GP Modifier According to the Centers for Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
When billing medical insurances what does a modifier GP mean?
Mar 07, 2020 · According to the Centers for Medicare and Medicaid Services, a GP modifier means that “Services [are] delivered under an outpatient physical therapy plan of care.” This means that the service or item received was a part of a preexisting plan of care for physical therapy created by Medicare doctors and physical
Does Medicare want a modifier on g0283?
Sep 30, 2017 · According to the Centers for Medicare and Medicaid Services, a GP modifier means that “Services [are] delivered under an outpatient physical therapy plan of care.” This means that the service or...
When to use the GY modifier with Medicare?
Jan 02, 2020 · According to the Centers for Medicare and Medicaid Services, a GP modifier means that “Services [are] delivered under an outpatient physical therapy plan of care.” This means that the service or item received was a part of a preexisting plan of care for physical therapy created by Medicare doctors and physical
What does a GP modifier mean?
Feb 02, 2020 · According to the Centers for Medicare and Medicaid Services, a GP modifier means that “Services [are] delivered under an outpatient physical therapy plan of care.” This means that the service or item received was a part of a preexisting plan of care for physical therapy created by Medicare doctors and physical
What does Medicare modifier GP mean?
The GP modifier indicates that a physical therapist's services have been provided. It's commonly used in inpatient and outpatient multidisciplinary settings. It's also used for functional limitation reporting (FLR), as physical therapists must report G-codes, severity modifiers, and therapy modifiers.Jul 6, 2018
Does Medicare cover GP modifier?
Medicare also requires the GP modifier for physical medicine codes; however, since Medicare does not cover physical medicine services when rendered by Doctors of Chiropractic, your billed physical medicine services would include both the GP and GY (non-covered service) modifiers.Apr 1, 2020
Is GP a payment modifier?
GP is the most appropriate for acupuncture claims, as it aligns with the therapy provider “physical therapy”. Medicare does not pay acupuncture providers for therapy; however, GP is a necessary modifier to assure a proper denial for a secondary payer to make payment.Jul 31, 2021
What are modifiers GP Go and GN?
Modifiers GN, GO, and GP refer only to services provided under plans of care for physical therapy, occupational therapy and speech-language pathology services. They should never be used with codes that are not on the list of applicable therapy services.Nov 1, 2019
Does 97140 need a modifier?
The 97140 CPT code is appended with the modifier -59 or the appropriate -X modifier.Oct 8, 2021
Does 97140 need a GP modifier?
Published by Sam Collins on April 16, 2021 Any PT now billed to Anthem will require the GP modifier. Note this modifier may be in addition to other modifiers that may be necessary such as 59 or XS on 97112, 97124, or 97140, Note the order of the modifiers is not critical but that both must appear.Apr 16, 2021
What is an HA modifier?
NOTE: The modifier is used to denote the type of service. 1. HA - Child/Adolescent Program (to be used for all services rendered to a beneficiary under the age of 21) 2. HF - Required for Substance Use Disorder Services.Jan 5, 2021
Does 97012 need a modifier?
Whether it's 97012 or 97140, by appending the 59 modifier, you will ensure that you receive reimbursement for both services.Jun 28, 2019
Can chiropractors use GP modifier?
GP is the most appropriate for chiropractic claims, as it aligns with the therapy provider “physical therapy”. This does not mean Medicare is paying chiropractic providers for therapy; however, GP is a necessary modifier to assure a proper denial for a secondary payer to make payment.Aug 9, 2021
Does 97110 need a GP modifier?
Both institutional and professional claims require Modifier GO and Modifier GP for the 97110 CPT code when billed under therapy plan of care. Modifier GO: Services delivered under an outpatient occupational therapy plan of care.
What are GN modifiers?
Definitions. Modifier GN: Services delivered under an outpatient speech language pathology plan of care. Modifier GO: Services delivered under an outpatient occupational therapy plan of care. Modifier GP: Services delivered under an outpatient physical therapy plan of care.Jun 21, 2021
What is GY modifier used for?
The GY modifier must be used when physicians, practitioners, or suppliers want to indicate that the item or service is statutorily non-covered or is not a Medicare benefit.Feb 4, 2011
What is the modifier for Medicare?
This modifier indicates that a required Advance Beneficiary Notice of Noncoverage (ABN) is on file for a service not considered medically necessary. It allows the provider to bill a secondary insurance for non-Medicare-covered services, and it also allows the provider to bill the patient directly. When you submit a claim containing this modifier, you should anticipate that Medicare will use claim readjustment reason code 50.
What is 59 modifier?
The 59 modifier signifies to Medicare that you performed a service or procedure separately and distinctly from another non-evaluation and management service provided on the same day. It’s a way to tell Medicare that payment for both services complies with the National Correct Coding Initiative. You can also use this modifier when you perform a procedure on a separate and distinct body part. (Note: There are subsets of the 59 modifier, including XE, XS, XP, and XU, which you can learn more about in this blog post .)
What is a level 2 modifier?
Level II HCPCS (Healthcare Common Procedure Coding System) modifiers: These are two-letter codes used by Medicare as well as some Medicaid and commercial plans. Here are four common PT billing modifiers, as well as some ways you can use them to bill appropriately for your organization:
Who is Meredith Castin?
Meredith Castin, PT, DPT, is the founder of The Non-Clinical PT, a career development resource designed to help physical, occupational, and speech therapy professionals leverage their degrees in non-clinical ways.
Is a physical therapy clinic a business?
The vast majority of PTs enter the field eager to help patients achieve their full functional abilities. That said, a PT clinic is still a business, and if you aren’t billing properly, it’s hard to keep your clinic afloat so you can improve the lives of the very patients you set out to help.
What is a KX modifier?
Modifier KX Use of the KX modifier indicates that the supplier has ensured coverage criteria for the DMEPOS billed is met and that documentation does exist to support the medical necessity of item. Documentation must be available upon request.
What is the GY modifier?
GY - Item or service statutorily excluded or does not meet the definition of any Medicare benefit. The GY modifier must be used when physicians, practitioners, or suppliers want to indicate that the item or service is statutorily non-covered or is not a Medicare benefit.
What is modifier GP mean?
According to the Centers for Medicare and Medicaid Services, a GP modifier means that “Services [are] delivered under an outpatient physical therapy plan of care.” This means that the service or item received was a part of a preexisting plan of care for physical therapy created by Medicare doctors and physical
What is g0 code?
Hospitals, subject to Outpatient Prospective Payment System (OPPS), report condition code G0 when multiple medical visits occurred on the same day in the same revenue center (0450, 0761, 0510) but the visits were distinct and constituted independent visits.
What is the modifier for speech therapy?
Code Modifiers Untimed CPT codes represent the "typical" time it takes to complete a specific evaluation or treatment. For significantly atypical procedures, a -22 modifier can be used to indicate that the work is substantially greater than typically required and a -52 modifier for an abbreviated procedure.
What can chiropractors bill for?
A. The most commonly billed chiropractic CPT codes are CPT Code 98940 Chiropractic manipulative treatment (CMT); Spinal, 1-2 regions, CPT Code 98941 Chiropractic manipulative treatment (CMT); Spinal, 3-4 regions, and CPT Code 98942 Chiropractic manipulative treatment (CMT); Spinal, 5 regions.
What is always therapy?
UnitedHealthcare - Always Therapy Codes. According to CMS, certain codes are “Always Therapy” services regardless of who performs them, and always require a therapy modifier (GP, GO, or GN) to indicate that they are provided under a physical therapy, occupational therapy, or speech-language pathology plan of care.
How many codes are GN modifiers required?
In addition, some “Always Therapy” codes have been identified as discipline specific. The GN modifier is specifically required for six codes, and, the GO and GP modifiers are each required on four codes, as noted below.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.
What is the KX modifier?
the individual patient is such that services are APPROPRIATELY provided in an episode that exceeds the cap. Routine use of the KX modifier for all patients with these conditions will likely show up on data analysis as aberrant and invite inquiry. Be sure that documentation is sufficiently detailed to support the use of the modifier.
What is CR in Medicare?
I. SUMMARY OF CHANGES: The purpose of this Change Request (CR) is to create edits in Original Medicare claims processing systems to ensure that certain 'always therapy' evaluation and reevaluation codes are reported with the correct modifier. It also makes several clarifications of details in Pub. 100-04, Chapter 5.
How long should a CPT be billed?
For any single timed CPT code in the same day measured in 15 minute units, providers bill a single 15-minute unit for treatment greater than or equal to 8 minutes through and including 22 minutes. If the duration of a single modality or procedure in a day is greater than or equal to 23 minutes through and including 37 minutes, then 2 units should be billed. Time intervals for 1 through 8 units are as follows:
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add a KX modifier to the therapy HCPCS code subject to the cap limits. The KX modifier shall not be added to any line of service that is not a medically necessary service; this applies to services that, according to a local coverage determination by the contractor, are not medically necessary services.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC statement of Work. The contractor is not obliged to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
When did CMS 1450 become effective?
Effective with claims submitted on or after April 1, 1998, providers billing on Form CMS-1450 were required to report the number of units for outpatient rehabilitation services based on the procedure or service, e.g., based on the HCPCS code reported instead of the revenue code. This was already in effect for billing on the Form CMS-1500, and CORFs were required to report their full range of CORF services on the Form CMS-1450. These unit-reporting requirements continue with the standards required for electronically submitting health care claims under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) - the currently adopted version of the ASC X12 837 transaction standards and implementation guides. The Administrative Simplification Compliance Act mandates that claims be sent to Medicare electronically unless certain exceptions are met.
Can a clinic use the exception process?
Clinicians may utilize the process for exception for any diagnosis or condition for which they can justify services exceeding the cap. Regardless of the diagnosis or condition, the patient must also meet other requirements for coverage.
What are modifiers in Medicare?
Modifiers are used to identify therapy services whether or not financial limitations are in effect . When limitations are in effect, the CWF tracks the financial limitation based on the presence of therapy modifiers. Providers/suppliers must continue to report one of these modifiers for any therapy code on the list of applicable therapy codes except as noted in §20 of this chapter. Consult §20 for the list of codes to which modifiers must be applied. These modifiers do not allow a provider to deliver services that they are not qualified and recognized by Medicare to perform.
What is modifier GN?
Submit modifier GN to indicate that the services were delivered under an outpatient speech language pathology plan of care .#N#If additional modifiers are required with the service, modifier GN must be submitted in the first or second modifier position.#N#Exception: Claims from physicians (all specialty codes) and non-physician practitioners, including specialty codes “50, 89, and 97”, may be processed without therapy modifiers for sometimes only therapy codes.#N#If specialty codes “65” and “67” are on the claim and an applicable HCPCS code is without one of the therapy modifiers (GN, GO, GP), the claim will be returned as unprocessable.
What is the code for PT?
they are considered therapy services and must meet the other conditions for physical and occupational therapy. The PT or OT would use the appropriate HCPCS/CPT code (s) in the 97000 – 97799 series and the corresponding therapy modifier, GP or GO, must be used.
Types of Physical Therapy Billing Modifiers
Cpt Modifiers
- 59 modifier
The 59 modifier signifies to Medicare that you performed a service or procedure separately and distinctly from another non-evaluation and management service provided on the same day. It’s a way to tell Medicare that payment for both services complies with the National Correct Coding I…
Level II HCPCS (Healthcare Common Procedure Coding System) Modifiers
- GP modifier
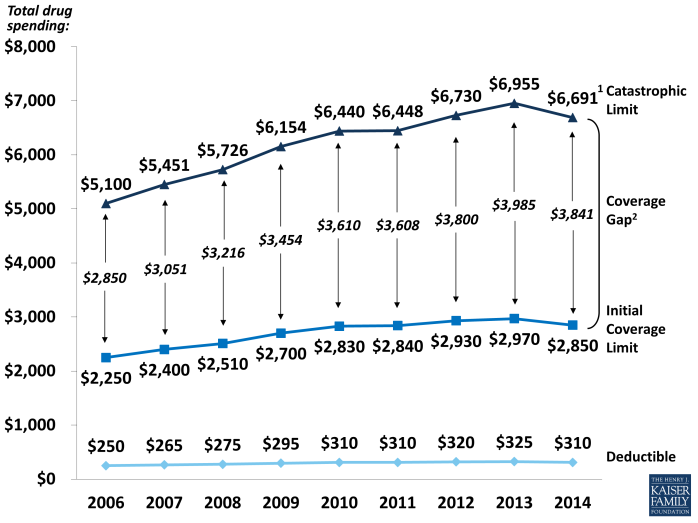
The GP modifier indicates that a physical therapist’s services have been provided. It’s commonly used in inpatient and outpatient multidisciplinary settings. It’s also used for functional limitation reporting (FLR), as physical therapists must reportG-codes, severity modifiers, and therapy modi… - KX modifier
This modifier is used for services providedafter a patient exceeds Medicare’s $2,010 threshold. Be sure that you only use this modifier when you know that continued treatment is medically necessaryand must be performed by a therapist—and that you justify that necessity with approp…
Conclusion
- We’re often challenged by the level of payment for our services. That’s why it’s so important to remember that modifiers exist to help us bill appropriately for the time we spend with patients—and they help ensure we receive payment for the services we provide. That said, as compliance expert Tom Ambury has pointed out, we never want to use a billing modifier on a cla…