Does the insurance EOB correspond to the dates of service/services?
The Insurance EOB Does Not Correspond To The Dates Of Service/servicesBeing Billed. Denied. These Supplies/items Are Included In The Purchase Of The Dme Item Billed On The Same Date Of Service (DOS).
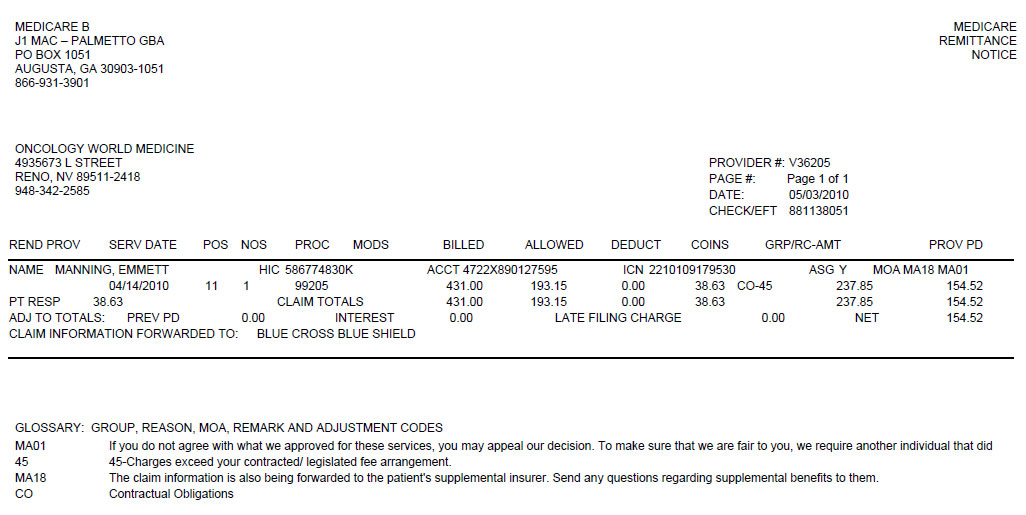
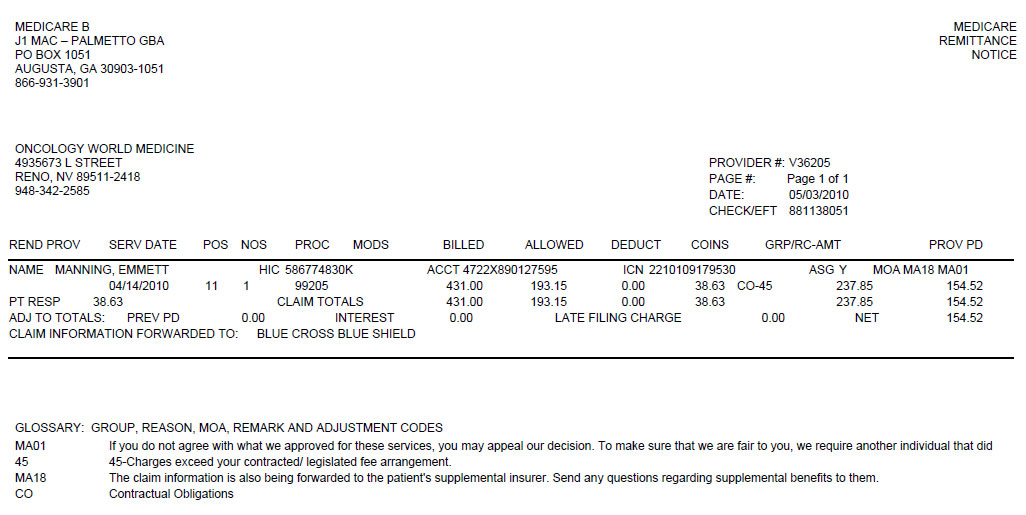
What is an explanation of Benefits (EOB)?
Each month you fill a prescription, your Medicare Prescription Drug Plan mails you an "Explanation of Benefits" (EOB). This notice gives you a summary of your prescription drug claims and costs. When should I get it? Who sends it? What should I do if I get this notice? Review your notice and check it for mistakes.
What is the difference between N16 and N17 for Medicare?
N16 Family/member Out-of-Pocket maximum has been met. Payment based on a higher percentage. N17 Per admission deductible. N18 Payment based on the Medicare allowed amount. N19 Procedure code incidental to primary procedure. N20 Service not payable with other service rendered on the same date.
What does N31 mean on a Medicare claim form?
N31 Missing/incomplete/invalid prescribing provider identifier. N32 Claim must be submitted by the provider who rendered the service. N33 No record of health check prior to initiation of treatment. N34 Incorrect claim form for this service. N35 Program integrity/utilization review decision. payment.
What does denial code N541 mean?
Claim Adjustment Reason Code P6, Reason and Remark Code N541: Mismatch between the submitted insurance type code and the information stored in our system.
What are Medicare remark codes?
Remittance Advice Remark Codes (RARCs) are used in a remittance advice to further explain an adjustment or relay informational messages that cannot be expressed with a claim adjustment reason code. Remark codes are maintained by CMS, but may be used by any health plan when they apply.
What is Claim Adjustment Reason code?
Claim adjustment reason codes (CARCs) communicate an adjustment, meaning that they must communicate why a claim or service line was paid differently than it was billed.
What are reason codes?
Reason codes, also called score factors or adverse action codes, are numerical or word-based codes that describe the reasons why a particular credit score is not higher. For example, a code might cite a high utilization rate of available credit as the main negative influence on a particular credit score.
Where would you find remark codes?
The list of remark codes is available at http://www.cms.hhs.gov/medicare/edi/hipaadoc.asp and http://www.wpc-edi.com/hipaa/, and the list is updated each March, July, and November.
How do you read an EOB for dummies?
1:342:35How to Read Your Medical EOB - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe amount you pay for the service this is the amount that you will be billed. Remember the EOB isMoreThe amount you pay for the service this is the amount that you will be billed. Remember the EOB is not a bill it just shows you how the costs are distributed. If you have any questions by your EOB.
What does Medicare adjustment mean?
"Adjustment" (discount) refers to the portion of your bill that your hospital or doctor has agreed not to charge. Insurance companies pay hospital charges at discounted rate.
What is adjustment code in medical billing?
A national administrative code set that identifies the reasons for any differences, or adjustments, between the original provider charge for a claim or service and the payer's payment for it.
How often are claim adjustment reason codes and remark codes updated?
Claim adjustment reason codes and remark codes are updated three times each year.
What are the most common errors when submitting claims?
Common Errors when Submitting Claims:Wrong demographic information. It is a very common and basic issue that happens while submitting claims. ... Incorrect Provider Information on Claims. Incorrect provider information like address, NPI, etc. ... Wrong CPT Codes. ... Claim not filed on time.
What does CO 59 mean on EOB?
Processed based on multiple or concurrent procedure rulesCO 59 – Processed based on multiple or concurrent procedure rules. Reason and action: This is Multiple surgeries detected, hence confirm with coding guideliness and take the necessity action.
What is reason code A1?
Description. Reason Code: A1. Claim/Service denied. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Remark Code: N370.
Why is my Medicare MSP claim rejected?
If you answered "Yes" to any of the above questions, your Medicare MSP claims are most likely rejecting because there is a mismatch of the type submitted and the Medicare MSP files. This situation can drastically impact the cash flow for your office.
What to do if you are receiving rejections from Medicare?
If you are still receiving rejections from Medicare, verify that your clearinghouse is submitting the MSP Type you provided for each patient.
How long does it take to refund Medicare payment to Palmetto GBA?
If you receive two primary payments, you should refund Medicare’s payment in full. Refund the Medicare payment to Palmetto GBA within 60 days of the date you identify the overpayment, even if Medicare’s records show that Medicare is primary.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) refers to instances in which Medicare does not have primary responsibility for paying the medical expenses of a Medicare beneficiary. This is because the Medicare beneficiary may be entitled to other coverage, which should pay the primary health benefits.
What is the number to call to check Medicare records?
If you find that there is a discrepancy between Medicare records and the patient's current insurance status, call the BCRC Contractor at 855–798–2627 or TDD/TYY 855–797–2627. The BCRC Contractor may also need to speak to the patient.
Can I get Medicare claim status through IVR?
Remember, you can obtain claim status information through the IVR at any time. If Medicare records show that Medicare is primary for the patient, Palmetto GBA will request that these records (Common Working File [CWF] records) be updated to reflect that Medicare is secondary.
Is Medicare a no fault situation?
No-Fault Situations: Medicare is secondary if illness/injury results from a no-fault liability. This type would most likely not be submitted to Palmetto GBA because we will pay services conditionally, as primary, based on your decision to submit the claim to Medicare for the Liability situation.
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.