- Medicare part A pays for the entire hospital stay plus any related outpatient charges for the 3 days prior to the inpatient order being written (i.e., the ER visit)
- The patient has no hospital co-pay
- Medicare part A pays for the SNF
What is the Medicare 3 day hospital stay rule?
meet the 3-day rule 3-DAY PRIOR HOSPITALIZATION BEFORE SNF ADMISSION Medicare beneficiaries meet the 3-day rule by staying 3 consecutive days in one or more hospitals as an inpatient. Hospitals count the admission day but not the discharge day. Time spent in the ER or in outpatient observation prior to admission does not count toward the 3-day rule. 3-DAY RULE WAIVER
What is Medicare 3 midnight rule?
- Waiver for Medicare Ground Ambulance Services Treatment in Place (PDF) (5/5/21)
- COVID-19 Emergency Declaration Blanket Waivers & Flexibilities for Health Care Providers (PDF) UPDATED (5/24/21)
- Blanket waivers of Section 1877 (g) of the Social Security Act (3/30/20)
What happens when you run out of Medicare days?
- You can contact Medicare directly at 800-MEDICARE (800-633-4227).
- Get help from trained, impartial counselors through your local State Health Insurance Assistance Program (SHIP).
- Look for programs that can help you pay Medicare costs through state Medicare savings programs.
What is the Medicare 72-hour rule?
72 Hour Rule and Medicare 72 Hour Rule and Medicare. The 72 hour rule is part of the Medicare Prospective Payment System (PPS). ... Recordkeeping. To make sure bills are processed (and paid) properly, the hospital must keep proper records. ... Staying Compliant. As you can see, it's very easy to mistakenly double-bill Medicare. ...
What is the 72 hour rule for Medicare?
The 72 hour rule is part of the Medicare Prospective Payment System (PPS). The rule states that any outpatient diagnostic or other medical services performed within 72 hours prior to being admitted to the hospital must be bundled into one bill.
Will Medicare pay for hospital stay less than 3 days?
Since March 2020, CMS has waived the three-day requirement during the health emergency and coronavirus pandemic. [15] Congress needs to repeal the 1965 statutory provision that limits Medicare Part A coverage in a SNF to beneficiaries who have been hospitalized as inpatients for at least three consecutive days.
How many days will Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
What is the two midnight rule for Medicare?
The Two-Midnight rule, adopted in October 2013 by the Centers for Medicare and Medicaid Services, states that more highly reimbursed inpatient payment is appropriate if care is expected to last at least two midnights; otherwise, observation stays should be used.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Can Medicare kick you out of the hospital?
Medicare covers 90 days of hospitalization per illness (plus a 60-day "lifetime reserve"). However, if you are admitted to a hospital as a Medicare patient, the hospital may try to discharge you before you are ready. While the hospital can't force you to leave, it can begin charging you for services.
What happens when you run out of Medicare days?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
How are hospital days counted?
Length of stay (LOS) is the duration of a single episode of hospitalization. Inpatient days are calculated by subtracting day of admission from day of discharge.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
What does code 44 mean in a hospital?
A Condition Code 44 is a billing code used when it is determined that a traditional Medicare patient does not meet medical necessity for an inpatient admission.
What surgeries are not covered by Medicare?
However, services such as elective cosmetic surgery, some dental procedures and laser eye surgery are not listed on the MBS....What Medicare doesn't coverAmbulance services.Most dental services (unless deemed medically necessary)Optometry (glasses, LASIK, etc)Audiology (hearing aids)Physiotherapy.Cosmetic Surgery.
What does condition code 64 mean?
Enter condition code 64 to indicate that the claim is not a "clean" claim, and therefore, not subject to the mandated claims processing timeliness standard.
What Is SNF Care?
SNF care takes place after you are hospitalized. These facilities provide a high level of patient supervision by qualified healthcare professionals.
What Are the Requirements for SNF Care?
You cannot get SNF care unless a doctor has determined that you need it because your condition warrants skilled nursing staff supervision.
Are there exceptions?
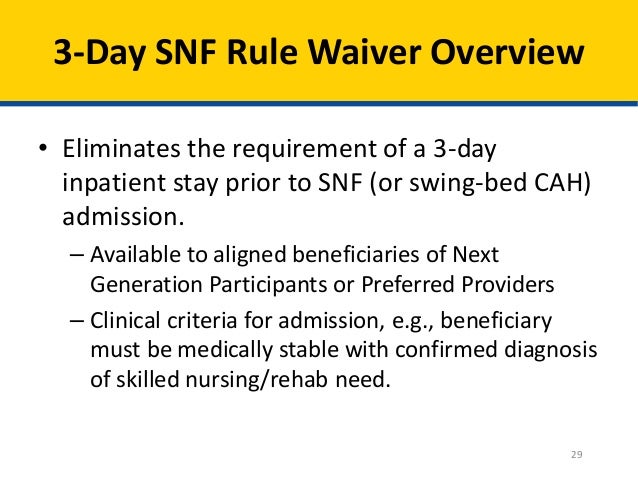
Yes, there are exceptions to the 3-day rule but they are very specific and are known as the 3-day rule waiver. Certain models that fall under the Shared Savings Program (SSP) and the Center for Medicare and Medicaid Innovation Models, offer SNF services without a prior 3-day admission to hospital.
Communication is Important
Most importantly, as a Medicare beneficiary, you should be aware of all the small print relating to your medical plan. Make sure to get in contact with your Medicare representative to discuss anything that is unclear.
How many days prior to SNF for Medicare?
However, for SNF coverage decisions, Medicare will not count the 3 days prior to the inpatient order toward the 3 inpatient days that Medicare requires in order for Medicare to pay for SNF charges. Medicare’s coverage rules are byzantine and indecipherable for the average patient.
How long is an inpatient in Medicare?
Medicare considers a patient to be in inpatient status if that patient is anticipated to need to be in the hospital for 2 midnights and in observation status if the patient is anticipated to be in the hospital for less than 2 midnights. Observation status was originally intended to be used to observe the patient to determine whether ...
How long does it take for Medicare to pay for SNF?
The 3-day rule is Medicare’s requirement that a patient has to be admitted to the hospital for at least 3 days in order for Medicare to cover the cost of a SNF after the hospitalization. If the patient is admitted for less than 3 days, then the patient pays the cost of the SNF and Medicare pays nothing. So, if this patient was in the hospital ...
How long does it take for a surgeon to change an order to inpatient?
The surgeon writes an order for the patient to be in observation status at the time of the surgery. After 2 days , the surgeon changes the order to inpatient status. The patient spends 4 nights in the hospital but still need more rehabilitation so the patient is discharged to a SNF.
How long do you have to stay in the hospital after a heart surgery?
The patient has difficult-to-control diabetes, heart failure, sleep apnea, and kidney failure so the surgeon anticipates that the patient will need to stay in the hospital for more than 2 midnights after the surgery to care for the medical conditions.
How long was a woman in the hospital after knee replacement?
She was in the hospital for 4 days after her surgery but was very slow to recover and was determined to be unsafe for discharge home without additional rehabilitation so she was discharged to a SNF (subacute nursing facility). She spent a week getting rehab at the SNF and then returned home only to find that she had a bill for the entire stay the nursing facility; Medicare covered none of it. She paid her bills but in doing so, wiped out most of her savings.
Is observation covered by Medicare?
However, if a patient is in observation status, then the hospital stay is not covered by Medicare part A but instead is covered by Medicare part B which requires the patient to pay a 20% co-pay for all of the charges plus pay for any medications administered during the hospitalization.
