
What part of Medicare covers hospital stays?
If admitted into a hospital, Medicare Part A will help pay for:
- the hospital room
- nursing services
- meals
- medications
- medical supplies
- durable medical equipment used while in hospital care, like wheelchairs, walkers, and crutches
- diagnostic testing
- rehabilitation services provided while an inpatient
How do Medicare Advantage plans pay for hospital stays?
- Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments.
- Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. ...
- Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. ...
How much will you pay for a hospital stay?
The average hospital stay runs $11,700 with Medicare ($13,600) and “other” insurance ($12,600) paying top dollar and the uninsured ($9,300) and Medicaid ($9,800) paying the least. Those are alarming figures, especially for families with limited budgets or no insurance.
How many days will Medicare pay for rehab?
Medicare pays part of the cost for inpatient rehab services on a sliding time scale. After you meet your deductible, Medicare can pay 100% of the cost for your first 60 days of care, followed by a 30-day period in which you are charged a $341 co-payment for each day of treatment. Longer stays may count against your lifetime reserve days, after which you may be billed for the full cost of care.
Which Medicare covers a patient's hospital stay?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What part of Medicare pays for hospitalization?
Medicare Part A hospital insuranceMedicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Does Medicare cover 100% of hospital costs?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Which part of Medicare covers hospital stays up to 60 days?
Medicare Part AWhat Are Medicare Lifetime Reserve Days? Medicare Part A pays for inpatient hospital care. During each benefit period, Medicare covers up to 90 days of inpatient hospitalization. After 90 days, Medicare gives you 60 additional days of inpatient hospital care to use during your lifetime.
What is the difference between Part C and Part D Medicare?
Medicare Part C and Medicare Part D. Medicare Part D is Medicare's prescription drug coverage that's offered to help with the cost of medication. Medicare Part C (Medicare Advantage) is a health plan option that's similar to one you'd purchase from an employer.
What does Part B of Medicare pay for?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
What is the Medicare deductible for 2021?
The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
What happens when you run out of Medicare days?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
What is the Medicare lifetime maximum?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What is the Medicare two midnight rule?
The Two-Midnight rule, adopted in October 2013 by the Centers for Medicare and Medicaid Services, states that more highly reimbursed inpatient payment is appropriate if care is expected to last at least two midnights; otherwise, observation stays should be used.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
What is covered by Medicare before a hospital stay?
This coverage includes: general nursing care. a semi-private room. hospital equipment and services. meals. medication that is part of inpatient hospital treatment.
How long does Medicare cover hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual’s reserve days. Medicare provides 60 lifetime reserve days. The reserve days provide coverage after 90 days, but coinsurance costs still apply.
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
How much does Medicare pay for skilled nursing in 2020?
Others, who may have long-term cognitive or physical conditions, require ongoing supervision and care. Medicare Part A coverage for care at a skilled nursing facility in 2020 involves: Day 1–20: The patient spends $0 per benefit period after meeting the deductible. Days 21–100: The patient pays $176 per day.
What is Medicare Part A?
Medicare Part A. Out-of-pocket expenses. Length of stay. Eligible facilities. Reducing costs. Summary. Medicare is the federal health insurance program for adults aged 65 and older, as well as for some younger people. Medicare pays for inpatient hospital stays of a certain length. Medicare covers the first 60 days of a hospital stay after ...
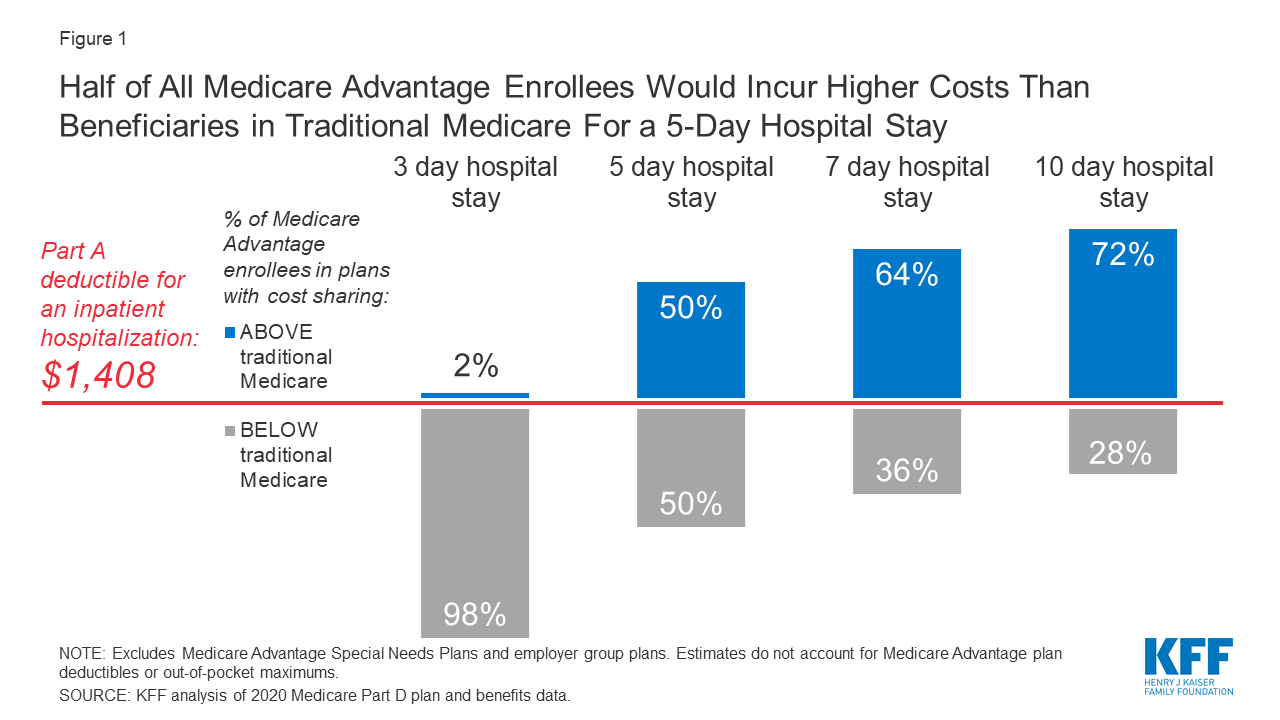
How much is the deductible for Medicare 2020?
This amount changes each year. For 2020, the Medicare Part A deductible is $1,408 for each benefit period.
What is long term acute care?
Long-term acute care hospitals specialize in treating medically complex conditions that may require extended hospital stays, of several weeks , for example. After doctors at a general acute care hospital have stabilized a patient, the patient may be transferred to a long-term care hospital.
When Should You Apply For Medicare Part A
If you wont get Medicare Part A premium-free, try to sign up for it when youre first eligible, as you could face a late enrollment penalty. Your initial enrollment period begins when you become eligible for Medicare. You can also join during the Medicare open enrollment period, which runs annually from October 15 through December 7.
Medicare Nursing Home Coverage
Part A does not pay for nursing home custodial care like bathing, dressing, eating and using the bathroom. But if you need skilled nursing facility care thats medically necessary , Part A may help cover it.2
Skilled Nursing Facility Care
After you are discharged from a hospital stay, you may still need care that you canât give yourself, like an intravenous injection. If thatâs the case, your doctor might order a stay at a skilled nursing facility where a skilled professional can administer your treatment and provide you with the proper medication.
Skilled Nursing Facility Care Costs
The costs for a rehab stay in a skilled nursing facility are as follows:
How Much Medicare Pays For You To Stay In A Hospital
Medicare Part A pays only certain amounts of a hospital bill for any one spell of illness.
Will Medicaid Pay For Long
Many Medicare enrollees are qualify for Medicaid due to their limited incomes and assets. Unlike Medicare, Medicaid covers both nursing home care and Home and Community Based Services .
What Constitutes One Spell Of Illness
A spell of illness, called a “benefit period,” refers to the time you are treated in a hospital or skilled nursing facility, or some combination of the two. The benefit period begins the day you enter the hospital or skilled nursing facility as an inpatient and continues until you have been out for 60 consecutive days.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
When is an inpatient admission appropriate?
An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
Is an outpatient an inpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient. In these cases, you're an outpatient even if you spend the night in the hospital.
Does Medicare cover skilled nursing?
Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're formally admitted to the hospital with a doctor's order. The day before you're discharged is your last inpatient day. You're an outpatient if you're getting ...
How long does a hospital stay in Medicare?
In order to be considered an inpatient stay, a recipient must be admitted for care by a doctor’s orders and that care must last longer than 24 hours.
How much does Medicare pay for inpatient care?
As an inpatient, you will pay 20% of the hospital bill once you have met the deductible for Medicare Part A. Medicare insurance sets the rates for services received as an inpatient in a hospital by diagnostic categories and conditional circumstances of the hospital itself.
What is disproportionate share hospital?
Hospitals that treat a large volume of low-income patients are classified as disproportionate share hospitals (DSH) and qualify for a higher percentage payment than hospitals without this classification. Teaching hospitals and hospitals in rural areas can also receive add-ons that increase the rate Medicare pays them.
Is observation only considered outpatient care?
Some patients may be admitted for observation-only services on an overnight basis, but this is classified as outpatient care rather than inpatient care. In those situations, Medicare Part B payment terms apply, which means recipients are accountable for their Part B deductible and corresponding copayment or coinsurance amounts.
