting the risk associated with a patient with expected high healthcare costs.
HCC Structure
The HCC structure uses two main sources of data to decide a patient’s risk factors: health status and demographic characteristics. The health status is based on the ICD-10-CM diagnosis codes and the demographic data incorporates information such as age, gender, and so on.
HCC Coding Guidelines
When it comes to the actual coding of HCCs, there are three base steps involved:
Conclusion
HCC aims for an overall better health management process plus accurate reimbursements from Medicare Advantage plans. To achieve this goal, responsibility rests on the healthcare providers to ensure that they apply appropriate diagnosis codes along with complete documentation.
Why are patients assigned to more than one category?
Patients are often assigned to more than one category because the combination of demographic information and risk factors can cumulate to represent more than one kind of illness or potential for illness.
Is HCC coding good?
Since costs can vary widely among patients, risk adjustment can now be used to evaluate patients on an equal scale. It opens up a world of new opportunities for coders and providers and may make reimbursements more efficient. And that’s good news for your revenue cycle performance.