Full Answer
What is the difference between Medicare and single payer?
Medicare provider and supplier organizations have business structures, such as corporations, partnerships, Professional Associations (PAs), or Limited Liability Companies (LLCs) that meet the “provider” and “supplier” definitions. Provider and supplier organizations don’t include organizations the IRS defines as sole proprietorships.
What is single-payer healthcare?
Single payer is a healthcare system that one entity, generally the government, is responsible for financing. In the single payer system, the government …
What is a Medicare provider and supplier organization?
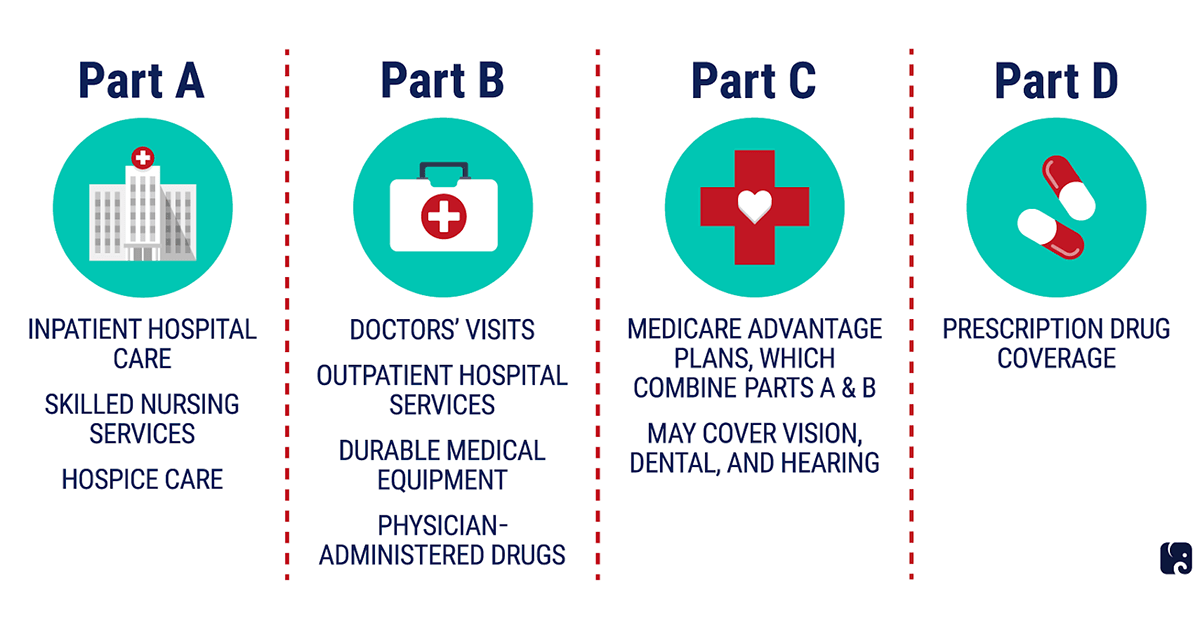
Medicare Advantage is Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage. These “bundled” plans include Part A, Part B, and usually Part D. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
What is the single payer system?
Jun 17, 2021 · Hence, you are governed by the same rules as a PAR provider and can only bill according to the allowable amounts on the Medicare Fee Schedule. However, there are some differences. As a non-PAR provider accepting assignment, you are paid 5% less than a Medicare participating provider. Also, to collect the 20% that Medicare doesn’t cover, you ...
How does Medicare define a provider?
Provider is defined at 42 CFR 400.202 and generally means a hospital, critical access hospital, skilled nursing facility, comprehensive outpatient rehabilitation facility (CORF), home health agency or hospice, that has in effect an agreement to participate in Medicare; or a clinic, rehabilitation agency, or public ...
What does Pecos mean for Medicare?
Welcome to the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) (*) Red asterisk indicates a required field. Log In. PECOS supports the Medicare Provider and Supplier enrollment process by allowing registered users to securely and electronically submit and manage Medicare enrollment information.
Is Pecos ID same as Medicare number?
The following walk-thru explains how a user can find their Medicare ID number in PECOS. Medicare numbers are also known as the CCN, P-Tan, Oscar, Provider number, or Medicare ID.
How do I know if a provider is enrolled in Pecos?
To determine if you have a current enrollment record in the PECOS, you can do the following:Utilize the national file of Medicare physicians and non-physician practitioners who are eligible to order / refer and have current enrollment records in the PECOS. ... Utilize Internet-based PECOS.More items...•Nov 17, 2017
What is Pico certified?
PECOS stands for Provider, Enrollment, Chain and Ownership System. It is a database where physicians register with the Centers for Medicare and Medicare Services (CMS). CMS developed PECOS as a result of the Patient Protection and Affordable Care Act.
What does Nppes stand for?
CMS developed the National Plan and Provider Enumeration System (NPPES) to assign NPIs.
What does a Medicare ID number look like?
On a Medicare card, an MBI will appear similar to this: 1EG4-TE5-MK73. The second, fifth, eighth, and ninth characters are always letters while the first, fourth, seventh, tenth, and eleventh characters are always numbers. You can visit cms.gov for more information on the format of an MBI.
Is the Medicare provider number the same as NPI?
What are the NPI and CCN numbers? The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
How do I verify a Medicare number?
Members can check their Medicare ID number by signing into myMedicare.gov. If a member doesn't have a myMedicare.gov account yet, they can 'create an account' and follow the instructions. For questions, members can call 1-800-MEDICARE (800-633-4227 TTY 877-486-2048).
What is Pecos NPI?
PECOS stands for Provider Enrollment and Chain/Ownership System. NPI: First Name: Last Name: Search.
What is Pecos enrolled?
PECOS is the online Medicare enrollment management system which allows you to: Enroll as a Medicare provider or supplier. Revalidate (renew) your enrollment. Withdraw from the Medicare program. Review and update your information.Dec 1, 2021
How do I disenroll from Medicare as a provider?
Withdrawing from Medicare?Providers/Organizations terminating a reassignment of benefits submit the.Providers terminating a solo practice submit the.Physician Assistants terminating employment with an organization submit the.Organizations terminating employment with a physician assistant submit the.More items...•Feb 13, 2020
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
What is a coba?
The Coordination of Benefits Agreement (COBA) Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the trading partners. The COBA Trading Partners document in the Download section below provides a list of automatic crossover trading partners in production, their identification number, and customer contact name and number. For additional information, click the COBA Trading Partners link.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
Does BCRC process claims?
The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What are the benefits of single payer healthcare?
Benefits of single payer healthcare. The main benefit of the single payer system is the provision of health insurance for everyone in the country. In an average month in 2018, approximately 29 million people under the age of 65 years in the U.S. had no health insurance, notes the Congressional Budget Office. A single payer system could greatly ...
What is single payer vs multiple payer?
Single payer vs. multiple payer. Single payer is a healthcare system that one entity, generally the government, is responsible for financing. In the single payer system, the government pays for medical services using money from taxes. However, as the government does not own or operate the system, it does not employ doctors ...
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What stakeholders are involved in the transition to single payer?
These stakeholders include health insurance and pharmaceutical companies, who are significant lobbyists in government.
What is Medicare for older people?
Medicare is health insurance in the United States for people aged 65 years and older, as well as some younger people with certain medical conditions. Some members of Congress and a portion of the U.S. population are interested in changing the country’s current healthcare system to one that would provide coverage for most residents, ...
What are the barriers to a single payer system?
One of the possible barriers to a single payer or Medicare for All system is the possibility of people paying higher taxes rather than having employers pay for health insurance. While many predictive models find that individuals could save money under such a system, voters tend to be concerned about the high cost to taxpayers.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is Medicare Participating Provider?
What is a Medicare Participating Provider? Enrolling as a Medicare participating provider means that you are in-network with the plan. You may also see this listed as a PAR provider. PAR stands for participating, and as such, your practice has a contract with Medicare.
How much less is a non-PAR provider than a Medicare provider?
However, there are some differences. As a non-PAR provider accepting assignment, you are paid 5% less than a Medicare participating provider. Also, to collect the 20% that Medicare doesn’t cover, you must go directly to the patient versus being able to bill their secondary insurance.
What is PAR provider contract?
As part of your PAR provider contract, your practice agrees to take assignment on all Medicare claims. This means you must accept the amount that Medicare assigns for payment for the services you provide.
What happens if you choose the wrong Medicare provider?
Choosing the wrong Medicare participation status for your provider can have significant financial consequences for your practice. Your choices are a Medicare Participating Provider (PAR) or a Medicare Non-Participating Provider (non-PAR). If you make the wrong choice, your allowable reimbursement can be limited, ...
How often does Medicare revalidate?
In addition to enrollment, the revalidation process – which occurs every five years in Medicare’s Provider Enrollment, Chain and Ownership System (PECOS) – also requires you to choose your participation status. Failure to revalidate can lead to deactivation from Medicare and the loss of reimbursement funds.
What does it mean if you don't accept Medicare assignment?
Non-PAR NOT Accepting Medicare Assignment: If you don’t want to accept assignment, this means that you’ll bill and get paid by the patient. For those providers that choose not to accept assignment, the federal government has a “limiting charge” amount set for the services you provide to its beneficiaries.
What should you consider when choosing a Medicare participation designation?
When deciding which Medicare participation designation is right for your practice, it is essential that you break down how and what you’ll be paid by each option. Items you should consider include: Total Medicare potential reimbursement. Total secondary potential reimbursement.
Why is continuity of care important in ABA?
There are many therapeutic processes like ABA therapy where continuity of care is critical for meeting treatment goals. When a client changes to a new insurance provider, maintaining continuity of care, or establishing a transition plan to a new in-network provider, is essential. In many of these scenarios a single case agreement often needs ...
Can you charge insurance for backdated sessions?
Though you cannot charge their insurance provider the standard full rate for any back-dated, past sessions. It’s also important to note that some insurance providers have standard protocols in place for a single case agreement negotiation. Some have a “Pay At The Highest Rate” as if you were an in-network provider.
Can a client find a practitioner in their network?
The client has tried and cannot find a practitioner or provider in their network that meets their needs in a manner they are comfortable with. In the case of ABA therapy, this needs to be done before starting therapy.
Where Can I Find My Medicare Number
The red, white, and blue Medicare card has your Medicare number on it.
When Will I Receive My Medicare Card
If automatically enrolled in Medicare, Medicare will mail your card to you either three months before your 65th birthday or just before you reach your 25th month of receiving disability benefits.
What Is My Medicare Beneficiary Identification Number
Your Medicare Beneficiary Identifier number is for billing and identification purposes.
Applying For Your National Provider Identifier
Whether youre just beginning your physical therapy career or are a seasoned veteran, having your NPI number should be a priority.
National Provider Identifier Standard
The National Provider Identifier is a Health Insurance Portability and Accountability Act Administrative Simplification Standard. The NPI is a unique identification number for covered health care providers.
Where Can You Find Your Medicare Claim Number
Your Medicare claim number, or Medicare Beneficiary Identifier is an 11-character number Medicare uses to identify you. Learn how to find your number and how to use it to file a Medicare claim or track your Medicare claim status.
Other Ways To Obtain A Medicaid Provider Number
The Centers for Medicare & Medicaid Services has 10 regional offices in different cities and states 2. Atlanta, Chicago and New York are just a few to mention. If you want to enroll in the Medicare provider services program in person, go to the nearest regional office.

Coordination of Benefits Overview
- The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken ...
Information Gathering
- Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare. For example, information submitted on a medical claim or from other sour…
Provider Requests and Questions Regarding Claims Payment
- MACs, intermediaries, and carriers will continue to process claims submitted for primary or secondary payment. Claims processing is not a function of the BCRC. Questions concerning how to bill for payment (e.g., value codes, occurrence codes) should continue to be directed to your local Medicare claims paying office. In addition, continue to return inappropriate Medicare paym…
Medicare Secondary Payer Records in CMS's Database
- The BCRC is the sole authority to ensure the accuracy and integrity of the MSP information contained in CMS's database (i.e., Common Working File (CWF)). Information received because of MSP data gathering and investigation is stored on the CWF. MSP data may be updated, as necessary, based on additional information received from external parties (e.g., beneficiaries, pr…
Termination and Deletion of MSP Records in CMS's Database
- Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office. MSP records that you have identified as invalid are reported to the BCRC for investigation and deletion.
Contacting The BCRC
- The BCRC’s trained staff will help you with your COB questions. Whether you need a question answered or assistance completing a questionnaire, the Customer Service Representatives are available to provide you with quality service. Click the Contactslink for BCRC contact information. In order to better serve you, please have the following information available when you call: 1. Yo…
Contacting The Medicare Claims Office
- Contact your local Medicare Claims Office to: 1. Answer your questions regarding Medicare claim or service denials and adjustments. 2. Answer your questions concerning how to bill for payment. 3. Process claims for primary or secondary payment. 4. Accept the return of inappropriate Medicare payment.
Coba Trading Partner Contact Information
- The Coordination of Benefits Agreement (COBA) Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the t…
mln Matters Articles - Provider Education
- The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matterslink.