What is the difference between Medicare amount and Medicare approved amount?
Amount Provider Charged: This is your provider's fee for this service. Medicare-Approved Amount: This is the amount a provider can be paid for a Medicare service. It may be less than the actual amount the provider charged.Your provider has agreed to accept this amount as full payment for covered services.
What does Service approved mean on a Medicare card?
Service Approved?: This column tells you if Medicare covered the home health service. Amount Provider Charged: This is your provider's fee for this service. Medicare-Approved Amount: This is the amount a provider can be paid for a Medicare service.
Can I be charged more than the Medicare-approved amount?
In some cases you may be charged more than the Medicare-approved amount. Original Medicare has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). A doctor, dentist, hospital or other practitioner who is not contracted with that particular health plan.
Do you still owe 20 percent of Medicare approved costs?
However, under Part B, you still owe 20 percent of the Medicare-approved amount for all covered items and services. You can save money on your Medicare approved costs by asking your doctor the following questions before you receive services:

What does the Medicare-approved amount mean?
The approved amount, also known as the Medicare-approved amount, is the fee that Medicare sets as how much a provider or supplier should be paid for a particular service or item. Original Medicare also calls this assignment. See also: Take Assignment, Participating Provider, and Non-Participating Provider.
Can a doctor charge more than the Medicare-approved amount?
A doctor who does not accept assignment can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive. A doctor who has opted out of Medicare cannot bill Medicare for services you receive and is not bound by Medicare's limitations on charges.
What percentage of the allowed amount is paid by Medicare for medical services?
In Original Medicare, the highest amount of money you can be charged for a covered service by doctors and other health care suppliers who don't accept assignment. The limiting charge is 15% over Medicare's approved amount. The limiting charge only applies to certain services and doesn't apply to supplies or equipment.
What is the difference between Medicare fee-for-service and Medicare managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
Why is Medicare-approved amount different than Medicare paid?
Amount Provider Charged: This is your provider's fee for this service. Medicare-Approved Amount: This is the amount a provider can be paid for a Medicare service. It may be less than the actual amount the provider charged. Your provider has agreed to accept this amount as full payment for covered services.
Why does Medicare pay less than the Medicare-approved amount?
Because you have met your deductible for the year, you will split the Medicare-approved amount with Medicare in order to pay your doctor for the appointment. Typically, you will pay 20 percent of the Medicare-approved amount, and Medicare will pay the remaining 80 percent.
What is the difference between allowed amount and paid amount?
If the billed amount is $100.00 and the insurance allows $80.00 then the allowed amount is $80.00 and the balance $20.00 is the write-off amount. Paid amount: It is the amount which the insurance originally pays to the claim. It is the balance of allowed amount – Co-pay / Co-insurance – deductible.
Why there is a difference between the amount billed allowed and paid?
The allowed amount is the maximum amount a plan will pay for a covered health care service. May also be called “eligible expense,” “payment allowance,” or “negotiated rate.” If a provider charges more than the plan's allowed amount, beneficiaries may have to pay the difference, (balance billing).
What is the difference between allowable amount and insurance payment?
For example, if the health insurance or plan's allowed amount for an office visit is $100 and you've met your deductible, your coinsurance payment of 20 percent would be $20. The health insurance or plan pays the rest of the allowed amount.
What is the main difference between traditional and managed fee-for-service reimbursement?
The main difference between a managed health care plan and a traditional fee-for-service health insurance plan is that managed health care plans are dependent on a network of key players, including health care providers, doctors, and facilities that establish a contract with an insurance provider to offer plans to ...
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What is managed fee-for-service?
Under the FFS model, the Centers for Medicare & Medicaid Services (CMS) and a state enter into an agreement through which the state would be eligible to benefit from savings resulting from initiatives that improve quality and reduce costs for both Medicare and Medicaid.
What is Medicare approved amount?
The Medicare-approved amount is the amount that Medicare pays your provider for your medical services. Since Medicare Part A has its own pricing structure in place, this approved amount generally refers to most Medicare Part B services. In this article, we’ll explore what the Medicare-approved amount means and it factors into what you’ll pay ...
What are the services covered by Medicare?
No matter what type of Medicare plan you enroll in, you can use Medicare’s coverage tool to find out if your plan covers a specific service, test, or item. Here are some of the most common Medicare-approved services: 1 mammograms 2 chemotherapy 3 cardiovascular screenings 4 bariatric surgery 5 physical therapy 6 durable medical equipment
What is a non-participating provider?
Nonparticipating provider. A nonparticipating provider accepts assignment for some Medicare services but not all. Nonparticipating providers may not offer discounts on services the way participating providers do. Even if the provider bills Medicare later for your covered services, you may still owe the full amount upfront.
How much is Medicare Part A deductible?
If you have original Medicare, you will owe the Medicare Part A deductible of $1,484 per benefit period and the Medicare Part B deductible of $203 per year. If you have Medicare Advantage (Part C), you may have an in-network deductible, out-of-network deductible, and drug plan deductible, depending on your plan.
What percentage of Medicare deductible is paid?
After you have met your Part B deductible, Medicare will pay its portion of the approved amount. However, under Part B, you still owe 20 percent of the Medicare-approved amount for all covered items and services.
What happens if a provider accepts assignment?
If they are a nonparticipating provider, they may still accept assignment for certain services. However, they can charge you up to an additional 15 percent of the Medicare-approved amount for these services.
What is Medicare Advantage?
Medicare Part B covers you for outpatient medical services. Medicare Advantage covers services provided by Medicare parts A and B, as well as: prescription drugs. dental.
What is the limiting charge for Medicare?
In Original Medicare, the highest amount of money you can be charged for a covered service by doctors and other health care suppliers who do not accept assignment. The limiting charge is 15% over Medicare’s approved amount. The limiting charge only applies to certain services and does not apply to supplies or equipment.
What percentage of Medicare is paid after deductible?
The amount you may be required to pay for services after you pay any plan deductibles. In Original Medicare, this is a percentage (like 20%) of the Medicare approved amount. You have to pay this amount after you pay the deductible for Part A and/or Part B.
What is the gap in Medicare coverage?
Also known as the “donut hole,” this is a gap in coverage that occurs when someone with Medicare goes beyond the initial prescription drug coverage limit. When this happens, the person is responsible for more of the cost of prescription drugs until their expenses reach the catastrophic coverage threshold.
What is copayment in Medicare?
A copayment is usually a set amount you pay. For example, this could be $10 or $20 for a doctor’s visit or prescription.
How often does Medicare pay deductibles?
For example, in Original Medicare, you pay a new deductible for each benefit period for Part A, and each year for Part B. These amounts can change every year.
How many days does Medicare pay for a hospital stay?
In Original Medicare, a total of 60 extra days that Medicare will pay for when you are in a hospital more than 90 days during a benefit period. Once these 60 reserve days are used, you do not get any more extra days during your lifetime. For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance.
What is hospice care?
Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional and spiritual needs of the patient. Hospice also provides support to the patient’s family or caregiver as well. Hospice care is covered under Medicare Part A (Hospital Insurance).
What does Lamoureux think about healthcare?
Lamoureux thinks the information actually gives consumers some negotiating power when it comes to health care costs, something they’ve never had before. He says the system of hospital pricing and reimbursement is badly broken and this step toward more transparency is long overdue.
Is a hospital bill a part of the overall cost of health care?
But a hospital bill is only one part of the overall health care cost picture. “That’s kind of like a rack rate in the hotel room,” says Karen Perdue, president of the Alaska State Hospital & Nursing Home Association. “Most people aren’t paying that one rate in the hotel.
Does private insurance pay more than Medicare?
Private insurance usually pays more than Medicare, but negotiates the amount. The system doesn’t make much sense, but Davis says more transparency will help: “For there to be pressure on pricing on the consumer side, the consumer has to understand what it’s going to cost them. And so, I think this is a good report.
How often do Medicare summary notices come out?
Medicare Summary Notices are sent out four times a year — once a quarter — but you don't have to wait for your notice to arrive in the mail. You can also check your account online at MyMedicare.gov. Claims typically appear on your electronic statement 24 hours after processing. 6.
How to contact Medicare if you have questions?
If the doctor's office cannot resolve your concerns, contact Medicare at 1-800-MEDICARE (1-800-633-4227) . 12. Service Provided.
What is the number to call for Medicare fraud?
If you think a provider or a business is involved in fraud, call us at 1-800-MEDICARE (1-800-633-4227) . Some examples of fraud include offers for free medical services, or billing you for Medicare services you didn't get. If we determine that your tip led to uncovering fraud, you may qualify for a reward.
Is Medicare summary notice a bill?
Your Medicare Summary Notice is not a bill. It is a statement you should review for accuracy and keep for your personal records. Very important: Never send a health care provider payment for charges listed on a Medicare Summary Notice until you've received a bill for the service directly from the provider.
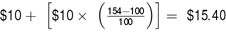
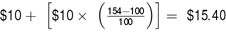
How much does Medicare pay for Part B?
Medicare will pay their 80 percent (of the Medicare-approved amount), assuming the Part B deductible has already been met, so in this case, $80. The patient then pays the remaining $20 of the approved amount, but then also the $15 in “excess” charges, for a total of $35.
Does Medicare Part B cover excess charges?
However, several Medigap plans don’t cover Medicare Part B excess charges. It’s important, therefore, to not only verify with your physician (s) that they accept assignment, but also, if you have supplemental coverage, to understand what is covered by your plan.