When can you sign up for Medicare supplement insurance?
Dec 22, 2020 · Medicare Supplement Insurance (Medigap) has a six-month open enrollment period (OEP). Your open enrollment period begins when you are both: 65 years old and. Enrolled in Medicare Part B. Unlike the Medicare OEP that happens once every year, you have only one Medigap OEP. If you get Medicare Part B before you turn 65, your Medigap OEP starts the first …
When is Medicare supplement open enrollment?
Dec 16, 2021 · Your Medicare Supplement Open Enrollment Period begins the first day of the month your Part B goes into effect. If you delay your Part B, your enrollment window for Medigap will start the same day as your Medicare Part B. You’re one-time open enrollment window will last six months. Most people will only have one OEP in their lifetime.
Is there open enrollment for Medicare supplements?
May 06, 2021 · Medicare Supplement Open Enrollment Period (OEP): this 6-month period starts the first month that you’re both age 65 or over, and enrolled in Medicare Part B. Your Medicare Supplement OEP is when you can buy a Medicare Supplement insurance plan without risk of being turned down or charged more if you have a health condition.
Is Medicare supplement open enrollment?
Aug 06, 2021 · Your Medicare Supplement Open Enrollment Period is unique to you and begins the first day of the month your Medicare Part B is effective. This window lasts for six months and is a once-in-a-lifetime opportunity to enroll in any Medicare Supplement plan without the need to answer health questions and undergo the medical underwriting process.
Is there a waiting period for Medicare supplement plans?
What is the Medicare Supplement Waiting Period? For up to six months after your Medicare Supplement plan begins, your new plan can choose not to cover its portion of payments for preexisting conditions that were treated or diagnosed within six months of the start of the policy.
What is the open enrollment period for Medicare Supplements?
Under federal law, you have a six-month open enrollment period that begins the month you are 65 or older and enrolled in Medicare Part B. During your open enrollment period, Medigap companies must sell you a policy at the best available rate regardless of your health status, and they cannot deny you coverage.
Can I change Medicare supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
When can I change my Medicare supplement plan for 2022?
You can change your Medicare Supplement Insurance (Medigap) plan anytime, but there are a few things you should know before you do so. You can enroll in a Medigap plan during your Medigap Open Enrollment Period.Nov 22, 2021
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
What are the four prescription drug coverage stages?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.Oct 1, 2021
Should I switch from Plan F to Plan G?
Two Reasons to switch from Plan F to G Plan G is often considerably less expensive than Plan F. You can often save $50 a month moving from F to G. Even though you will have to pay the one time $233 for the Part B deductible on Medigap G, the monthly savings will be worth it in the long run.Sep 5, 2019
Which states allow you to change Medicare Supplement plans without underwriting?
In some states, there are rules that allow you to change Medicare supplement plans without underwriting. This includes California, Washington, Oregon, Missouri and a couple others. Call us for details on when you can change your plan in that state to take advantage of the “no underwriting” rules.
Can you switch back and forth between Medicare and Medicare Advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
When can I switch from Medigap to Medicare Advantage?
The best (and often only time) to switch from Medigap to Medicare Advantage is during the Open Enrollment Annual Election Period which runs from Oct 15th to Dec 7th. To switch during this time, you would enroll in a MA plan which can only start on Jan 1st of the following year.Jul 8, 2015
Can you have two Medicare supplement plans?
En español | By law, Medigap insurers aren't allowed to sell more than one Medigap plan to the same person.
Can you switch from Plan N to Plan G without underwriting?
You can change Medigap carriers, while keeping the same level of coverage, during the months surrounding your Medigap anniversary. For example, you can switch from a Plan G to a Plan G without underwriting, but not from a Plan G to a Plan N.Jan 30, 2021
Medicare Enrollment Periods When You’Re New to Medicare
When you first become eligible for Medicare, you’re enrolling in Original Medicare (Part A and Part B), the government-run health-care program for...
Medicare Enrollment For Original Medicare
When you turn 65, you will automatically be enrolled in Medicare Part A and Part B (Original Medicare) if you are receiving retirement benefits fro...
Medicare Enrollment Periods For Original Medicare
If you need to manually enroll in Medicare Part A and/or Part B, you can sign up during the following times: 1. Initial Enrollment Period (IEP) — W...
Medicare Enrollment If You’Re Disabled, Have ALS, Or Have ESRD
You can also qualify for Medicare before age 65 in certain situations. If you are under age 65 and receiving Social Security or certain Railroad Re...
Medicare Enrollment For Medicare Plans
When it comes to certain types of Medicare coverage, such as Medicare Advantage (Part C) or Medicare prescription drug coverage, Medicare enrollmen...
Enrolled in Medicare: Making Changes to Your Medicare Coverage
Once you’re enrolled in Original Medicare or a Medicare Advantage plan, you can generally only make changes to your coverage during certain times o...
Medicare Enrollment If You Have A Special Situation
Once the Annual Election Period has passed, you’re much more limited in the types of changes you can make to your Medicare coverage. However, in ce...
When is the enrollment period for Medicare?
Drop your Medicare Advantage plan and return to Original Medicare. Drop your stand-alone Medicare prescription drug plan. Annual Enrollment Period: October 15 – December 7 each year.
How long does Medicare enrollment last?
You’re eligible for Medicare because you turn age 65. Initial Enrollment Period: the 7-month period that begins 3 months before your birthday month, includes your birthday month, and ends 3 months after your birthday month.
How to switch Medicare Advantage plans?
Medicare enrollment: switching Medicare Advantage plans 1 Change from one Medicare Advantage plan to another. 2 Disenroll from your Medicare Advantage plan. 3 Pick up a stand-alone Medicare Part D prescription drug plan. You can only do this during this period if you disenroll from a Medicare Advantage plan.
What is Medicare Part C?
Medicare Part C is Medicare Advantage. Medicare Part D is prescription drug coverage. You want to do any of these…. Medicare Advantage and Medicare prescription drug plan enrollment period. Sign up for a Medicare Advantage plan. Switch from one Medicare Advantage plan to another.
Can you change your Medicare coverage?
When you enroll in Medicare, you have a choice of how you receive your Medicare benefits. You can also make changes in your Medicare coverage. It’s important to understand the Medicare enrollment periods, when they happen, and how you can use them.
What happens if you miss your Medigap open enrollment period?
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
How long does Medicare open enrollment last?
Applying outside your open enrollment window can result in higher premiums, as well as restrict your coverage options. This window only lasts for six months for each new beneficiary, unless you delay enrollment into Part B due to having other creditable coverage.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
What is Medicare Supplement Open Enrollment Period?
What is Medicare Supplement Open Enrollment? Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions.
Which states have open enrollment?
Some states have unique open enrollment rules, like Connecticut and California. In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries.
Do you have to be 65 to get a Medigap plan?
Many states are not required to offer all supplement plans to those under 65. Most states only offer Plan A to those under 65. If they wait to enroll in a Medigap plan when they turn 65 during their second Medigap OEP, they’ll be able to choose from all the programs available to them in their state.
How long does Medicare Advantage last?
Your Special Enrollment Period starts 60 days before and lasts for 63 days after your previous coverage ends.
What is a select Medicare plan?
A Medicare SELECT policy is a Medigap plan with provider networks that is combined with Original Medicare. 1 If you experience issues with your Medicare SELECT policy, then you may qualify for a Medigap Special Enrollment Period.
How long does Medigap last?
You can purchase a new plan within a reasonable amount of time after learning about the rule violation. Your Special Enrollment Period lasts for 63 days after your previous coverage ends.
Why did Medicare cancel my plan?
You canceled your Medicare Advantage plan because it violated its contract with you. You canceled your enrollment in a Medicare supplement plan and enrolled in a Medicare Advantage plan for the first time. Then, you canceled the Medicare Advantage plan within the first 12 months (applies to Plan N as well).
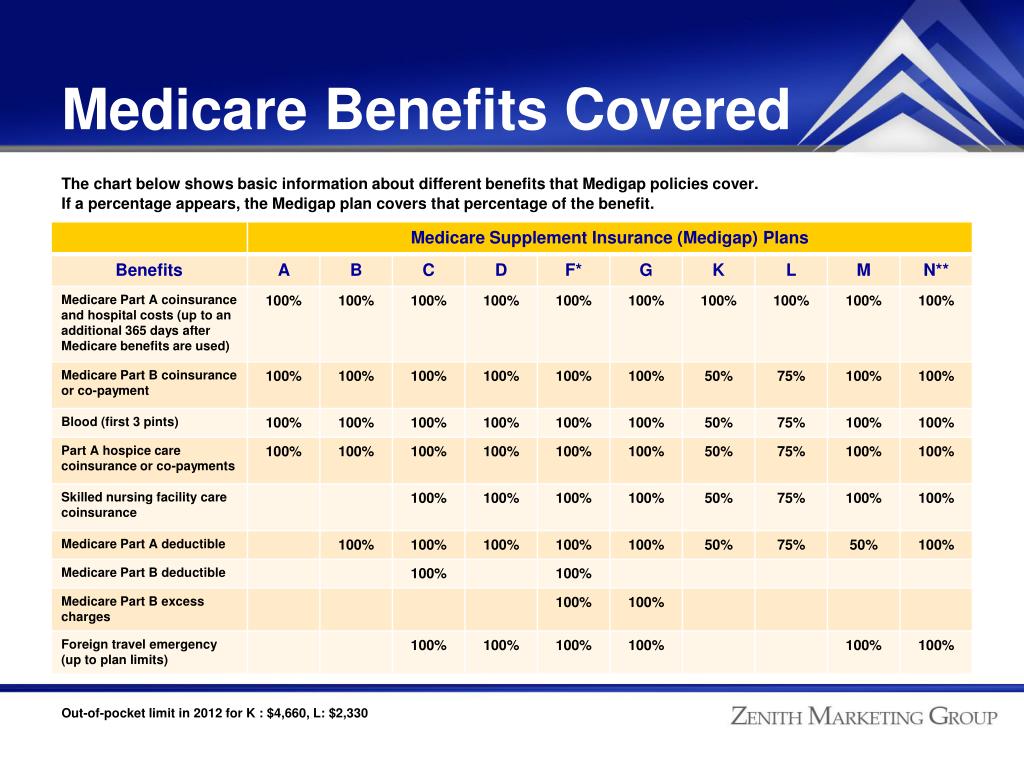
What is the Medicare deductible?
The Medicare deductibles, coinsurance and copays listed are based on the 2019 numbers approved by the Centers for Medicare and Medicaid Services. You can go to any hospital, doctor or other health care provider in the U.S. or its territories that accepts Medicare.
Is Blue Cross Medicare endorsed by the government?
This is a solicitation of insurance. We may contact you about buying insurance. Blue Cross Medicare Supplement plans aren't connected with or endorsed by the U.S. government or the federal Medicare program. If you're currently enrolled in Plan A or Plan C, you can stay with your plan as long as you pay your premium.
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
How to change Medicare Advantage plan?
☐ I currently have a Medicare Advantage plan (Part C) with built-in drug coverage. 1 Switch from your current Medicare Advantage plan to another Medicare Advantage plan with or without built-in drug coverage. 2 Drop your Medicare Advantage plan and go back to Original Medicare. 3 Join a stand-alone Medicare prescription drug plan if you go back to Original Medicare or if you switch to a Medicare Advantage plan that does not include drug coverage. 4 Drop Medicare prescription drug coverage completely. Note that you may be charged a penalty if you decide you want drug coverage again later. 5 Make no changes and your current coverage will renew as is.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. .
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
