Now 99397 or 99396, Preventative Care Exam, for a Medicare patient is not covered by Medicare. Medicare typically does not cover preventative care. There are some exceptions.
Full Answer
Is CPT code 99397 the same as 99387?
Regardless of what the exam is called, the CPT codes 99397 (established patient) and 99387 (new patient), which represent the preventive care examination, have very specific parameters and are never reimbursed by Medicare.
What does 99393 mean in medical terms?
99393 Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; late childhood (age 5 through 11 years)
What is the CPT code for a preventive care exam?
Regardless of what the exam is called, the CPT codes 99397 (established patient) and 99387 (new patient), which represent the preventive care examination, have very specific parameters and are never reimbursed by Medicare.
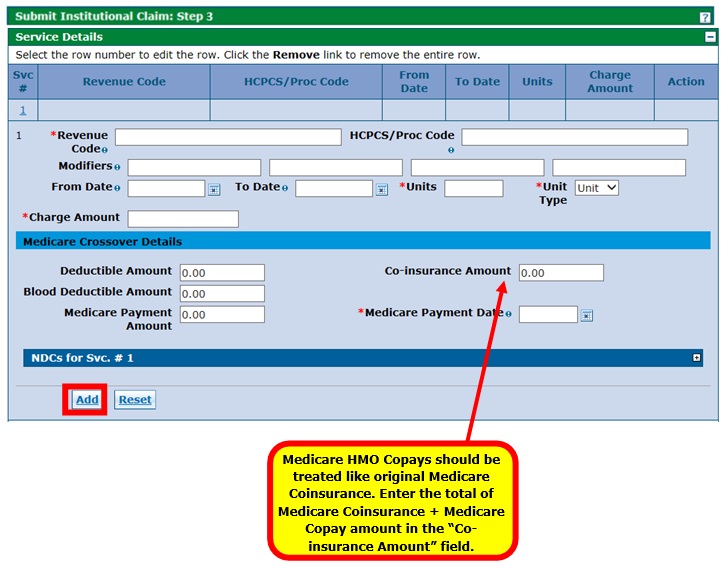
What is the Medicare crossover claim?
Home / Medical Billing Services / What is the Medicare Crossover Claim? What is the Medicare Crossover Claim? A crossover claim is a claim for a recipient who is eligible for both Medicare and Medicaid, where Medicare pays a portion of the claim, and Medicaid is billed for any remaining deductible and/or coinsurance.

Can 99396 be billed to Medicare?
New. We bill Medicare and MCR Advantage plans the Annual Wellness Visit codes G0438 and G0439. We never use 99396 or 99397 for Medicare/MCR Advantage, because they are not a covered code.
What is the Medicare code for 99396?
The Current Procedural Terminology (CPT®) code 99396 as maintained by American Medical Association, is a medical procedural code under the range - Established Patient Preventive Medicine Services.
Does Medicare pay for 99386?
True Blue. The 99386 is not being paid because Medicare does not cover 99386. They have the "Welcome to Medicare and AWV "G" codes. Also, you cannot bill two "new patient" visits.
How do I bill for Medicare Annual Wellness visit?
Coding and Billing a Medicare AWV Medicare will pay a physician for an AWV service and a medically necessary service, e.g. a mid-level established office visit, Current Procedural Terminology (CPT) code 99213, furnished during a single beneficiary encounter.
Does 99396 require a modifier?
Per CCI the 99495 or 99496 cannot have a modifier 25 appended, which may be a hint that it is intended to be billed alone. But a 99396 for example can take a modifier 25. So the combination 99396-25 and 99495 may well be acceptable.
Can 99396 be billed with 99213?
In this case, you may submit codes for both a preventive service (such as 99396) and a regular office visit (such as 99213) by attaching -25 to the office-visit code.
Is 99386 a new patient code?
99386- Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; 40-64 years. Z00.
Can you bill 99396 and g0439?
No you cannot bill the AWV with the preventive visit. You can bill the AWV with a separate E/M.
Can 99396 and 99214 be billed together?
Generally, yes you would want to append Modifier 25 to the 99214, if the services provided include both preventive services and problem management services, and as long as documentation clearly supports both services.
What is the billing code for annual wellness visit?
The two CPT codes used to report AWV services are: G0438 initial visit. G0439 subsequent visit.
What is the difference between a wellness visit and an annual physical?
An annual physical exam is more extensive than an AWV. It involves a physical exam by a doctor and includes bloodwork and other tests. The annual wellness visit will just include checking routine measurements such as height, weight, and blood pressure.
Does Medicare cover CPT code 99397?
A full physical 99397 or 99387 is NOT covered by Medicare and patients are responsible for the cost and can be billed. Some secondary insurance companies may cover the full physical exam, which helps beneficiaries.
What is a 99391?
99391 – Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; infant (age younger than 1 year) – Average fee amount $90
What is the CPT code for preventive medicine?
Preventive Medicine Services [Current Procedural Terminology (CPT®) codes 99381-99387, 99391-99397, Healthcare Common Procedure Coding System (HCPCS) code G0402 are comprehensive in nature, reflect an age and gender appropriate history and examination, and include counseling, anticipatory guidance, and risk factor reduction interventions, usually separate from disease-related diagnoses. Occasionally, an abnormality is encountered or a pre existing problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse the Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.existing problem is addressed during the Preventive visit, and significant elements of related Evaluation and Management (E/M) services are provided during the same visit. When this occurs, Oxford will reimburse the Preventive Medicine service plus 50% the Problem-Oriented E/M service code when that code is appended with modifier 25. If the Problem-Oriented service is minor, or if the code is not submitted with modifier 25 appended, it will not be reimbursed.
What is a periodic comprehensive preventive medicine?
Periodic comprehensive preventive medicine reevaluation and management of an individual includes an age- and gender-appropriate history; physical examination; counseling, anticipatory guidance, or risk factor reduction interventions; and the ordering of laboratory or diagnostic procedures.
What is the primary diagnosis code for HCY?
Providers must use V20.2 as the primary diagnosis on claims for HCY screening services. There are two exceptions. CPT codes 99381EP and 99391EP must be billed with diagnosis code V20.2, V20. 31 or V20 .32. CPT codes 99385 and 99395 must be billed with diagnosis code V25.01-V25.9, V70.0 or V72.31.
What is a CPT 4 exam?
A preventive medicine exam, as described by CPT-4 codes (99384 – 99397), includes a comprehensive age and gender appropriate history, examination, counseling/anticipatory guidance/risk-factor reduction interventions, and the ordering of appropriate immunization (s) and laboratory/diagnostic procedures.
What is CPT in nutrition?
According to CPT, for Medical Nutrition Therapy assessment and/or intervention performed by a physician, report Evaluation and Management or Preventive Medicine service codes.
What is preventive medicine code?
The comprehensive nature of a Preventive Medicine code reflects an age and gender appropriate examination. When a screening code is billed with a Preventiv e Medicine code on the same date of service by the Same Specialty Physician , Hospital, Ambulatory Surgical Center or Other Health Care Professional, only the Preventive Medicine code is reimbursed.
What is a crossover claim for Medicare?
A crossover claim is a claim for a recipient who is eligible for both Medicare and Medicaid, where Medicare pays a portion of the claim, and Medicaid is billed for any remaining deductible and/or coinsurance.
What happens if a Medicare crossover is processed first?
If the crossover claim from Medicare is processed first, the provider submitted claim will be denied as a duplicate claim. If the provider submitted claim is processed prior to the Medicare crossover claim, the provider submitted claim will be paid as it is today if the zero-fill indicator is included on the claim.
What happens if you bill multiple Medicare lines?
If a provider bills multiple lines to Medicare and Medicare pays one or more lines but denies the others, the paid line (s) (as long as there are PRs) will be crossed over to Medicaid and the provider must resubmit the crossover payment as an adjustment to Medicaid to add the additional lines. When Medicare claim payment is zero, ...
Can you bill Medicaid if you have a Medicare remittance?
When the indicator appears on the Medicare remittance you will not bill Medicaid for those clients. Providers can check their Medicare Remittance Advice/ Remittance Remark Code that will verify their claims are crossing over.
Can you fax a medicaid cover sheet?
You may use Medicaid’s web portal to create a fax cover sheet, which should include: Attention: Provider Enrollment. Medicaid also recommends that you add your provider ID number to all pages within your document (including the fax cover sheet).
Does Medicare bill with a rate code?
In most instances, there are no changes to how you bill Medicare however Institutional providers who submit with rate codes are encouraged to include the Medicaid rate code on their claim to Medicare. The amount paid by Medicaid will be the deductible/coinsurance or co-pay amounts as indicated on the crossover claim from Medicare.
Can I use NPI on my Medicare?
The NPI that is used on your Medicare claim must be enrolled with Medicaid. Your crossover claims will not be processed if the NPI on your Medicare claim is not enrolled with Medicaid. In this case, Medicaid will reject the crossover claim back to Medicare and Medicare will send a notification letter of the rejection to the provider.
What is the procedure code for mental health screening?
Providers must use procedure code 96160 or 96161 for the required mental health screening. Procedure codes 96160 and 96161 must be billed with the appropriate medical check-up procedure code. Only one procedure code (96160 or 96161) may be reimbursed once per lifetime.
What age do you need to be to get a mental health checkup?
Mental health screening using one of the validated, standardized mental health screening tools recognized by THSteps is required once for all clients who are 12 through 18 years of age.
Does Medicare cover preventive visits?
This document is designed to assist physicians in documenting, reporting and receiving reimbursement for these services. Medicare does not cover comprehensive preventive visits (99381-99397).
What is the CPT code for a routine physical?
Regardless of what the exam is called, the CPT codes 99397 (established patient) and 99387 (new patient), which represent the preventive care examination, ...
What happens if you get additional tests during the same visit that aren't covered under these preventative benefits?
If you get additional tests or services during the same visit that aren’t covered under these preventative benefits, you may have to pay coinsurance, and the Part B deductible may apply.”. What is there in either a G0438 or G0439 exam that is not covered in a 99397 exam; and, why wouldn’t I just be billed for whatever a 99397 exam covers ...
What is a periodic comprehensive preventive medicine?
Periodic comprehensive preventive medicine reevaluation and management of an individual, including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; 65 years and older.
Is the AWV a preventative physical exam?
The AWV is not an annual routine preventative physical exam. Those exams are much more comprehensive than the AWV. Many healthcare providers believe that the AWV is a routine physical exam and bill the G0438/G0439. That is incorrect.
Is 99397 billed fraudulently?
Additionally, billing the 99397 ( not covered by Medicare) and billing the AWV at the same time is not fraudulent and can be billed if that is exactly what happened and the physician has the proper documentation.
Is 99397 covered by Medicare?
A full physical exam, 99397, is different than an Annual Wellness Visit, G0438/G0439, or “ Welcome to Medicare Exam ”, G0402. A full physical 99397 or 99387 is NOT covered by Medicare and patients are responsible for the cost and can be billed. Some secondary insurance companies may cover the full physical exam, which helps beneficiaries.
Does secondary insurance cover physical exams?
Some secondary insurance companies may cover the full physical exam, which helps beneficiaries. The decision for which service a patient should receive needs to be made prior to any exam as it determines the scope of the exam and the documentation needed for the exam.