The Medicare hospice benefit for patients and families includes the following:
- Home visits by nurses, social workers, hospice aides, chaplains, physicians, nurse practitioners and volunteers as described in the patient’s plan of care
- Medications, supplies and durable medical equipment related to the hospice diagnosis
- Assistance with advance care planning
- Support and education for caregivers
Full Answer
What is the difference between Medicare and hospice?
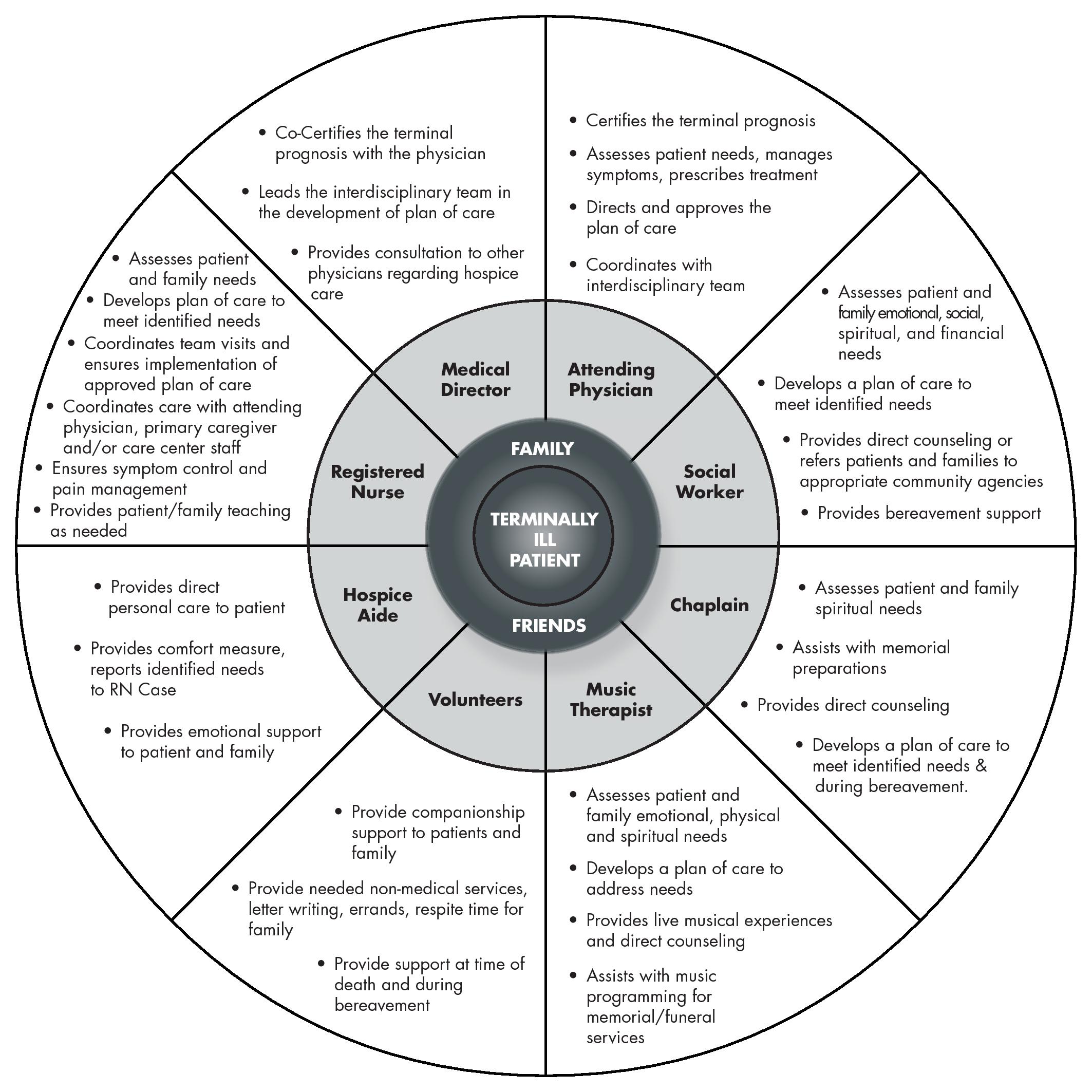
Medications are not covered under Medicare, and medical equipment and supplies may be covered at 80% under Medicare Part B. Hospice is also covered by Medicare, Medicaid and most private insurance plans for eligible patients. Medicare covers medications, medical equipment and supplies related to the terminal diagnosis. Care Team
How much does Medicare cost for hospice?
Medicare covers hospice care costs once a patient reaches all the criteria. These costs might be up to $10,000 per month, depending on the nature of the disease and the level of care required. However, on average, it is usually around $200 for home care and up to $1000 for general inpatient care per day.
Does Medicare provide hospice care coverage?
Yes, Medicare covers hospice care. Both at-home and short-term inpatient hospice care are covered 100%, provided you meet some simple requirements. In this guide, we’ll go over those requirements, as well as what you need to know about hospice care under Medicare. Who is eligible for hospice care under Medicare?
How does Medicare pay for hospice?
OIG referred to its prior reports that recommended CMS work with hospices to make sure they're providing drugs covered under the hospice benefit and develop a strategy to make sure Medicare doesn't pay for hospice-covered drugs. OIG said these suggestions ...
What are the benefits of a hospice program?
7 Benefits of Hospice CareIt Offers a Familiar Environment. ... It Provides a Comprehensive Plan. ... It Offers Personalized Care and Support. ... It Gives Patients a Sense of Dignity. ... It Respects a Patient's Wishes. ... It Lessens Financial Burdens. ... It Provides Family Counseling.
What are the four levels of hospice care?
Every Medicare-certified hospice provider must provide these four levels of care:Hospice Care at Home. VITAS supports patients and families who choose hospice care at home, wherever home is. ... Continuous Hospice Care. ... Inpatient Hospice Care. ... Respite Care.
How long does the average hospice patient live?
Location: Patients admitted to hospice from a hospital are most likely to die within six months. Those admitted from home are next most likely to die within six months and those admitted from nursing homes are least likely.
Can you be on hospice for years?
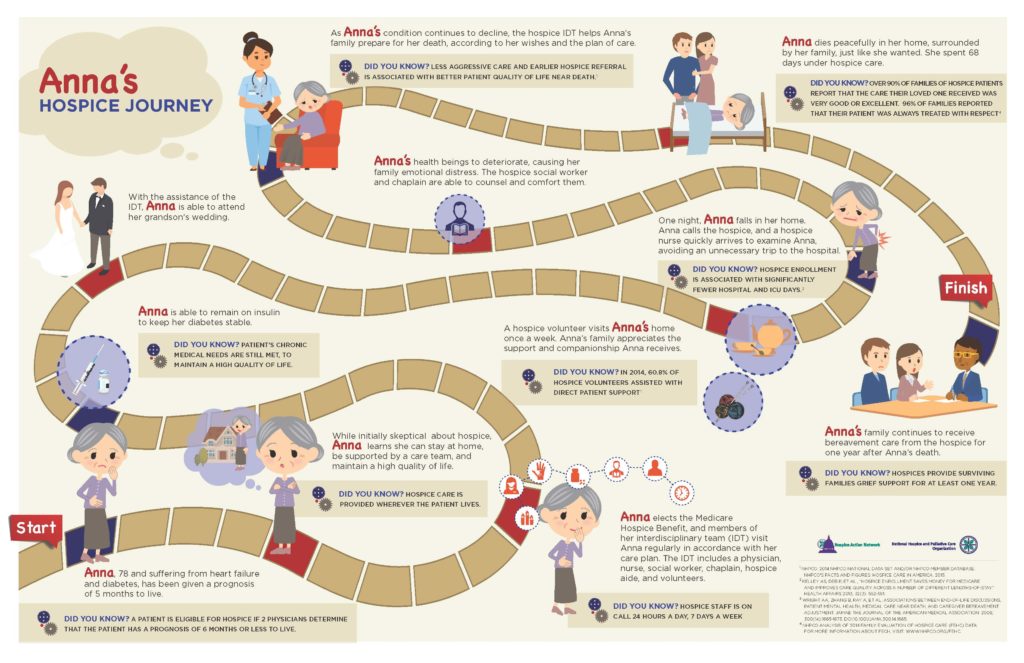
A. You are eligible for hospice care if you likely have 6 months or less to live (some insurers or state Medicaid agencies cover hospice for a full year). Unfortunately, most people don't receive hospice care until the final weeks or even days of life, possibly missing out on months of helpful care and quality time.
How to file a complaint with hospice?
If you or your caregiver has a complaint about the quality of care you get from your hospice provider, you can file a complaint with your hospice provider directly. If you are uncomfortable filing a complaint with your hospice provider, or if you’re dissatisfied with how your hospice provider has responded to your complaint, you can file a complaint with your BFCC-QIO by visiting Medicare.gov/claims-appeals/file- a-complaint-grievance/filing-a-complaint-about-your-quality-of-care or calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
How much does Medicare pay for respite care?
For example, if Medicare approves $100 per day for inpatient respite care, you’ll pay $5 per day and Medicare will pay $95 per day. The amount you pay for respite care can change each year.
What is a Beneficiary and Family Centered Care Quality Improvement Organization?
Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO)—A type of QIO (an organization of doctors and other health care experts under contract with Medicare) that uses doctors and other health care experts to review complaints and quality of care for people with Medicare. The BFCC-QIO makes sure there is consistency in the case review process while taking into consideration local factors and local needs, including general quality of care and medical necessity.
How long do you have to be in hospice to live?
Note: Only your hospice doctor and your regular doctor (if you have one) can certify that you’re terminally ill and have 6 months or less to live.
What is hospice care?
Hospice is a program of care and support for people who are terminally ill (with a life expectancy of 6 months or less, if the illness runs its normal course) and their families. Here are some important facts about hospice:
How to appeal hospice care?
Contact your State Health Insurance Assistance Program (SHIP) if you need help filing or understanding an appeal. For more information on filing a claim or an appeal, visit Medicare.gov/claims-appeals or call 1-800-MEDICARE.
How to find hospice provider?
To find a hospice provider, talk to your doctor, or call your state hospice organization. Visit Medicare.gov/contacts, or call 1-800-MEDICARE (1-800-633-4227) to find the number for your state hospice organization.
How to find out if hospice is Medicare approved?
To find out if a hospice provider is Medicare-approved, ask one of these: Your doctor. The hospice provider. Your state hospice organization. Your state health department. If you're in a Medicare Advantage Plan (like an HMO or PPO) and want to start hospice care, ask your plan to help find a hospice provider in your area. ...
How often can you change your hospice provider?
You have the right to change your hospice provider once during each benefit period. At the start of the first 90-day benefit period, your hospice doctor and your regular doctor (if you have one) must certify that you’re terminally ill (with a life expectancy of 6 months or less).
How long do you have to be on hospice care?
At the start of the first 90-day benefit period, your hospice doctor and your regular doctor (if you have one) must certify that you’re terminally ill (with a life expectancy of 6 months or less). At the start of each benefit period after the first 90-day period, the hospice medical director or other hospice doctor must recertify that you’re terminally ill, so you can continue to get hospice care.
How long can you live in hospice?
Hospice care is for people with a life expectancy of 6 months or less (if the illness runs its normal course). If you live longer than 6 months , you can still get hospice care, as long as the hospice medical director or other hospice doctor recertifies that you’re terminally ill.
What is a hospice aide?
Hospice aides. Homemakers. Volunteers. A hospice doctor is part of your medical team. You can also choose to include your regular doctor or a nurse practitioner on your medical team as the attending medical professional who supervises your care.
When do you have to ask for a list of items and services that are not related to your terminal illness?
If you start hospice care on or after October 1, 2020 , you can ask your hospice provider for a list of items, services, and drugs that they’ve determined aren’t related to your terminal illness and related conditions. This list must include why they made that determination. Your hospice provider is also required to give this list to your non-hospice providers or Medicare if requested.
Does hospice cover inpatient care?
The cost of your inpatient hospital care is covered by your hospice benefit , but paid to your hospice provider.
What does hospice cover?
The Medicare hospice benefit covers all of the care related to your terminal illness and necessary to keep you comfortable, as long as you receive your care from a Medicare-approved hospice vendor. 2 It pays for: Hospice physicians and nurses.
How long do you have to live to be eligible for hospice?
Not everyone can get hospice; you must qualify for it. To be eligible for hospice, you must have a life expectancy of fewer than six months (although if you live longer than six months, ...
How long do you have to be on hospice?
To be eligible for hospice, you must have a life expectancy of fewer than six months (although if you live longer than six months, you can continue to receive hospice benefits as long as your hospice doctor recertifies that you're terminally ill; the recertification is initially after 90 days and 180 days, and then every 60 days thereafter). ...
What is the job of a social worker?
Social workers to help you get your affairs in order and to help you and your family deal with emotional difficulties and grief. Respite care needed to give your caregiver a break. Speech, occupational, or physical therapy needed to keep you comfortable or teach you how to cope with the changes your body is undergoing.
Why are meds necessary?
Medications necessary to keep you comfortable and control or prevent your symptoms.
Can you continue to pay for hospice care with Medicare?
If you're enrolled in a Medicare Advantage plan and you need hospice care, you can choose to remain in that plan as long as you continue to pay the premium, and the Medicare Advantage plan will continue to cover your healthcare needs that are not related to your hospice needs or your terminal condition (or you can choose to get care that's unrelated to your terminal illness via Original Medicare, with the regular deductibles and coinsurance that apply to that coverage).
Is hospice part of Medicare?
The Medicare hospice benefit is part of Medicare Part A. When you sign up for hospice, whether you’re on Original Medicare or a Medicare Advantage Plan like a Medicare HMO, you’ll automatically be covered under the Original Medicare hospice benefit.
What is the coinsurance for respite care?
Respite Care Coinsurance: The patient’s daily coinsurance amount is 5% of the Medicare payment for a respite care day. The coinsurance amount may not be more than the inpatient hospital deductible for the year that the hospice coinsurance period began. This level of care includes room and board costs.
How many days does hospice respite last?
Inpatient respite care: A day the patient elects to get hospice care in an approved inpatient facility for up to 5 consecutive days to give their caregiver a rest.
How much is coinsurance for hospice?
The coinsurance amount is 5% of the cost of the drug or biological to the hospice, determined by the drug copayment schedule set by the hospice. The coinsurance for each prescription may not be more than $5.00. The patient does not owe any coinsurance when they got it during general inpatient care or respite care.
How long can a hospice patient be on Medicare?
After certification, the patient may elect the hospice benefit for: Two 90-day periods followed by an unlimited number of subsequent 60-day periods.
What is the best treatment for a patient who died?
Dietary counseling. Spiritual counseling. Individual and family or just family grief and loss counseling before and after the patient’s death. Short-term inpatient pain control and symptom management and respite care. Medicare may pay for other reasonable and necessary hospice services in the patient’s POC.
What is hospice care?
Hospice is a comprehensive, holistic program of care and support for terminally ill patients and their families. Hospice care changes the focus to comfort care (palliative care) for pain relief and symptom management instead of care to cure the patient’s illness. Patients with Medicare Part A can get hospice care benefits if they meet ...
What is routine home care?
Routine home care: A day the patient elects to get hospice care at home and isn’t getting continuous home care. A patient’s home might be a home, a skilled nursing facility (SNF), or an assisted living facility. Routine home care is the level of care provided when the patient isn’t in crisis.
How to elect hospice?
Individuals must elect the hospice benefit by filing an election statement with a particular hospice. They must acknowledge that they understand that other Medicaid services for the cure or treatment of the terminal condition are waived. Individuals may, however, revoke the election of hospice at any time and resume receipt of the Medicaid-covered benefits waived when hospice was elected.
What is hospice benefit?
The Hospice benefit is an optional state plan service that includes an array of services furnished to terminally ill individuals.
What is IRC in healthcare?
Inpatient Respite Care (IRC), which is short-term care and intended to relieve family members or others caring for the individual. General Inpatient Care (GIC), which is short term and intended for pain control or acute or chronic symptom management which cannot be provided in other settings.
How long is a social worker's service?
The service is provided by a registered nurse or social worker that day for at least fifteen minutes and up to four hours total . The service is not provided by the social worker via telephone.
Can you revoke hospice?
Individuals may , however, revoke the election of hospice at any time and resume receipt of the Medicaid-covered benefits waived when hospice was elected. A hospice provider must obtain a physician certification that an individual is terminally ill and hospice services must be reasonable and necessary for the palliation or management ...
What happens if a hospice beneficiary is discharged?
If a beneficiary revokes or is discharged from hospice care, the remaining days in the benefit period are lost. If/when the beneficiary meets the hospice coverage requirements, they can re-elect the hospice benefit, and will begin with the next benefit period.
How many days does hospice last?
The Medicare hospice benefit consists of two 90- day benefit periods and an unlimited number of sixty-day benefit periods.
Is the 90 day benefit period renewable?
NOTE: The two 90-day benefit periods are not renewable – once they are used, the beneficiary has only 60-day benefit periods remaining. The eligibility systems, ELGA and ELGH, can be used to identify the benefit periods already used by the beneficiary. Refer to “ Chapter Two: Checking Beneficiary Eligibility ” of the Fiscal Intermediary Standard System (FISS) Guide for more information about ELGA and ELGH.