Many Medicare beneficiaries won’t have to pay the increased prices during the coverage gap because their prescription drug costs won’t reach the initial coverage limit of $4,020 in 2020. People who qualify for Extra Help (or the Low-Income Subsidy) will avoid the coverage gap.
Full Answer
What does no gap coverage mean Medicare?
Jan 17, 2022 · What is Gap Coverage? Gap coverage is insurance that covers more than the standard amount of your medications. This type of coverage isn’t available in all areas. The coverage gap isn’t going to affect everyone. You’re most likely to enter the gap if you have a lot of medications or if you have several high-cost medications like brand-name or specialty tier drugs.
How to cover the gaps in Medicare?
Dec 12, 2019 · The coverage gap is a temporary limit on what most Medicare Part D Prescription Drug Plans or Medicare Advantage Prescription Drug plans pay for prescription drug costs. This gap will officially close in 2020, but you can still reach this out-of-pocket threshold where your medication costs may change.
Do I need ful coverage if I have GAP insurance?
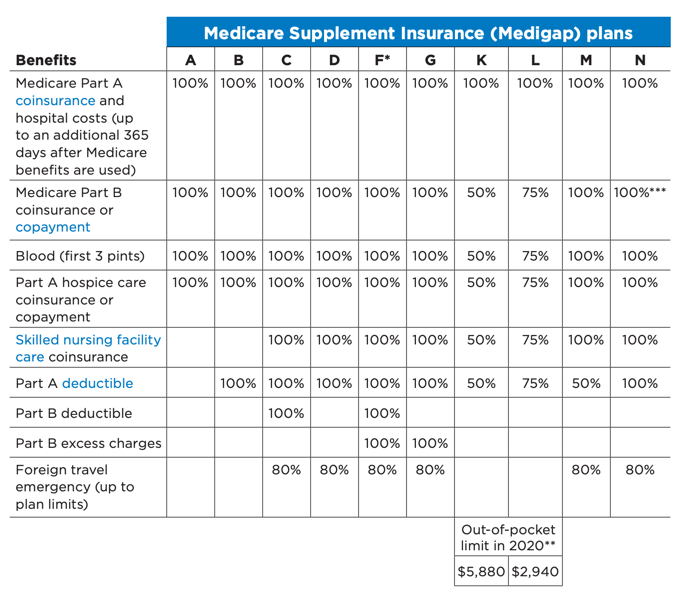
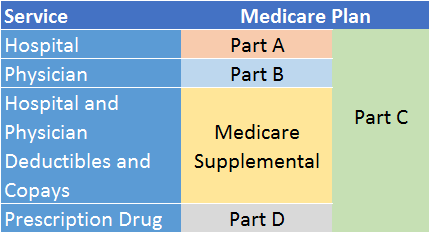
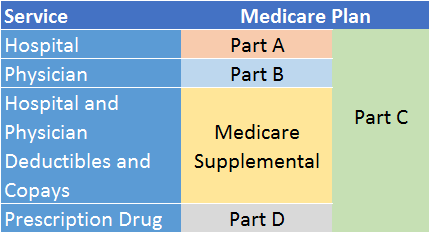
Medigap is Medicare Supplement Insurance that helps fill "gaps" in. Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and ...
How much does gap coverage cost?
that has a coverage gap. The other 72% of people with Medicare will not have a coverage gap. These people have coverage from former employers, are getting extra help because they have limited income and resources, or are in a Medicare drug plan that provides some type of coverage during the gap. People who have limited income
How do I avoid the Medicare donut hole?
Five Ways to Avoid the Medicare Part D Coverage Gap (“Donut Hole”...Buy generic prescriptions. Jump to.Order your medications by mail and in advance. Jump to.Ask for drug manufacturer's discounts. Jump to.Consider Extra Help or state assistance programs. Jump to.Shop around for a new prescription drug plan. Jump to.
What is the Medicare donut hole for 2021?
For 2021, the coverage gap begins when the total amount your plan has paid for your drugs reaches $4,130 (up from $4,020 in 2020). At that point, you're in the doughnut hole, where you'll now receive a 75% discount on both brand-name and generic drugs.
Does the Medicare donut hole reset each year?
Your Medicare Part D prescription drug plan coverage starts again each year — and along with your new coverage, your Donut Hole or Coverage Gap begins again each plan year. For example, your 2021 Donut Hole or Coverage Gap ends on December 31, 2021 (at midnight) along with your 2021 Medicare Part D plan coverage.
How does the coverage gap work?
Once you reach the coverage gap, you'll pay no more than 25% of the cost for your plan's covered brand-name prescription drugs. You'll pay this discounted rate if you buy your prescriptions at a pharmacy or order them through the mail. Some plans may offer you even lower costs in the coverage gap.
Has the donut hole been eliminated?
The Medicare donut hole is closed in 2020, but you still pay a share of your medication costs.
What happens when you reach the donut hole?
How does the donut hole work? The donut hole closed for all drugs in 2020, meaning that when you enter the coverage gap you will be responsible for 25% of the cost of your drugs. In the past, you were responsible for a higher percentage of the cost of your drugs.
What is the Medicare donut hole for 2022?
$4,430In 2022, you'll enter the donut hole when your spending + your plan's spending reaches $4,430. And you leave the donut hole — and enter the catastrophic coverage level — when your spending + manufacturer discounts reach $7,050. Both of these amounts are higher than they were in 2021, and generally increase each year.
Is the donut hole going away in 2022?
In 2022, the coverage gap ends once you have spent $7,050 in total out-of-pocket drug costs. Once you've reached that amount, you'll pay the greater of $3.95 or 5% coinsurance for generic drugs, and the greater of $9.85 or 5% coinsurance for all other drugs. There is no upper limit in this stage.
How long does the donut hole last in Medicare?
When does the Medicare Donut Hole End? The donut hole ends when you reach the catastrophic coverage limit for the year. In 2022, the donut hole will end when you and your plan reach $7,050 out-of-pocket in one calendar year.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Is there still a donut hole in Medicare Part D?
The Part D coverage gap (or "donut hole") officially closed in 2020, but that doesn't mean people won't pay anything once they pass the Initial Coverage Period spending threshold. See what your clients, the drug plans, and government will pay in each spending phase of Part D.
Do Medicare Advantage plans cover the donut hole?
Some people ask: Do Medicare Advantage plans cover the donut hole? If you choose to include Medicare prescription drug coverage in your Medicare Advantage plan, it will still have a donut hole just like a regular Part D plan. Medicare Advantage does not cover any additional Part D costs during the coverage gap.
What Is The Coverage Gap (“Donut Hole”), and When Does It Start?
For those who are new to the coverage gap, or “donut hole,” learning about the different Medicare Part D coverage phases is a good place to start....
What Costs Count Towards Getting Out of The Coverage Gap (“Donut Hole”)?
Once you’ve entered the coverage gap (“donut hole”), it’s important to understand which out-of-pocket costs count towards helping you reach the cat...
What Costs Don’T Count Towards Getting Out of The Coverage Gap (“Donut Hole”)?
Not all out-of-pocket costs count towards reaching catastrophic coverage. The following costs don’t count towards getting you out of the coverage g...
How Do I Avoid The Medicare Part D Coverage Gap (“Donut Hole”)?
Now that you know about the coverage gap (“donut hole”), here is some good news: 1. Many Medicare beneficiaries won’t have to pay the increased pri...
What If I Have Questions About The Coverage Gap (“Donut Hole”)?
If you have questions about how the coverage gap works and how to avoid it, I can help. A licensed insurance agent such as myself can help you comp...
What are My Costs in the Coverage Gap?
Once you reach $4,430 in total spending on your covered drugs, you’re responsible for a certain percentage of the costs. When you enter the coverage gap, you’ll pay no more than 25% of the actual drug cost.
What Plans Provide Gap Coverage?
A Part D drug plan or Part C Medicare Advantage plan may include gap coverage, though these plans aren’t available everywhere and may have a higher premium. Plans are available by location, if you don’t live in the service area, you’re not eligible for that policy.
Is the Medicare Coverage Gap Going Away?
While the coverage gap has closed, it doesn’t mean that it goes away. After the Initial Coverage Period, people with Medicare will pay a higher portion of their drug costs.
Which Plan Covers My Medications at the Lowest Cost?
There is not one specific plan that suits everyone’s needs. Most of the time spouses will find they have different plan needs. Perhaps you have a brand-name medication that fewer plans cover, or maybe there is a plan option that allows you to avoid the donut hole.
What is the coverage gap in Medicare?
Typically, each new coverage phase begins once your spending has reached a certain amount. The coverage gap is one of the coverage phases under Medicare Part D.
Why won't Medicare pay the $4,020 coverage gap?
Now that you know about the coverage gap (“donut hole”), here is some good news: Many Medicare beneficiaries won’t have to pay the increased prices during the coverage gap because their prescription drug costs won’t reach the initial coverage limit of $4,020 in 2020.
What is the deductible phase of Medicare?
Deductible phase: For most stand-alone Medicare Prescription Drug Plans and Medicare Advantage Prescription Drug plans, you’ll pay 100% for medication costs until you reach the yearly deductible amount (if your plan has one). After you reach the deductible, the Medicare plan begins to cover its share of prescription drug costs. The deductible amount may vary by plan, and some plans may not have a deductible. If your Medicare plan doesn’t have a deductible, then you’ll start your coverage in the initial coverage phase (see below).
How to avoid coverage gap?
Managing your out-of-pocket prescription drug costs is a big part of avoiding the coverage gap. Here are some tips for how you can lower the amount you spend on medications: Many expensive prescription drugs have a generic or lower-cost alternative. Switching to lower-cost drugs may help you avoid entering the coverage gap.
What is the Medicare Part D coverage gap?
The Medicare Part D Coverage Gap (“Donut Hole ”) Made Simple. Summary: When it comes to Medicare prescription drug coverage, you might have questions surrounding the Medicare Part D coverage gap, also known as the “donut hole.”. The coverage gap is a temporary limit on what most Medicare Part D Prescription Drug Plans or Medicare Advantage ...
How much is the coverage gap for 2020?
While in the coverage gap, you’ll typically pay up to 25% of the plan’s cost for both covered brand-name drugs and generic drugs in 2020. You’re out of the coverage gap once your yearly out-of-pocket drug costs reach $ 6,350 in 2020. Once you have spent this amount, you’ve entered the catastrophic coverage phase.
When will the Medicare coverage gap end?
This gap will officially close in 2020 , but you can still reach this out-of-pocket threshold where your medication costs may change. Find affordable Medicare plans in your area.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Does Medicare cover prescription drugs?
Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage. If you want prescription drug coverage, you can join a Medicare Prescription Drug Plan (Part D). If you buy Medigap and a Medicare drug plan from the same company, you may need to make 2 separate premium payments. Contact the company to find out how to pay your premiums.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Note: Medigap plans sold to people who are newly eligible for Medicare aren’t allowed to cover the Part B deductible.
How much of your prescription drug costs will you pay after you reach the coverage gap?
You’ll pay no more than 25% of your drug costs after reaching the coverage gap. The coverage gap ends when your out-of-pocket expenses for medications on the plan’s formulary reach a certain threshold, which may change each year. At this point, you enter the catastrophic coverage phase.
What is the Medicare donut hole?
Summary: Most Medicare Part D prescription drug plans include a coverage gap in Part D benefits, also known as the Medicare “donut hole.” During this gap in prescription drug coverage, beneficiaries may have to pay more of their prescription drug costs until they reach the catastrophic coverage phase of their plan.
Can Medicare Part D beneficiaries enter the prescription drug coverage gap?
Each year , Medicare Part D beneficiaries may enter the prescription drug coverage gap if they and their drug plan have paid a specified amount on covered drugs.
Can Medicare save you money on prescriptions?
Don’t let the Part D coverage gap alarm you too much; a Medicare prescription drug plan can still save you money on your medications.
Will everyone enter the Medicare coverage gap?
Not everyone will enter the Medicare coverage gap, or “donut hole,” each year. For example, Medicare beneficiaries who get Extra Help paying for Part D costs won’t enter this coverage gap. Here are some ways you may be able to save money on prescription drugs:
Do you pay coinsurance on Medicare prescriptions?
In the catastrophic coverage phase of a Medicare prescription drug plan, you only pay a small coinsurance or copayment on covered medications for the rest of the calendar year.
How to fill gaps in Medicare?
The best way to fill in the gaps Medicare leaves open is to obtain a Medicare Supplement policy. As the name Medigap would suggest, these plans fill in the holes in coverage. There are several different plan options for Medigap, offering varying amounts of coverage for a range of monthly premium prices. As you might expect, the plans that cover more benefits are higher in cost.
What is a donut hole in Medigap?
The donut hole refers to a phase in prescription drug coverage when the beneficiary must pay a certain percentage for drugs. This phase ends when the total amount spent on drugs in the year reaches a specific threshold, and the following stage, catastrophic coverage, begins.
How long does Medicare cover skilled nursing?
Medicare alone only offers up to 20 days of full coverage for this care, after which you’re responsible for coinsurance payments each day until coverage runs out on the hundredth day.
What is a Medigap plan?
A Medigap plan will cover what Medicare leaves for the patient in hospital and outpatient settings. Specifically, it works with your Medicare to ensure one hundred percent of your standard health care costs are handled. Plus, these plans include additional coverage that can save you a great deal of money in the future. In the content below, we will explain three ways gap coverage can help you save money and secure your future.
How many days do you have to be in the hospital for Medicare?
On standard Medicare, each day in the hospital after the first 60 days costs hundreds of dollars in coinsurance. After 90 consecutive days, you’ll need to start using your lifetime reserve days, of which Medicare provides 60.
How long does Medicare Supplement cover travel?
The lifetime limit is $50,000. With this coverage, your plan will pay the greater portion of your medical bills outside of the U.S. for up to 60 days at a time.
Does Medicare cover gap?
Many people believe they’ll receive coverage for all their health care expenses once they’re on Medicare. The reality is there are several costs that Medicare alone doesn’t cover. Thus, beneficiaries must pay these out-of-pocket.
What is a Medicare Part D gap?
When Medicare Part D prescription drug plans first became available, there was a built-in gap in coverage. This coverage gap opened after initial plan coverage limits had been reached and before catastrophic coverage kicked in. While in this gap, plan members had to pay the full cost of their covered drugs until their total costs qualified them ...
What is phase 3 coverage gap?
Most Medicare drug plans have a coverage gap (also called the "donut hole"). This means there's a temporary limit on what the drug plan will cover for drugs. Not everyone will enter the coverage gap, and it doesn’t apply to members who get Extra Help to pay for their Part D costs. Once in the gap, you’ll pay no more ...
What is the limit for Part D coverage in 2021?
If the combined amount you and your drug plan pay for prescription drugs reaches a certain level during the year—that limit is $4,130 in 2021—you enter the Part D coverage gap or “donut hole.”.
How much is a deductible for 2021?
The deductibles vary between plans and some Part D plans have no deductible. In 2021, the deductible can’t be more than $445.
Is the Affordable Care Act closing the donut hole?
Where members once paid 100% of their costs in the gap, now their share of costs in the donut hole is limited to 25% for both brand-name and generic drugs. The donut hole has essentially closed. 2
What is a donut hole in Medicare?
What Is the Medicare Part D “Donut Hole”? Most Medicare Part D prescription drug plans have a coverage gap. More commonly, this has been known as the “donut hole.”. The “donut hole” essentially refers to where a drug plan may reach its limit on what it will cover for drugs. Once you and your Medicare Part D plan have spent a certain amount on ...
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How much does Medicare pay for generic drugs?
For generic drugs: You’ll pay 25% of the price. Medicare pays 75% of the price. Only the amount you pay will count towards getting you out of the “donut hole.”. NOTE: Some plans may have coverage in the gap, so if this is true for you, you will get a discount after the plan’s coverage has been applied to the drug’s price. ...
How much does it cost to leave the Donut hole?
In order to leave the “donut hole,” your total out-of-pocket costs much reach $6,550. If you hit this number, then you enter the catastrophic payment stage. Your plan pays most of the cost for your drugs in the catastrophic stage. You may pay a small copay or coinsurance, and you will remain in this stage for the rest of the year.
Is the Donut hole going away?
The “donut hole” isn’t really going away, because Medicare Part D still has four payment stages. The “donut hole” is the third stage, and you move through the Part D payment stages based on how much you, your plan, and others on your behalf have paid for your drugs during the year.
Do copays count toward dollar limits?
You may pay a small copay or coinsurance, and you will remain in this stage for the rest of the year. Your out-of-pocket drug costs, including copays, coinsurance amounts and your deductible, if any, count toward the dollar limits. Other amounts that contribute to reaching the limits include:
How to request a network gap exception?
The information you’ll need at hand when requesting a network gap exception includes: 1 The CPT or HCPCS code describing the healthcare service or procedure you need. 2 The ICD-10 code describing your diagnosis. 5 3 The out-of-network provider’s contact information. 4 A date range during which you expect to receive the requested service. For example, from February 1, 2021, to July 31, 2021. 5 The names of any in-network providers of the same specialty within your geographic area along with an explanation as to why that particular in-network provider isn’t capable of performing the service.
Why is my health insurance denied?
Sometimes, requests are denied for a simple reason such as: The insurer was unable to contact the out-of-network provider’s office. The insurer thinks there are in-network providers capable of providing the same service.
What is a PPO plan?
Some insurers offer very robust networks with a PPO design that allows members to access care outside the network, while others offer plans with much more limited networks and an HMO or EPO design that requires members to use an in-network provider (or obtain a network gap exception).
What happens if you see an out of network provider?
Without a network gap exception, when you see an out-of-network provider, you’ll pay more than you would have paid if you had used an in-network provider. If you have an HMO or an EPO, your health plan likely won’t pay one dime of the cost of your non-emergency out-of-network care unless you get a network gap exception. If you have a PPO or POS plan, your health plan will help you pay for the care you get out-of-network, even without a network gap exception. 2 However, your deductible, coinsurance, and copayments will be significantly larger when you use an out-of-network provider than when you use an in-network provider.
What does an insurer think of in-network providers?
The insurer thinks there are in-network providers capable of providing the same service.
Does a PPO plan cover out of network care?
If you have a PPO or POS plan, your health plan will help you pay for the care you get out-of-network, even without a network gap exception. 2 However, your deductible, coinsurance, and copayments will be significantly larger when you use an out-of-network provider than when you use an in-network provider. ...
Can a health plan grant a network gap exception?
First, be aware that your health plan isn’t going to be eager to grant a network gap exception. It’s extra work for them, and it might end up being expensive for them as well. However, if the health plan doesn’t have an in-network provider that's in your area or if that provider isn't capable of providing the healthcare service that you need, it’s not fair to make you pay higher cost-sharing just because the health plan doesn’t have a sufficiently robust provider network. So, insurers can grant a network gap exception to allow you to get the care you need from an out-of-network provider without paying more than you should have to pay.