How do Medicare payment systems work?
A Prospective Payment System (PPS) refers to several payment formulas when reimbursement depends on predetermined payment regardless of the intensity of services provided. Medicare bases payment on codes using the classification system for that service (such as diagnosis-related groups for hospital inpatient services and ambulatory payment classification for …
How does Medicare pay for inpatient and outpatient care?
May 22, 2020 · A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What is the prospective payment system used to reimburse home health agencies?
Nov 15, 2021 · A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What does PPS stand for in Medicare?
The RBRVS system is the basis for the Medicare payment system (T/F) T Preferred provider organization (PPOs) never allow members to receive care from providers outside the network (T/F) False, They may; a higher percentage of charges will need to be paid Exclusions are expenses covered by an insurance company (T/F) False, Not covered

What payment system is used by the Centers for Medicare and Medicaid?
The resource-based relative value scale (RBRVS) is the physician payment system used by the Centers for Medicare & Medicaid Services (CMS) and most other payers.
What is the payment system Medicare uses for establishing payment for hospital stays?
PPS is Medicare's system for reimbursing Part A inpatient hospital cost, and the amount of payment is determined by the assigned diagnosis-related group (DRG).
What is the IPPS payment system?
Section 1886(d) of the Social Security Act (the Act) sets forth a system of payment for the operating costs of acute care hospital inpatient stays under Medicare Part A (Hospital Insurance) based on prospectively set rates. This payment system is referred to as the inpatient prospective payment system (IPPS).Apr 18, 2022
What replaced the reasonable cost based payment system?
PPS replaced the retrospective cost-based system of payment for Medicare services with a prospective payment system. Under PPS, a predetermined specific rate for each discharge dictates payment according to the diagnosis related group (DRG) in which the discharge is classified.
What are Rbrvs used for?
Resource-based relative value scale (RBRVS) is a schema used to determine how much money medical providers should be paid. It is partially used by Medicare in the United States and by nearly all health maintenance organizations (HMOs).
What are the basis of the IPPS?
The IPPS pays a flat rate based on the average charges across all hospitals for a specific diagnosis, regardless of whether that particular patient costs more or less. Everything from an aspirin to an artificial hip is included in the package price to the hospital.
What does IPPS stand for?
IPPSAcronymDefinitionIPPSInpatient Prospective Payment System (medical payments)IPPSInternational Parallel Processing SymposiumIPPSInternational Planned Parenthood Federation (est. 1952)IPPSInternational Pelvic Pain Society11 more rows
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).
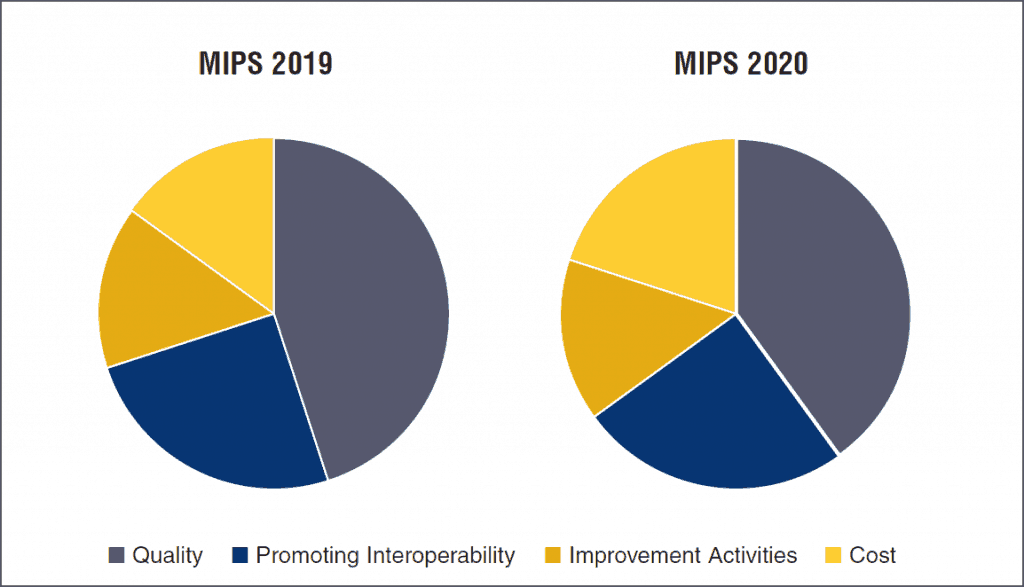
What is MIPS score?
MIPS is a performance-based payment system composed of four categories that provide clinicians the flexibility to choose the activities and measures that are most meaningful to their practice . An eligible clinician’s performance in each of the four weighted performance categories is combined to create the MIPS Composite Performance Score, also known as the MIPS Final Score, which is used to determine Medicare Part B payment adjustments in future years.
What is improvement activity?
The Improvement Activities category of MIPS is intended to encourage eligible clinicians to participate in activities that improve clinical practice in areas such as shared decision making, patient safety, coordinating care, and increasing access.
