If your primary payer was Medicare, Medicare Part B would pay 80 percent of the cost and cover $80. Normally, you’d be responsible for the remaining $20. If you have a secondary payer, they’d pay the $20 instead.
How does Medicare work when it is a secondary insurance?
- You will always have the choice of keeping your employer health insurance when you are eligible for Medicare if you work for a large company
- Depending on the size of your company, Medicare may be your primary or secondary insurance
- Medicare also works with COBRA, TRICARE, VA benefits, and HRAs
Can Medicare be used as a secondary insurance?
“Depending on the size of the employer, Medicare can be primary or Medicare can be secondary,” Mordo says. If the employer has 20 or more employees, the employer’s health plan will be primary, and Medicare will be secondary.
Is Medicare ever used as a secondary insurance carrier?
You can still get Medicare if you’re insured by a private company, but there are some occasions when Medicare becomes the secondary payer for your benefits. Being a “secondary payer” means that Medicare is second-in-line to paying your healthcare claims.
Will Medicaid cover my co-pay as secondary insurance?
Qualified low-income individuals and families may be able to use Medicaid as a secondary insurance to cover insurance premiums, deductibles or co-pays. Medicaid is the government-funded health insurance program administered in each state. Both the name of the program and its requirements vary by state.
What is the cost of supplemental insurance for Medicare?
Medicare Supplement Plans have premiums that cost anywhere from around $70/month to around $270/month. Typically, plans with higher monthly premiums will have lower deductibles. Plans with lower monthly premiums typically have higher deductibles.
What is the average cost of AARP Medicare supplement insurance?
1. AARP Medigap costs in states where age doesn't affect the pricePlan nameAverage monthly cost for AARP MedigapPlan B$242Plan C$288Plan F$256Plan G (our recommendation for best overall plan)$1936 more rows•Jan 24, 2022
What is the monthly premium for Plan G?
How Much Does a Medigap Plan G Cost?StateMonthly premium rangeNumber of Plans availableColorado$110 to $375 $32 to $66 high-deductible57 total *49 (attained age) ^4 (community) ~4 (issue age)California$128 to $246 $37 to $81 high-deductible28 total *26 (attained age) ^2 (issue age)1 more row•Apr 12, 2022
What is the deductible for Plan G in 2022?
$2,490Medigap Plan F and Plan G have high-deductible options that include an annual deductible of $2,490 in 2022. Plan members must meet this deductible before the plan begins to cover any of Medicare out-of-pocket expenses.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Why does AARP recommend UnitedHealthcare?
AARP endorses UnitedHealthcare as part of a marketing agreement between the two companies. For each plan sold, AARP receives a royalty payment from UnitedHealthcare. However, AARP/UnitedHealthcare Medicare Advantage plans generally provide good coverage at affordable prices.
What is the difference in Plan G and N?
This is where the differences between Plan G and N start. Plan G covers 100% of all Medicare-covered expenses once your Part B deductible has been met for the year. Medicare Plan N coverage, on the other hand, has a few additional out-of-pocket expenses you will have to pay, which we'll cover next.
Is Medicare G the best plan?
Medicare Plan G is currently the most comprehensive Medicare Supplement plan in terms of the coverage it offers. If you desire stability and knowing what to expect from your health care costs (and if you can afford the premium), Medicare Plan G may be the best option for you.
What is the plan g deductible for 2021?
$2,370Effective January 1, 2021, the annual deductible amount for these three plans is $2,370. The deductible amount for the high deductible version of plans G, F and J represents the annual out-of-pocket expenses (excluding premiums) that a beneficiary must pay before these policies begin paying benefits.
What is the Medicare Part B premium for 2022?
$170.10The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
Does AARP offer high deductible plan G?
AARP also offers a high-deductible version of Plan G. This option will require you to pay a deductible of $2,340 before the plan begins to assist with costs. Once you've met your deductible, the plan will pay 100% of covered costs for the remainder of the year.
What is the difference between plan F and plan G?
Medigap Plan G is currently outselling most other Medigap plans because it offers the same broad coverage as Plan F except for the Part B deductible, which is $233 in 2022. The only difference when you compare Medicare Supplements Plan F and Plan G is that deductible. Otherwise, they function just the same.
What is secondary coverage for health insurance?
Secondary health insurance policies can fill in any coverage gaps, such as vision coverage, and available policies can also reduce the cost of heal...
Can you have two health insurance plans at the same time?
Yes, it's common to have multiple health insurance policies, and dual coverage can help cover more of your medical costs so that you pay less out o...
Which insurance companies offer secondary health insurance?
Plans are available from Blue Cross Blue Shield, USAA, AARP, UnitedHealthcare, Aetna, Aflac, Alliance, Humana, Cigna and more.
Is secondary health insurance worth it?
Secondary health insurance can give you financial protection if your main insurance policy has limitations. Most people have some form of secondary...
How much does secondary health insurance cost?
Secondary health insurance can cost anywhere from $5 per month to hundreds of dollars per month, depending on the type of coverage and the level of support the plan provides.
What is secondary insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance.
What is Medicare Supplemental Insurance?
Medicare supplemental insurance: Also called Medigap plans, these supplemental plans can help cover services that are not covered by Original Medicare. Plans can also help pay your out-of-pocket costs for deductibles, copayments and coinsurance.
How to reduce the cost of pregnancy?
You can reduce the cost of your pregnancy by signing up for supplemental health insurance for pregnant women. Options include short-term disability insurance and a maternity leave plan, which can help replace the lost income. Plus, a hospital indemnity plan can reduce your out-of-pocket hospital costs by giving you a direct cash payment for covered situations. The best policy for you will depend on your specific needs.
Why combine secondary insurance with cheap insurance?
Combining secondary health insurance with a cheap health insurance plan can help you pay less for broad coverage that would be more expensive if you purchased only one plan.
How much does Medicare supplement cost?
The cost of Medicare supplement plans has the biggest range because of the variety of plans and coverage options. Low-cost plans such as Plan K start at just $62 per month, and other choices such as Plan A or Plan B can cost more than $700 per month.
What happens if you have multiple insurance policies?
If you have multiple insurance policies, there is a clear order in which the plans will pay for health care services.
What is the standard Medicare premium for 2021?
In 2021, the standard premium is $148.50. However, even with this added cost, many people find their overall costs are lower, since their out-of-pocket costs are covered by the secondary payer. Secondary payers are also useful if you have a long hospital or nursing facility stay.
How does Medicare and Tricare work together?
Medicare and TRICARE work together in a unique way to cover a broad range of services. The primary and secondary payer for services can change depending on the services you receive and where you receive them. For example: TRICARE will pay for services you receive from a Veteran’s Administration (VA) hospital.
How much does Medicare pay for an X-ray?
For example, if you had a X-ray bill of $100, the bill would first be sent to your primary payer, who would pay the amount agreed upon by your plan. If your primary payer was Medicare, Medicare Part B would pay 80 percent of the cost and cover $80. Normally, you’d be responsible for the remaining $20. If you have a secondary payer, they’d pay the $20 instead.
How does Medicare work with employer sponsored plans?
Medicare is generally the secondary payer if your employer has 20 or more employees . When you work for a company with fewer than 20 employees, Medicare will be the primary payer.
What is primary payer?
A primary payer is the insurer that pays a healthcare bill first. A secondary payer covers remaining costs, such as coinsurances or copayments. When you become eligible for Medicare, you can still use other insurance plans to lower your costs and get access to more services. Medicare will normally act as a primary payer and cover most ...
What can help you decide if a secondary payer makes sense for you?
Your budget and healthcare needs can help you decide if a secondary payer makes sense for you.
Does Medicare cover coinsurance?
Medicare will normally act as a primary payer and cover most of your costs once you’re enrolled in benefits. Your other health insurance plan will then act as a secondary payer and cover any remaining costs, such as coinsurance or copayments.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Does Medicare pay for workers compensation?
Medicare generally will not pay for an injury or illness/disease covered by workers’ compensation. If all or part of a claim is denied by workers’ compensation on the grounds that it is not covered by workers’ compensation, a claim may be filed with Medicare.
How does Medicare work with insurance carriers?
Generally, a Medicare recipient’s health care providers and health insurance carriers work together to coordinate benefits and coverage rules with Medicare. However, it’s important to understand when Medicare acts as the secondary payer if there are choices made on your part that can change how this coordination happens.
Who is responsible for making sure their primary payer reimburses Medicare?
Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment. Medicare recipients are also responsible for responding to any claims communications from Medicare in order to ensure their coordination of benefits proceeds seamlessly.
What does a primary payer do?
In the simplest of terms, a primary payer will cover the cost of a health care bill according to its policy rules and up to the limit established therein.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
How much will Medicare premiums be in 2021?
If you don’t qualify for a premium-free Part A, you might be able to buy it. In 2021, the premium is either $259 or $471 each month, depending on how long you or your spouse worked and paid Medicare taxes.
How much do you pay for Medicare after you pay your deductible?
You’ll usually pay 20% of the cost for each Medicare-covered service or item after you’ve paid your deductible.
How often do you pay premiums on a health insurance plan?
Monthly premiums vary based on which plan you join. The amount can change each year. You may also have to pay an extra amount each month based on your income.
How often do premiums change on a 401(k)?
Monthly premiums vary based on which plan you join. The amount can change each year.
Is there a late fee for Part B?
It’s not a one-time late fee — you’ll pay the penalty for as long as you have Part B.
Do you have to pay Part B premiums?
You must keep paying your Part B premium to keep your supplement insurance.
What type of insurance is ordered to pay for care before Medicaid?
Some of the coverage types that may be ordered to pay for care before Medicaid include: Group health plans. Self-insured plans. Managed care organizations. Pharmacy benefit managers. Medicare. Court-ordered health coverage. Settlements from a liability insurer. Workers’ compensation.
What is a dual eligible Medicare beneficiary?
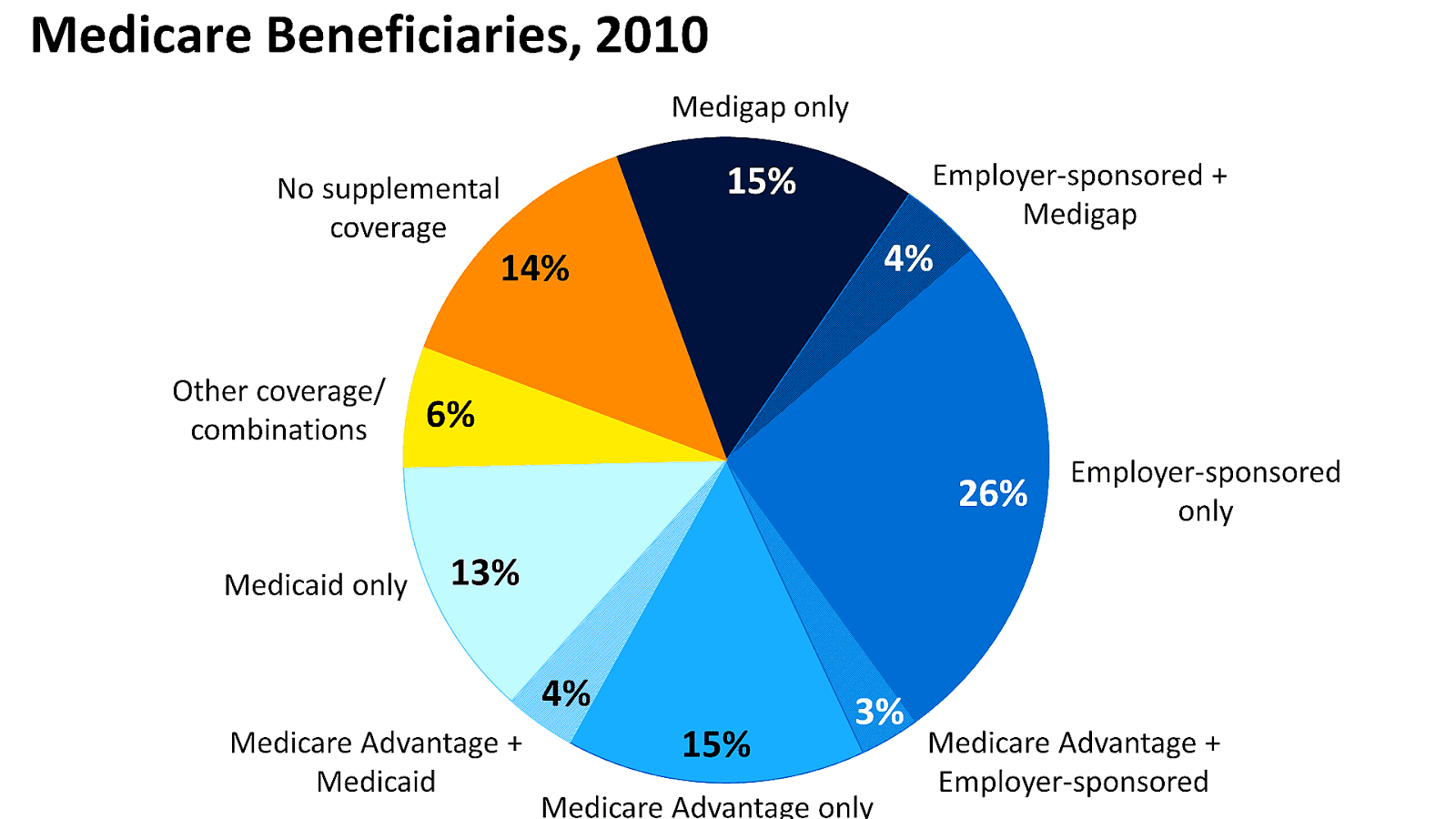
Dual-eligible beneficiaries are often automatically enrolled in a Medicare Savings Program (MSP), which covers the Medicare Part B premium and may offer additional services.
What is the last resort for medicaid?
Medicaid acts as the “payer of last resort” when a beneficiary has an employer-based or other private commercial insurance plan. This means Medicaid will be the last plan to contribute to a medical bill and may pick up copayments and coinsurances in similar fashion to how Medicaid works with Medicare.
What is third party liability?
Third party liability. Under federal law, all other sources of health care coverage must pay claims first before Medicaid will pick up any share of the cost of care. This is referred to as “third party liability” (TPL), which means the primary payment for care is the responsibility of any available third-party resources and not that of Medicaid.
Can you be on Medicare and Medicaid at the same time?
Some people are eligible for both Medicare and Medicaid and can be enrolled in both programs at the same time. These beneficiaries are described as being “dual eligible.”.
Is medicaid a primary or secondary insurance?
Medicaid can work as both a primary or secondary insurer. In this Medicaid review, we explore when and how the program works as secondary, or supplemental, insurance that can coordinate with other types of insurance.
Does Medicare pick up coinsurance?
Copayments and coinsurances that are left remaining after Medicare applies its coverage will be picked up by Medicaid. Dual-eligible beneficiaries can expect to pay little to nothing out of their own pocket after Medicaid has picked up its share of the cost.
What is senior supplement?
Senior Supplements. Supplemental health insurance for seniors, which is sold by private health insurance companies, is an addition to existing healthcare coverage that’s designed specifically to meet seniors’ needs.
Does Medicare Supplement cover dental?
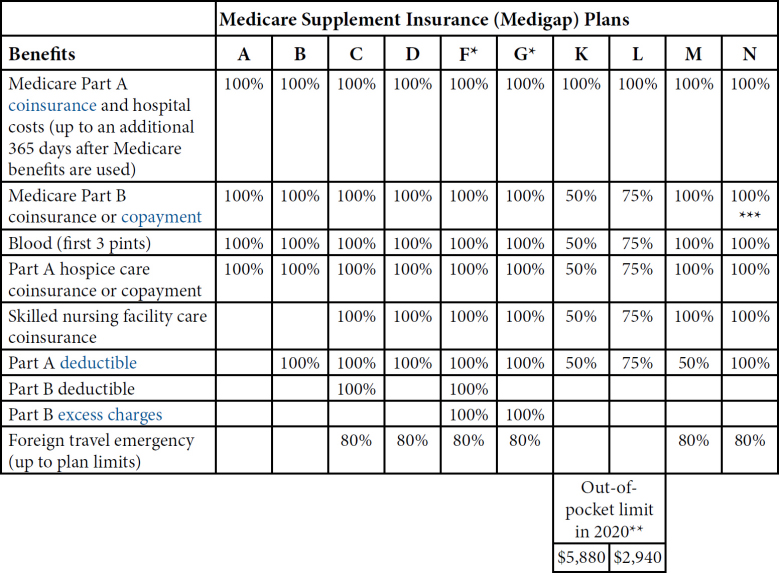
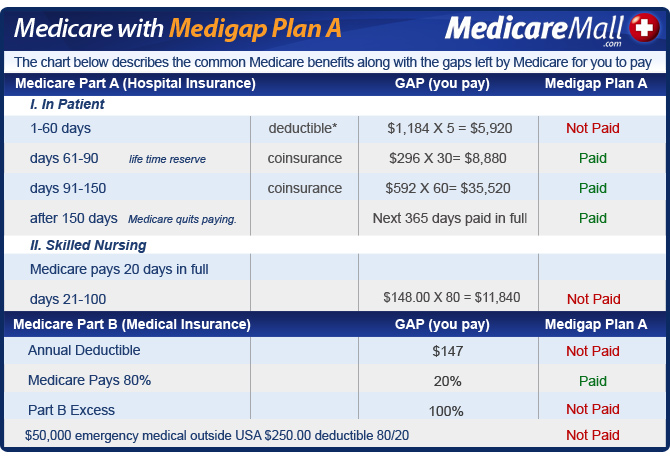
Like Medicare’s “parts,” each plan offers different benefits and has a different premium amount. These plans cover healthcare expenses that Medicare doesn ’t pay for such as coinsurance and deductibles. But, Medigap plans do not cover dental, vision, or any other supplemental health insurance benefits.
Does Medicare cover dental insurance?
These plans cover healthcare expenses that Medicare doesn’t pay for such as coinsurance and deductibles. But, Medigap plans do not cover dental, vision, or any other supplemental health insurance benefits.
Is there a Medicare Supplement plan for seniors?
There’s no single supplemental health insurance plan for seniors that fits everyone. But there is most likely a plan that will fit your specific needs. HealthMarkets can make finding a plan easy. Get a free quote for supplemental health insurance for seniors. Or, if you’re looking for the cost of Medicare Supplement plans, answer a few quick questions about your preferences. Then, HealthMarkets FitScore® technology will help you compare Medicare supplement plans and find one that’s the right fit for your needs. Get started today!
How is Medicare Supplement Plan cost determined?
The cost of a Medicare Supplement plan is determined by the individual insurance company that sells it. When researching different companies, be sure to ask how they price their policies. 10 Learning which factors they base their pricing on will help you determine both the costs for you today and what to expect in the future if your health situation changes.
How long do you have to switch back to Medicare Advantage?
If you’re unhappy with your Advantage plan and switch back to a Medicare Original Plan (which you can do within 12 months of enrolling in the Medicare Advantage plan), you then become eligible for Medicare Supplement insurance.
Why is AARP the best Medicare supplement?
We chose AARP as best for its set pricing for Medicare Supplement coverage because it doesn’t charge more as you grow older. This is especially helpful if you are still covered under your employer's insurance and may require coverage after the age of 65.
What is a Medicare Supplement Plan?
A Medicare Supplement Plan, also called a Medigap plan, is a plan sold by private companies, separate from Medicare. Medicare Supplement plans pay for the costs, or “gaps,” in coverage that are not paid for by Original Medicare. These can include prescriptions, doctor visits, vision and dental care, and more.
When is the best time to buy a Medicare Supplement?
The best time to buy a Medicare Supplement policy is during your Initial Medicare Open Enrollment Period. This is a one-time only, six-month span when federal law allows you to sign up for any Medicare Supplement policy you want that is sold in your state. Preexisting conditions are accepted during this time period, and you can't be denied a Medicare Supplement policy or charged more due to past or present health problems. Make sure you know when your Open Enrollment Period starts. 12
What to do if you have a gap in Medicare?
If you’re experiencing a gap in coverage from Medicare, then you may need to choose supplemental coverage . Explore your options when it comes to finding out what coverage you’re lacking and if things like prescriptions, doctor visits, vision, and dental care are covered or if you need help paying for them. If you’re not fully covered, then consider purchasing supplemental insurance.
Is Medicare Advantage the same as Medigap?
Both Medicare Advantage and Medigap plans are supplements to Original Medicare, but they are different. Medicare Advantage is an alternative Medicare plan. Medicare Advantage has a low or $0 monthly charge and covers most prescription medicine, though the choice of doctors and networks may be limited.