
What is the current Medicare tax rate?
The thresholds are as follows:
- For two married individuals filing jointly, the threshold is $250 000.
- For a married individual filing separately, $125 000.
- The threshold for a single person is $200 000.
- For the head of a household, with a qualifying person – $200 000.
- For a widow (er) with dependent child/ren – $200 000.
How much will Medicare cost this year?
You are eligible for Medicare and premium-free Part A, if you or your spouse paid federal taxes for 40 quarters. If you do not have 40 quarters, you may be eligible to purchase Part A coverage. This costs $458.00 per month if you have less than 30 quarters. If you paid federal taxes for 30 – 39 quarters, the monthly premium for Part A is $252.00.
How much is monthly premium for Medicare?
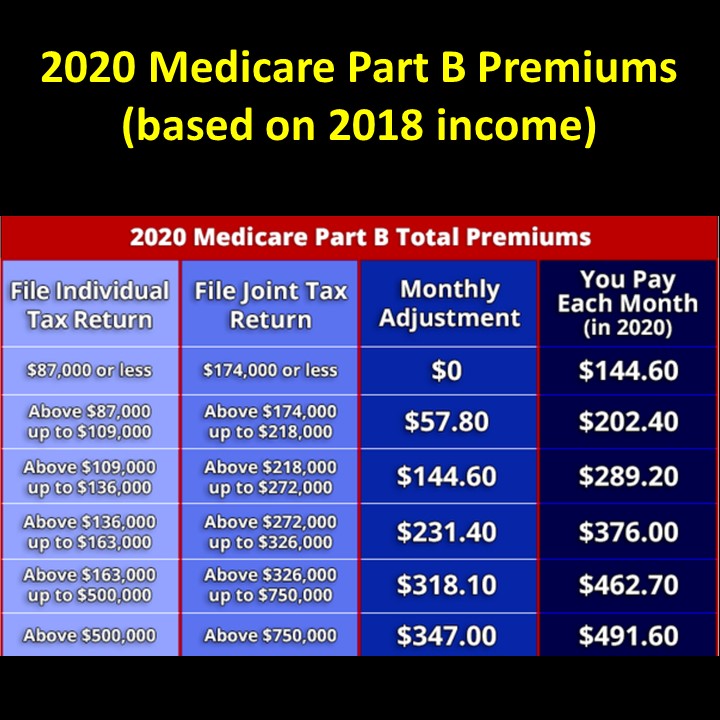
While zero-premium liability is typical for Part A, the standard for Medicare Part B is a premium that changes annually, determined by modified adjusted gross income and tax filing status. For 2020, the standard monthly rate is $144.60.
How much will my Medicare premiums be?
Taxes on your bonuses are likely to be varying between 40% and 45%. In addition to these costs, you will also have to pay National ... but you will also pay Social Security, Medicare, unemployment, and state or local taxes. bonuses are subject to income ...
What are 2021 Medicare premiums?
The Centers for Medicare & Medicaid Services (CMS) has announced that the standard monthly Part B premium will be $148.50 in 2021, an increase of $3.90 from $144.60 in 2020.
What is the cost of Medicare Part B for 2021?
$148.50 forMedicare Part B Premiums/Deductibles The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
Did the cost of Medicare increase for 2021?
In November 2021, CMS announced the monthly Medicare Part B premium would rise from $148.50 in 2021 to $170.10 in 2022, a 14.5% ($21.60) increase.
How much does Medicare take out of Social Security in 2021?
The standard Medicare Part B premium for medical insurance in 2021 is $148.50. Some people who collect Social Security benefits and have their Part B premiums deducted from their payment will pay less.
What is the cost of Medicare Part B for 2022?
$170.10The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
What is the Part B monthly premium for 2021?
$148.50The standard Part B premium amount is $148.50 (or higher depending on your income) in 2021. You pay $203.00 per year for your Part B deductible in 2021.
What is the Medicare Part B increase for 2022?
$170.10In November 2021, CMS announced that the Part B standard monthly premium increased from $148.50 in 2021 to $170.10 in 2022. This increase was driven in part by the statutory requirement to prepare for potential expenses, such as spending trends driven by COVID-19 and uncertain pricing and utilization of Aduhelm™.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
Is Medicare premium based on income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
How much money is taken out of my Social Security check for Medicare?
Medicare Part B (medical insurance) premiums are normally deducted from any Social Security or RRB benefits you receive. Your Part B premiums will be automatically deducted from your total benefit check in this case. You'll typically pay the standard Part B premium, which is $170.10 in 2022.
Does Medicare get deducted from your Social Security check?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
How much will Social Security deduct for Medicare in 2022?
Most people with Medicare will see a 5.9 percent cost-of-living adjustment (COLA) in their 2022 Social Security benefits—the largest COLA in 30 years. This significant COLA increase will more than cover the increase in the Medicare Part B monthly premium.
When will Medicare announce the 2020 rate announcement?
2020 Medicare Advantage and Part D Rate Announcement and Final Call Letter. Fact Sheet. On April 1, 2019 , the Centers for Medicare & Medicaid Services (CMS) released final policy and payment updates to the Medicare Advantage (MA) and Part D programs through the 2020 Rate Announcement and Call Letter. The Advance Notice was posted in two parts: Part ...
What is CMS finalizing for 2020?
Given the urgency and scope of the continuing national opioid epidemic, CMS is finalizing a number of additional policies for 2020 to help Medicare plan sponsors prevent and combat prescription opioid overuse.
Why is the CMS removing the C measure?
CMS is temporarily removing the Controlling High Blood Pressure (Part C) measure from the 2020 and 2021 Star Ratings due to a substantive measure specification change to align with the release of new hypertension treatment guidelines from the American College of Cardiology and American Heart Association .
What is the 2020 star rating?
The 2020 Star Ratings is the final year when all changes to the methodology for calculating the ratings and any changes in the measurement set will be addressed using the Call Letter. CMS is finalizing a policy to adjust the 2020 Star Ratings in the event of extreme and uncontrollable circumstances, such as major hurricane weather events. ...
When will CMS accept comments?
CMS accepted comments on all proposals through March 1, 2019. The final updates will continue to maximize competition among Medicare Advantage and Part D plans, as well as include important actions to address the nation’s opioid crisis.
Can MA health insurance be supplemental?
Traditionally, MA plans have only been allowed to offer “primarily health related” supplemental benefits and must offer these benefits uniformly to all enrollees. Beginning with the 2019 plan year, CMS determined that plans can provide certain enrollees with access to different supplemental benefits.
Does Puerto Rico have Medicare Advantage?
Puerto Rico. In Puerto Rico, a far greater proportion of Medicare beneficiaries receive benefits through Medicare Advantage than in any state or territory. The policies finalized for 2020 will continue to provide stability for the Medicare Advantage program in the Commonwealth and to Puerto Ricans enrolled in MA plans.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
How much does Medicare pay for prescriptions in 2020?
In 2020, the catastrophic coverage threshold is $6,350. Once you are eligible for catastrophic coverage, you will only pay 5% ...
What is the IRMAA for 2020?
In addition to a monthly premium, recipients with certain incomes may be required to pay extra for their Part D plan; this is called the Part D income-related monthly adjust amount (IRMAA). For 2020, this amount is based on the recipient’s tax filing status for 2018.
What factors determine how much the monthly premium will be?
Factors that determine how much the monthly premium will be include the copay the insurer requires for each prescription, the deductible recipients are obligated to pay and the list of drugs available on the carrier’s formulary.
How long does Medicare have to enroll in a Part D plan?
Medicare recipients who do not enroll in a Part D prescription drug plan or have creditable coverage with another plan for 63 days or more past their Initial Enrollment Period may be charges a late enrollment penalty if they choose a Part D plan later on.
Does Medicare limit copayments?
Medicare does not limit the amount plans can require for copayments and coinsurance amounts. Medicare also does not standardize how drugs are categorized into different tiers, which impacts how much the copayment or coinsurance amount for that medication may be in each tier.
Medicare FFS (Part A and Part B)
CMS estimates the Medicare FFS improper payment rate through the Comprehensive Error Rate Testing (CERT) program. Each year, the CERT program reviews a statistically valid stratified random sample of Medicare FFS claims to determine if they were paid properly under Medicare coverage, coding, and payment rules.
Medicare Part C (Medicare Advantage)
The Part C improper payment estimate measures improper payments resulting from errors in beneficiary risk scores. The primary component of most beneficiary risk scores is based on clinical diagnoses submitted by plans for risk-adjusted payment.
Medicare Part D (Prescription Drug Benefit)
The Medicare Part D improper payment estimate measures the payment error related to inaccurately submitted prescription drug event (PDE) data, where the majority of errors for the program exists.
Medicaid and CHIP
CMS estimates Medicaid and CHIP improper payments through the Payment Error Rate Measurement (PERM) program. The improper payment rates are based on reviews of the FFS, managed care, and eligibility components of Medicaid and CHIP in the year under review.
Exchange Improper Payment Measurement
While a FY 2016 risk assessment concluded that the Advance Payments of the Premium Tax Credit (APTC) program is susceptible to significant improper payments, the program is not yet reporting improper payment estimates for FY 2020. CMS is committed to implementing an improper payment measurement program as required by PIIA.
CMS Actions
CMS is committed to reducing improper payments in the Medicare FFS, Medicare Part C, Medicare Part D, Medicaid, and CHIP programs.
What percentage of Medicare reimbursement is for social workers?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate. For example, clinical nurse specialists are reimbursed at 85% for most services, while clinical social workers receive 75%. 1.
What is Medicare reimbursement?
Medicare reimburses health care providers for services and devices they provide to beneficiaries. Learn more about Medicare reimbursement rates and how they may affect you. Medicare reimbursement rates refer to the amount of money that Medicare pays to doctors and other health care providers when they provide medical services to a Medicare ...
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the CY 2021 rule?
The calendar year (CY) 2021 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When is the 2021 Medicare PFS final rule?
The CY 2021 Medicare Physician Fee Schedule Final Rule was placed on display at the Federal Register on December 2, 2020. This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021.
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When is the CY 2020 PFS final rule?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
How much is Medicare Part B 2021?
The standard Medicare Part B premium is $148.50/month in 2021. A 40% surcharge on the Medicare Part B premium is about $700/year per person or about $1,400/year for a married couple both on Medicare. In the grand scheme, when a couple on Medicare has over $176k in income, they are probably already paying a large amount in taxes.
How much does Medicare cover?
The premiums paid by Medicare beneficiaries cover about 25% of the program costs for Part B and Part D. The government pays the other 75%. Medicare imposes surcharges on higher-income beneficiaries. The theory is that higher-income beneficiaries can afford to pay more for their healthcare. Instead of doing a 25:75 split with ...
How long does it take to pay Medicare premiums if income is higher than 2 years ago?
If your income two years ago was higher and you don’t have a life-changing event that makes you qualify for an appeal, you will pay the higher Medicare premiums for one year. IRMAA is re-evaluated every year as your income changes.
What percentage of Medicare premiums do Medicare beneficiaries pay?
The premiums paid by Medicare beneficiaries cover about 25% of the program costs for Part B and Part D. The government pays the other 75%.
How much does Medicare premium jump?
If your income crosses over to the next bracket by $1, all of a sudden your Medicare premiums can jump by over $1,000/year. If you are married and both of you are on Medicare, $1 more in income can make the Medicare premiums jump by over $1,000/year for each of you.
When will IRMAA income brackets be adjusted for inflation?
The IRMAA income brackets (except the very last one) started adjusting for inflation in 2020. Here are the IRMAA income brackets for 2021 coverage and the projected brackets for 2022 coverage. Before the government publishes the official numbers, I’m able to make projections based on the inflation numbers to date.
