The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the Department of Health and Human Services (HHS) . CMS also monitors Medicaid programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion.
What is the Department of Health and Medicare?
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children’s Health Insurance Program (CHIP).
What does the Centers for Medicare and Medicaid (CMS) do?
CMS is a branch of the The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children’s Health Insurance Program (CHIP). . CMS also monitors
What agency runs the Medicare program?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the Department Of Health And Human Services (Hhs)
How is Medicare funded?
How is Medicare funded? The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the
Which department of the federal government is responsible for the Medicare program?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Does the government contribute to Medicare?
Is Medicare funded by the state or federal government? Medicare is a federal program, and as a result, the vast majority of Medicare funding comes from the federal government. However, state governments do make a small contribution for enrollees who qualify for both Medicare and Medicaid.
Who decides Medicare coverage?
Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
How is Medicare primarily funded?
A: Medicare is funded with a combination of payroll taxes, general revenues allocated by Congress, and premiums that people pay while they're enrolled in Medicare. Medicare Part A is funded primarily by payroll taxes (FICA), which end up in the Hospital Insurance Trust Fund.
Why is Medicare conditional?
Medicare makes this conditional payment so you will not have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare when a settlement, judgment, award, or other payment is made.
What is a POR in Medicare?
A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities.
What is a RAR letter for MSP?
After the MSP occurrence is posted, the BCRC will send you the Rights and Responsibilities (RAR) letter. The RAR letter explains what information is needed from you and what information you can expect from the BCRC. A copy of the Rights and Responsibilities Letter can be found in the Downloads section at the bottom of this page. Please note: If Medicare is pursuing recovery directly from the insurer/workers’ compensation entity, you and your attorney or other representative will receive recovery correspondence sent to the insurer/workers’ compensation entity. For more information on insurer/workers’ compensation entity recovery, click the Insurer Non-Group Health Plan Recovery link.
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
Can you get Medicare demand amount prior to settlement?
Also, if you are settling a liability case, you may be eligible to obtain Medicare’s demand amount prior to settlement or you may be eligible to pay Medicare a flat percentage of the total settlement. Please see the Demand Calculation Options page to determine if your case meets the required guidelines. 7.
What is BCRC in Medicare?
Benefits Coordination & Recovery Center (BCRC) - The BCRC consolidates the activities that support the collection, management, and reporting of other insurance coverage for beneficiaries. The BCRC takes actions to identify the health benefits available to a beneficiary and coordinates the payment process to prevent mistaken payment of Medicare benefits. The BCRC does not process claims, nor does it handle any GHP related mistaken payment recoveries or claims specific inquiries. The Medicare Administrative Contractors (MACs), Intermediaries and Carriers are responsible for processing claims submitted for primary or secondary payment.
What is Medicare investigation?
The investigation determines whether Medicare or the other insurance has primary responsibility for meeting the beneficiary's health care costs. Collecting information on Employer Group Health Plans and non-group health plans (liability insurance ...
What is a COB plan?
Coordination of benefits (COB) allows plans that provide health and/or prescription coverage for a person with Medicare to determine their respective payment responsibilities (i.e., determine which insurance plan has the primary payment responsibility and the extent to which the other plans will contribute when an individual is covered by more than one plan).
Does Medicare pay a claim as a primary payer?
Where CMS systems indicate that other insurance is primary to Medicare, Medicare will not pay the claim as a primary payer and will return it to the provider of service with instructions to bill the proper party.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
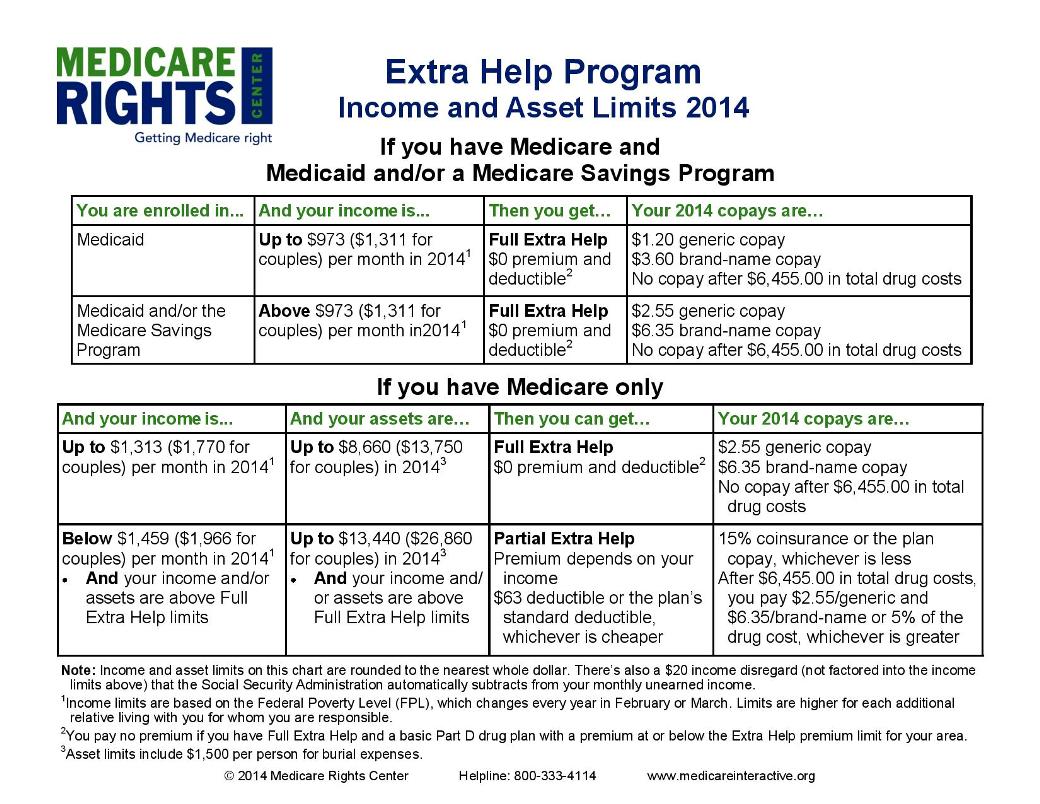
What is QMB in Medicare?
The Qualified Medicare Beneficiary ( QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program.
Can a QMB payer pay Medicare?
Billing Protections for QMBs. Federal law forbids Medicare providers and suppliers, including pharmacies, from billing people in the QMB program for Medicare cost sharing. Medicare beneficiaries enrolled in the QMB program have no legal obligation to pay Medicare Part A or Part B deductibles, coinsurance, or copays for any Medicare-covered items ...
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.