
Step Therapy is a utilization management restriction that your Medicare Part D prescription drug plan can add to a formulary medication. If you have a formulary drug subject to Step Therapy, you are required to try a less-expensive medication before the drug plan will pay for the formulary drug that your doctor may have originally prescribed.
What is part B Step therapy?
The new policy rescinds a 2012 memo prohibiting the use of step therapy. Part B drugs are those administered by a physician or in a clinical setting; they’re typically intravenous medications. Medicare Part D is the prescription drug program for medications beneficiaries get from a pharmacy. Part D plans already employ step therapy practices.
How to start my Medicare?
Try these tips in your 30s:
- Reassess your budget and if there’s spending that doesn’t align with your values, cut out those low-priority expenses
- Look for ways to boost your income. Can you ask for a raise? ...
- Diversify your retirement accounts; if you have access to a 401 (k) at work, take advantage of it, especially if there’s a match. ...
What is prescription drug step therapy?
- Allergies
- Asthma
- COPD
- Cardiovascular health
- Diabetes
- High cholesterol
- Mental health issues
- Bladder problems
- Acid reflux and heartburn
What is the definition of step therapy?
What is Step Therapy? Step therapy is a type of prior authorization for drugs that begins medication for a medical condition with the most preferred drug therapy and progresses to other therapies only if necessary, promoting better clinical decisions.
How does step therapy work?
Step therapy is a program for people who take prescription drugs regularly to treat a medical condition, such as arthritis, asthma or high blood pressure. It allows you and your family to receive the affordable treatment you need and helps your organization continue with prescription-drug coverage.
What is an example of a step therapy?
Step therapy is trying lower-priced medications before taking a step up to one that costs more. Here's an example of step therapy: You take a generic drug to lower your cholesterol, but it's not working. Your doctor prescribes another medication, but it's still not working.
What is step therapy CMS?
Step therapy is a utilization management tool that allows a plan to require an enrollee to try a different, less expensive drug that treats the same condition before it will cover a more expensive drug.
What is the difference between prior authorization and step therapy programs?
Automation of prior authorization for medications is referred to as electronic prior authorization. Step therapy is an insurance protocol that requires patients to try one or more insurer-preferred medications prior to a physician recommendation. This practice is also known as “fail first” and can take weeks or months.
What is step therapy criteria?
Step therapy is a type of prior authorization for drugs that begins medication for a medical condition with the most preferred drug therapy and progresses to other therapies only if necessary, promoting better clinical decisions.
What is Aetna step therapy?
How step therapy works. One of these special requirements or coverage limits is known as step therapy, where we require a trial of a preferred drug to treat a medical condition before covering another non-preferred drug.
What is prior authorization?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What's the phone number to Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
What is step therapy exception?
A step therapy exception request is needed when the prescriber is requesting coverage of a drug that has “step therapy” or requires a person to try the most cost-effective medication(s) in a certain order before coverage of (or “stepping up to”) the less cost-effective medication is granted.
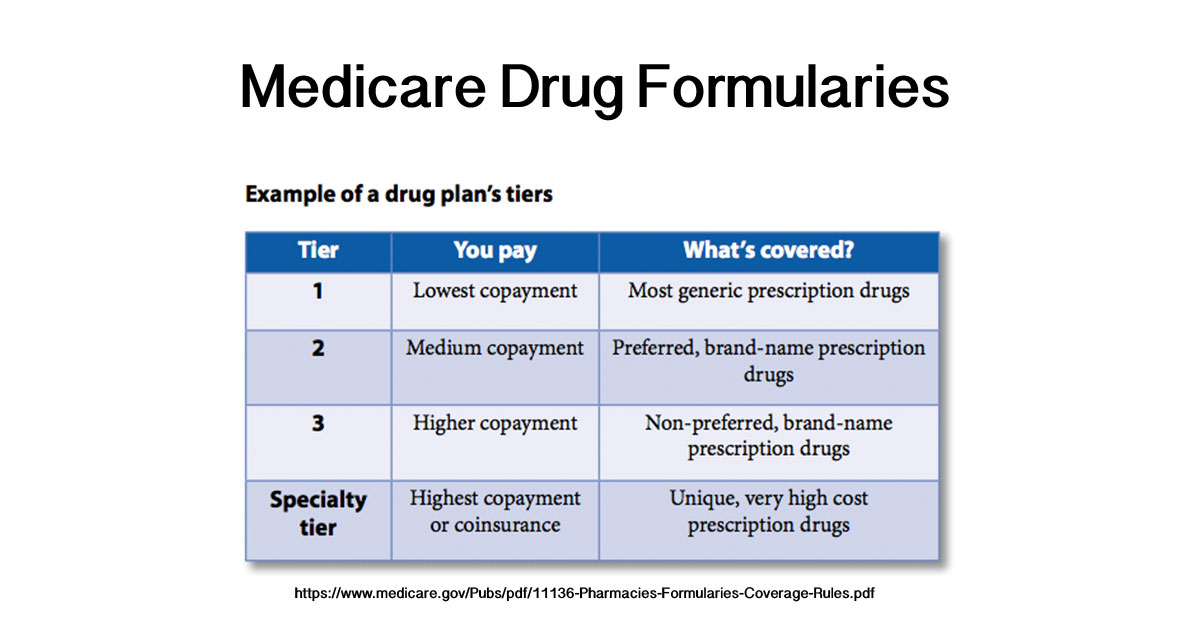
What are Tier 4 and 5 drugs?
Level or Tier 4: Nonpreferred brand-name drugs and some nonpreferred, highest-cost generic drugs. Level or Tier 5: Highest-cost drugs including most specialty medications.
How are formularies established?
The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties. This committee evaluates and selects new and existing medications for what is called the (health plan's) formulary.
What is step therapy?
Step therapy is trying lower-priced medications before taking a step up to one that costs more. Here’s an example of step therapy: You take a generic drug to lower your cholesterol, but it's not working. Your doctor prescribes another medication, but it's still not working. Your doctor prescribes a different medication that works well.
Can you prescribe a drug that doesn't require step therapy?
There may be another drug they can prescribe that doesn't require step therapy. If not, you can call the number on the back of your Blue Cross ID card to start the approval process and tell us the information we need. You can also start the approval process by filling out and sending in a coverage determination form.
Does step therapy cover drug costs?
In this case, you have. If you don't follow the procedure for step therapy when it's required, the drug may cost you more, or may not be covered at all.
When will Medicare start implementing step therapy?
Medicare Advantage (MA) plans will have the choice of implementing step therapy to manage Part B drugs, beginning January 1, 2019 as part of broader care coordination activities that include patient rewards and incentives. Currently, there are more than 20 million beneficiaries enrolled in MA plans.
What is step therapy?
Step therapy is a type of prior authorization for drugs that begins medication for a medical condition with the most preferred drug therapy and progresses to other therapies only if necessary, promoting better clinical decisions. For example, using step therapy plans could ensure that a senior who is newly diagnosed with a condition begin treatment ...
What is the CMS?
Today, the Centers for Medicare & Medicaid Services (CMS) introduced much-needed competition and negotiation into the market for physician-administered and other Part B medications that will result in better deals and lower drug costs for patients.
Can Step Therapy be used on Part B?
Under this new policy, step therapy can only be applied to new prescriptions or administrations of Part B drugs for beneficiaries that are not actively receiving the affected medication. This means that no beneficiary currently receiving drugs under part B will have to change their medication.
What Is Step Therapy?
Step therapy is a system for obtaining prior authorization for drugs and helping plan beneficiaries get the best medication treatment at the lowest price possible. It mandates that drug treatments for a medical condition progress in steps.
Which Drugs Are In Step Therapy?
Medications that may typically be included as a part of step therapy are drugs used to treat the most common medical conditions, such as:
What About Pre-existing Conditions?
If you are already taking a more expensive medication for a certain health condition at the time you join a Medicare Advantage plan with drug coverage, you may still be covered for that drug if you have already tried the lower-cost, first step drug.
Does insurance have to prove step therapy?
There is little oversight of step therapy. Generally, insurers do not have to prove the effectiveness of their step therapy policies or even take into account the side effects of their substitute drugs. NPF is actively working on a solution to step therapy.
Can insurance cover a drug that fails?
Sounds good so far. However, if your insurer believes there’s a better alternative to the medication your doctor prescribes, you are required to try that first. Only if that drug fails will the original prescription be filled. An insurer may insert several cheaper drugs and wait for them all to fail before finally agreeing to cover ...