The Medicare claims appeal process has five levels:
- Redetermination. The first step in the Medicare appeals process is a review of the initial determination made by the company that handles Medicare claims. ...
- Reconsideration. ...
- Administrative law judge (ALJ) hearing. ...
- Medicare Appeals Council review. ...
- Judicial review in U.S. ...
How does the Medicare appeals process work?
To increase your chance of success, you may want to try the following tips:
- Read denial letters carefully. ...
- Ask your healthcare providers for help preparing your appeal. ...
- If you need help, consider appointing a representative. ...
- Know that you can hire legal representation. ...
- If you are mailing documents, send them via certified mail. ...
- Never send Medicare your only copy of a document. ...
- Keep a record of all interactions. ...
What are the levels of Medicare Appeals?
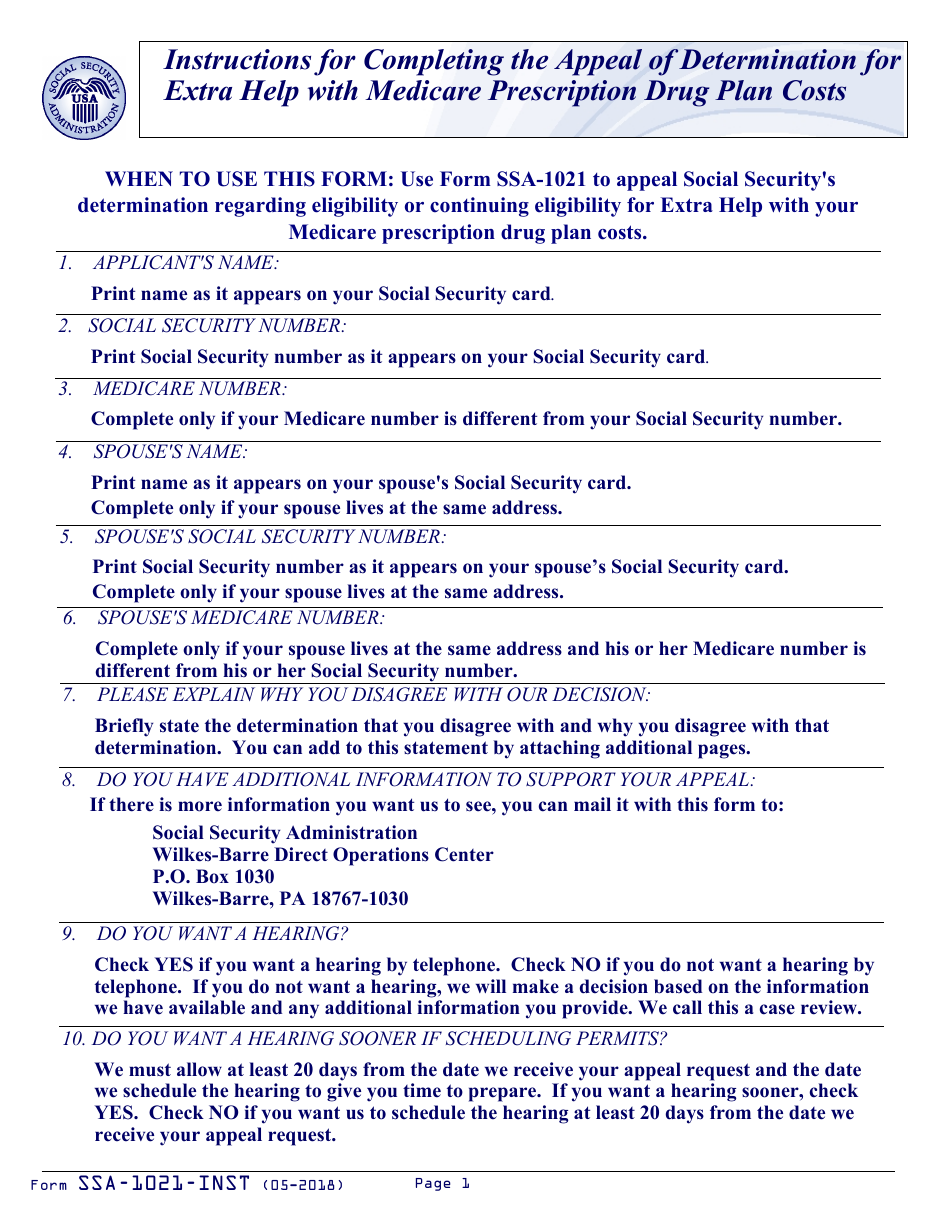
Your signature or your representative’s signature.
- Your name and Medicare health insurance claim number
- The specific item (s) or service (s) that prompted your reconsideration. ...
- The name of the company that made the redetermination (the company that handled the Medicare claim in Level 1). ...
- A detailed explanation of why you disagree with the decision.
- Your signature or your representative’s signature.
How to properly compose Medicare appeal letter and its sample?
Sample Appeal Letter A. Please accept this letter as [patient's name] appeal to [insurance company name] decision to deny coverage for [state the name of the specific procedure denied]. It is my understanding based on your letter of denial dated [insert date] that this procedure has been denied because: [quote the specific reason for the denial ...
What is second level Medicare appeal?
- Your name, address, and Medicare health insurance claim number. ...
- The appeal number included on the Level 2 reconsideration notice, if any
- A list of dates for the items or services you’re appealing
- A detailed written explanation of why you disagree with the Level 2 decision
- Any additional information you feel might help your case. ...
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What are the steps taken when appealing a Medicare claim?
Left navigationFile a complaint (grievance)File a claim.Check the status of a claim.File an appeal. Appeals if you have a Medicare health plan. Get help filing an appeal.Your right to a fast appeal.Authorization to Disclose Personal Health Information.
What are the chances of winning a Medicare appeal?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is the first step in the Medicare appeals process?
If you disagree with the Medicare contractor's decision on your claim, you have the right to file an appeal. The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
What is appeal process?
Appeals are decided by panels of three judges working together. The appellant presents legal arguments to the panel, in writing, in a document called a "brief." In the brief, the appellant tries to persuade the judges that the trial court made an error, and that its decision should be reversed.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
What are the six levels of appeals for Medicare Advantage plans?
Appealing Medicare DecisionsLevel 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
How long does a Medicare discharge appeal take?
You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN. Medicare Advantage plans typically decide within 14 days. Prescription plans usually respond within 72 hours.
Can you be denied Medicare coverage?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What are the different types of Medicare appeals?
Original Medicare (Fee-for-service) AppealsOriginal Medicare (Fee-for-service) Appeals.Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Third Level of Appeal: Decision by Office of Medicare Hearings and Appeals (OMHA) Fourth Level of Appeal: Review by the Medicare Appeals Council.
Why would Medicare deny a claim?
A claim that is denied contains information that was complete and valid enough to process the claim but was not paid or applied to the beneficiary's deductible and coinsurance because of Medicare policies or issues with the information that was provided.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How to ask for a prescription drug coverage determination?
To ask for a coverage determination or exception, you can do one of these: Send a completed "Model Coverage Determination Request" form. Write your plan a letter.
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How many levels of appeals are there for Medicare?
There are five levels in the Medicare appeals process. 2 If at any time your appeal is approved by Medicare, the process ends at the level you are currently on. If a denial is upheld, you will have to decide whether or not to proceed to the next level.
What is level 5 appeal?
Level 5: Judicial review by a federal district court. You are only eligible for a Level 5 appeal if your case meets a minimum financial requirement, $1,670 of denied services in 2020. 2 If necessary, you can combine claims to meet this dollar amount. A decision by a federal district court is final.
How long does it take to clear Medicare backlog?
There is now a court order to clear the backlog by the end of 2022. 4 If the ALJ does not make their determination in a reasonable amount of time, you can request to proceed directly to Level 4. If the ALJ denies your appeal, you have 60 days to request review with a Medicare Appeals Council at Level 4.
What is Medicare summary notice?
The Medicare Summary Notice (MSN) is a form you will receive quarterly (every three months) that lists all the Medicare services you received during that time, the amount that Medicare paid, and any non-covered charges, among other information. 1 Please note that the MSN is sent to people on Original Medicare ( Part A and Part B ), not to people on Medicare Advantage. It is not a bill and may be sent to you from the company assigned to process your Medicare claim, not from Medicare itself.
How long does it take to get a level 1 Medicare claim?
The first step is to complete a Redetermination Request Form. You will get a Level 1 decision within 60 days. It could take an additional 14 days, however, if you submit additional information after the case was filed.
What to do if you don't win a level 3 appeal?
If you did not succeed in a Level 3 appeal, you can complete a Request for Review of an Administrative Law Judge (ALJ) Medicare Decision/Dismissal Form or send a written request to the Medicare Appeals Council to have them review the ALJ's decision.
What is the level of Medicare review?
Level 1: Reconsideration by your health plan. Level 2: Review by an Independent Review Entity (IRE) Level 3: Hearing before an Administrative Law Judge (ALJ) Level 4: Review by the Medicare Appeals Council (Appeals Council) Level 5: Judicial review by a federal district court.
Overview Of Medicare Appeals Process
If you disagree with a decision by Medicare on whether to provide coverage or payment for a certain medical service, then you have certain appeal rights. You can make an appeal request for Medicare to reconsider their decision. There are five levels to the appeals process although they may not all be necessary for your specific appeal.
Five Levels Of Medicare Appeals
Similar to the court system, there are different levels of appeals in Medicare. If you are unsuccessful at one level, then you can appeal to the next level. If you go all the way to the top, you could end up in Federal court. In practice though, very few appeals make it that far. Here are the different levels and what you need to know about each.
How Long Do You Have To File An Appeal?
The answer depends on which stage of the process you are currently in. Initially, you should look at your Medicare Summary Notice (MSN) for the claim that you wish to appeal. It will have a date printed on it by which you must file your first level appeal. Generally, this date is 120 days from the date you received the initial determination.
Tips For Winning Your Appeal
We know that you want to win your appeal or else you would not be filing it in the first place. There are some things that you should keep in mind when filing appeals with the Centers for Medicare & Medicaid Services. If you keep these tips in mind, it can greatly increase your odds of being successful.
The Bottom Line
If you disagree with a decision by Medicare whether to cover a service or how much to pay, then you have a right to file an appeal. It could be nearly any decision that they make from whether to pay for care in a skilled nursing facility to whether a prescription drug is medically necessary.
How successful are Medicare appeals?
Medicare appeals are actually quite successful. In fact, data has shown that roughly 80% to 90% of appeals are won by the claimant who is appealing the decision. If you do not win your appeal at the first or second level, do not give up. Keep going as far in the appeals process as possible to increase your odds of ultimately winning your appeal.
How long does Medicare have to respond to an appeal?
It depends on which stage of the appeals process you are on. For Level 1, the general timeframe to respond to the appeal is 60 days. At level 2, the decision is again made within 60 days. If a decision cannot be reached in this timeframe, you will still receive notice of your rights in the appeals process.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
What is a fast appeal?
If waiting for a decision would affect a person’s health, they can ask for a fast appeal. An example of the need for a fast decision might be if someone is an inpatient in a hospital or SNF and they are concerned that the facility is discharging them too soon.
What happens if Medicare denies coverage?
If Medicare denies coverage of an item or service, an individual has the right to appeal the decision. People must provide proof with a claim and submit this to Medicare with an application form.
Who can help you file an appeal for Medicare?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
What is the minimum amount for Medicare appeal?
Before going to Level 3, though, your case must meet the minimum dollar amount. This varies every year; in 2019, the minimum amount is $160.
How long do you have to appeal a level 1 decision?
If you disagree with the decision in Level 1, you have 180 days (6 months) to request a reconsideration from a qualified independent contractor (QIC). Follow the instructions included in the Level 1 decision, making sure you include a written description of why you’re appealing.
What is a Medicare summary notice?
If you have Original Medicare and are denied coverage for a service or item , you should receive a Medicare Summary Notice (MSN) regarding the decision. This details the amount paid (if any) as well as what you owe the provider.
What happens if you disagree with Medicare?
The Medicare appeal process includes five levels, allowing you to continue even if your appeal is denied at one level.
Can you appeal a Medicare plan?
You can also appeal a coverage decision if you have a Medicare health plan (commonly referred to as Part C or Medicare Advantage ). Some of the terminology may be a little different, but the process is basically the same, including the five appeal levels:
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.