Medicare Part B does not cover for Durable Medical Equipment that is not suitable for use in the home. This includes some types of equipment used in skilled nursing facilities or hospitals, such as: Oscillating beds
What doesn't Medicare cover?
Medicare doesn't cover everything. Even if Medicare covers a service or item, you generally have to pay your Deductible , Coinsurance, and Copayment . Find out if Medicare covers a test, item, or service you need.
Does Medicare cover durable medical equipment?
Original Medicare’s Part B covers durable medical equipment items when your Medicare-enrolled doctor or health care provider prescribes it for you to use at home. Once you have the doctor’s prescription, you can take it to any Medicare-enrolled supplier.
Does Medicare cover DME?
Medicare Part B (Medical Insurance) covers Medically necessary DME if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: Blood sugar meters Blood sugar test strips; Canes Commode chairs; Continuous passive motion devices Continuous Positive Airway Pressure (CPAP) devices; Crutches; Hospital beds
What is considered durable medical equipment (DME)?
durable medical equipment (DME) if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: Air-fluidized beds & other support surfaces (these supplies are only rented) Blood sugar monitors. Blood sugar test strips. Canes. Commode chairs. Continuous passive motion machines.

What kinds of medical care are not paid Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
Which item is not covered by Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What is not an example of durable medical equipment DME?
As its name implies, the equipment must be durable, meaning that it could normally be used by successive patients. Disposable medical supplies, such as incontinence pads and catheters, are not considered to be DME based on Medicare rules, as they generally cannot be re-used or used by successive patients.
Is DME covered by Medicare Part B?
DME is reusable medical equipment, like walkers, wheelchairs, or hospital beds. If I have Medicare, can I get DME? Anyone who has Medicare Part B (Medical Insurance) can get DME as long as the equipment is medically necessary.
What diagnosis codes are not covered by Medicare?
Non-Covered Diagnosis CodesBiomarkers in Cardiovascular Risk Assessment.Blood Transfusions (NCD 110.7)Blood Product Molecular Antigen Typing.BRCA1 and BRCA2 Genetic Testing.Clinical Diagnostic Laboratory Services.Computed Tomography (NCD 220.1)Genetic Testing for Lynch Syndrome.More items...•
What types of procedures usually are not covered by insurance?
Health insurance typically covers most doctor and hospital visits, prescription drugs, wellness care, and medical devices. Most health insurance will not cover elective or cosmetic procedures, beauty treatments, off-label drug use, or brand-new technologies.
Is a heart monitor considered durable medical equipment?
Note: Pulse tachometers (pulse rate monitors, heart rate monitors) do not meet Aetna's definition of covered durable medical equipment (DME) in that they are not primarily medical in nature and are normally of use in the absence of illness or injury.
What classifies as durable medical equipment?
Durable medical equipment (DME) is equipment that helps you complete your daily activities. It includes a variety of items, such as walkers, wheelchairs, and oxygen tanks. Medicare usually covers DME if the equipment: Is durable, meaning it is able to withstand repeated use.
Is a sliding board covered by Medicare?
QUESTION: Are Transfer Boards covered by Medicare? ANSWER: Transfer boards may be considered medically necessary for patients with medical conditions that limit their ability to transfer from wheelchair to bed, chair, or toilet. For Medicare coverage of these products visit a local supplier.
Is a knee brace durable medical equipment?
Orthotic devices like braces are otherwise known as Durable Medical Equipment. Braces may be used to support the knee, neck, arm, or back. Combining the use of orthotic devices with other treatments may delay the need for a surgical procedure.
Does Medicare pay for walkers and shower chairs?
Q: Will Medicare cover the cost of wheelchairs and walkers? A: Yes. Medicare Part B covers a portion of the cost for medically-necessary wheelchairs, walkers and other in-home medical equipment.
How Much Does Medicare pay for a rollator?
In most cases, Medicare will pay 80% of the rolling walker costs. Be sure to check your supplemental insurance policy for the details of your plan that will cover whatever Medicare does not –minimizing as much out of pocket expense as possible.
What is not covered by Medicare?
Medicare only covers DME that is medically necessary, not convenient. Therefore, items that are intended only to make things more convenient or comfortable are not covered by Medicare.
How many parts are there in Medicare?
There are four parts to the Medicare plan: A, B, C, and D. Each of these parts covers different parts of healthcare, with parts A and B being the most common parts that people enroll in. You can enroll in one or more parts of Medicare, depending on your income.
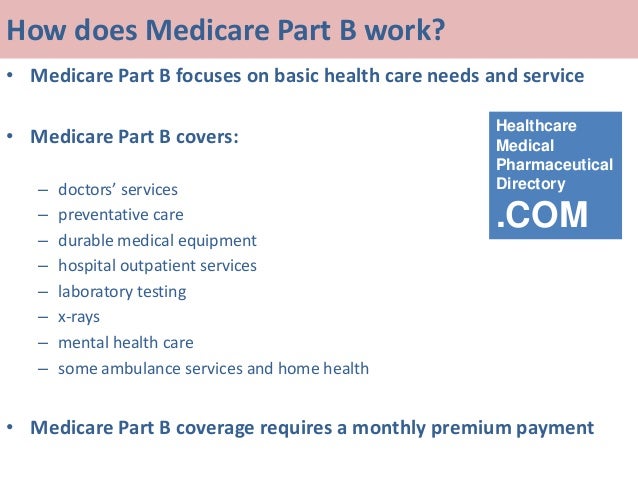
What is Medicare Part B?
Out of the four parts, Medicare Part B is the part of the Medicare plan that helps to pay for Durable Medical Equipment (DME). DME is any specialized piece of medical equipment that your doctor prescribes for you to use at home on a long-term basis.
How much does Medicare pay for DME?
For qualified beneficiaries, Medicare pays 80% of the cost of the covered DME. If you do not have additional insurance that covers this cost, then you are responsible for the remaining 20%. However, Medicare may not pay the 80% if you are buying the DME from a supplier that is not Medicare-approved.
How many people will be covered by the 2020 Medicare?
This federal health insurance program provides coverage to millions of Americans, with enrollment expected to reach 64 million in 2020. The program not only covers seniors aged 65 and above, but it also covers younger people with long-term disabilities and those with permanent kidney failure.
Does Medicare pay for incontinence pads?
Incontinence pads. Under pads. Besides incontinence products , Medicare does not disposable products, such as surgical facemasks, intravenous supplies, catheters, compression leggings, disposable sheets, and gauze, etc. However, Medicare may pay for some of these items disposable items if you receive home health care.
Does Medicare cover medical equipment outside the home?
2. Equipment mainly intended for use outside the home. Medicare Part B covers for durable medical equipment that patients can use around the house. So, if you can walk on your own for short distances within your home, Medicare will not cover for equipment that you only need outside the home, such as”.
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
What are the drugs covered by Medicare?
Some of the drugs Medicare Part B does cover can include: 1 Drugs used with an item of durable medical equipment such as a nebulizer 2 Certain antigens 3 Injectable osteoporosis drugs 4 Erythropoietin by injection 5 Blood clotting factors 6 Oral drugs given for End-Stage Renal Disease 7 Enteral nutrition, such as intravenous and tube feeding 8 Intravenous Immune Globulin (IVIG) that is provided at home 9 Transplant and immunosuppressive drugs
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (Medigap) Medicare Supplement Insurance plans are used to cover some of the out-of-pocket expenses associated with Original Medicare, such as deductibles and copayments. Medicare Supplement Insurance plans can work alongside your Original Medicare benefits. You cannot have a Medigap plan and a Medicare Advantage plan ...
How often does Medicare cover diabetic eye exams?
Eye exams for diabetic retinopathy can be covered once a year, but only if you have diabetes. Medicare beneficiaries who want coverage for routine vision care, glasses and contact lenses may consider a Medicare Advantage plan that offers vision benefits.
What is Medicare Part B?
Enteral nutrition, such as intravenous and tube feeding. Intravenous Immune Globulin (IVIG) that is provided at home. Transplant and immunosuppressive drugs. Medicare Part B also covers vaccinations and flu shots.
Can Medicare beneficiaries get additional coverage?
How Medicare beneficiaries can get coverage for additional services. Medicare beneficiaries looking for coverage for the above services are not entirely out of luck. There are three Medicare options that may be used for coverage outside of or in addition to Original Medicare benefits. Medicare Advantage (Medicare Part C)
Does Medicare cover everything?
Original Medicare doesn’t cover everything. Learn about your coverage options, including Medicare Advantage plans that may cover additional services you need. Medicare provides coverage for a wide range of services and products, but it doesn’t cover everything. In this guide, we take a look at what is not covered by Original Medicare ...
Does Medicare cover prescription drugs?
Prescription drugs. Original Medicare does not cover most prescription drugs. Only a select few prescription drugs are covered by Original Medicare, and only under limited conditions. Medicare Part B also covers vaccinations and flu shots.
What is considered durable medical equipment?
Durable medical equipment that is not suitable for at-home use such as paraffin bath units used in hospitals or skilled nursing facilities. Most items that are considered as providing convenience or comfort (ex. air conditioners) Items that are thrown away after use or that aren’t used with equipment (ex. catheters)
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is the difference between Medicare Advantage and Original?
The main difference between Original Medicare and Medicare Advantage lies in how you get a durable medical equipment item covered. For example, a Medicare Advantage plan may require prior authorization in order for items to be covered.
What is DME in medical terms?
Medicare defines durable medical equipment, or DME, as reusable medical equipment that has been deemed medically necessary. Your doctor or another health care provider determines what equipment you need per Medicare guidelines. He or she assesses your health condition, what equipment can be used in your home and what equipment you are able to use.
How long does a durable medical equipment item last?
Used because of an illness or injury. Able and necessary to be used at home (though you may also use it outside your home)*. Likely to last for three or more years.
What are some examples of DME?
Some examples of DME are walkers, hospital beds, home oxygen equipment, diabetes self-testing equipment (and supplies), and certain nebulizers and their medications (non-disposable). Wheelchairs and power scooters are also included in the list of DME, but additional rules apply. (See below.)
What is Part B for Medicare?
Original Medicare’s Part B covers durable medical equipment items when your Medicare-enrolled doctor or health care provider prescribes it for you to use at home. Once you have the doctor’s prescription, you can take it to any Medicare-enrolled supplier.
Does Medicare cover exceptions?
This booklet outlines the 4 categories of items and services Medicare doesn’t cover and exceptions (items and services Medicare may cover). This material isn’t an all-inclusive list of items and services Medicare may or may not cover.
Does Medicare cover personal comfort items?
Medicare doesn’t cover personal comfort items because these items don’t meaningfully contribute to treating a patient’s illness or injury or the functioning of a malformed body member. Some examples of personal comfort items include:
Does Medicare cover non-physician services?
Medicare normally excludes coverage for non-physician services to Part A or Part B hospital inpatients unless those services are provided either directly by the hospital/SNF or under an arrangement that the hospital/SNF makes with an outside source.
Does Medicare cover dental care?
Medicare doesn’t cover items and services for the care, treatment, filling, removal, or replacement of teeth or the structures directly supporting the teeth, such as preparing the mouth for dentures, or removing diseased teeth in an infected jaw. The structures directly supporting the teeth are the periodontium, including:
Can you transfer financial liability to a patient?
To transfer potential financial liability to the patient, you must give written notice to a Fee-for-Service Medicare patient before furnishing items or services Medicare usually covers but you don’ t expect them to pay in a specific instance for certain reasons, such as no medical necessity .
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is gap filling in Medicare?
For newly covered items of DMEPOS paid on a fee schedule basis where a Medicare fee does not exist , the Centers for Medicare & Medicaid Services (CMS) uses a process to establish fees called gap-filling. This allows Medicare to establish a price that aligns with the statutory requirements for the DMEPOS fee schedule.
When will Medicare change the KU modifier?
As aforementioned, these system changes will be implemented on July 1, 2020.
What is Medicare Accessibility Act?
CMS is implementing the Patient Access and Medicare Protection Act to ensure that beneficiaries have access to wheelchair accessories and seat and back cushions when furnished with Group 3 complex rehabilitative power wheelchairs. To ensure beneficiary access to these accessories particularly for these vulnerable populations, advance payment may be available for suppliers. Prior to July 1, suppliers will be paid the adjusted fee schedule rates. The average reduction during this period for these items is approximately 10%. During this time, CMS has announced that suppliers are able to submit a single advance payment request for multiple claims if the conditions described in CMS regulations at 42 CFR Section 421.214 are met. Additional information is below.
What is TTFT in Medicare?
TTFT is a system consisting of an electromagnetic field generator and transducer arrays and will be covered under the Medicare Part B benefit for durable medical equipment (DME) for items and services furnished on or after September 1, 2019.
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
When does the Cares Act end?
Section 3712 (a) of the CARES Act extends the current adjusted fee schedule methodology that pays for certain items furnished in rural and non-contiguous non-CBAs based on a 50/50 blend of adjusted and unadjusted fee schedule amounts through December 31, 2020 or through the duration of the PHE, whichever is later.
Does Medicare cover CGMs?
Based on input from patients and other stakeholders, The Centers for Medicare & Medicaid Services (CMS) is announcing important changes in its written policies regarding how Medicare covers continuous glucose monitors (CGMs). These changes are consistent with the Agency’s approach of putting patients first and incentivizing innovation and use of e-technology.
