Medicare star ratings are important because they give you an idea about which plans in your area have the highest satisfaction ratings. Star ratings only pertain to Medicare Advantage and Part D plans. For both types of coverage, the ratings provide a way to compare your plan options beyond their cost.
What is the best Medicare plan?
They are here to talk about their 5 star medicare plans available to switch your current plan or during the election periods throughout the year. As independent agents, Deb and Jerry represent most of the supplement plan and drug -plan carriers and all Medicare advantage plan carriers.
What is Medicare 5 star rating system?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
What is a five star Medicare plan?
5 ... Medicare to let them know that he wanted to keep his original Medicare. According to a Centers for Medicare & Medicaid Services spokesperson, an ACO is not "a Medicare Advantage Plan ...
Why are Medicare star ratings important?
- Staying healthy: access to preventative services to keep members healthy.
- Chronic conditions management: care coordination and frequency of treatment that members received for their long-term/chronic conditions.
- Member experience: overall satisfaction with the plan.

Do Medicare supplement plans have star ratings?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent.
What are Medicare Part D star ratings?
Medicare Part D Star Ratings The Centers for Medicare & Medicaid Services (CMS) creates plan ratings that indicate the quality of Medicare plans on a scale of 1 to 5 stars with 5 stars being the highest rating.
What states have 5 star Medicare Advantage plans?
States where 5-star Medicare Advantage plans are available:Alabama.Arizona.California.Colorado.Florida.Georgia.Hawaii.Idaho.More items...•
Which Medicare Advantage plan has the highest rating?
What Does a Five Star Medicare Advantage Plan Mean? Medicare Advantage plans are rated from 1 to 5 stars, with five stars being an “excellent” rating. This means a five-star plan has the highest overall score for how well it offers members access to healthcare and a positive customer service experience.
What is the best Medicare Part D plan for 2022?
The 5 Best Medicare Part D Providers for 2022Best in Ease of Use: Humana.Best in Broad Information: Blue Cross Blue Shield.Best for Simplicity: Aetna.Best in Number of Medications Covered: Cigna.Best in Education: AARP.
What are the Medicare 5-star measures?
Medicare has many categories, around 37, actually, for measuring the quality and performance a plan must meet before it can receive a 5-Star Rating. Measures include staying healthy programs, managing chronic conditions, member experience and satisfaction, pharmacy services, and customer service.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What's the best state for Medicare?
MinnesotaMedicare plays a central part in healthcare for adults over 65 (nearly 63 million enrolled in 2020). Yet they don't all experience the same quality of care....In this Article.Overall Rank1StateMinnesotaTotal Score66.70Cost20.60Quality22.3150 more columns
When a health plan reaches a star rating of 5 they are able to?
5-Stars is the highest rating However, if a plan gets a 5-star rating, it is considered excellent. This means you'll get a plan that excels at keeping members healthy and has better customer service.
Are there disadvantages to a Medicare Advantage plan?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
What is the difference between AARP Medicare Complete and AARP Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
Why are star ratings important to Medicare Advantage plans?
Medicare star ratings are important because they give you insight into which plans in your area have the highest satisfaction ratings among those on Medicare.
What are CMS Medicare star ratings based on?
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calc...
What does a CMS 5-star rating mean?
A 5-star Medicare plan has earned the best-possible rating for quality and performance. If a 5-star plan is available in your area, you can switch...
What is the highest rating for a Medicare Advantage plan?
A 5-star Medicare Advantage plan has the highest possible rating. Plans are ranked on a scale of 1 star to 5 stars. Only 16% of contracts have achi...
Can you get a $0 Medicare Advantage plan with 5-stars?
Yes, in 92% of the counties where 5-star plans are available, you can get a free Medicare Advantage plan that also has 5 stars. However, the cost o...
Why are star ratings important when choosing a Medicare plan?
Medicare star ratings tell you about a plan's quality and performance across a range of criteria. This can tell you the rate of customer satisfacti...
Top 5-star Medicare Advantage plans
Medicare Advantage plans with five stars are top-tier plans that are considered "excellent" by the Medicare's administering agency, the Centers for Medicare & Medicaid Services (CMS).
5-star special enrollment period
If a 5-star plan is available in your location, you qualify for a 5-star special enrollment period (SEP) that allows you to switch to a 5-star plan at any time during the year.
How Medicare star ratings are calculated
Each Medicare plan's overall star rating is a weighted average of several different data points. This means it's a robust measurement that can help you understand which are the best-performing Medicare plans in your area.
Frequently asked questions
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calculations about the number of complaints, outcomes such as how often those with diabetes fill their prescriptions and more.
Methodology
Data and analysis is based on Centers for Medicare & Medicaid Services (CMS) public use files, fact sheets and technical notes. Medicare Advantage analysis only includes plans that include prescription drug coverage and excludes employer-sponsored plans, special needs plans, PACE plans, sanctioned plans and health care prepayment plans (HCPPs).
Why do hospitals have star ratings?
Star ratings can give you information and help you compare hospitals locally and nationwide, but you should consider a variety of factors when choosing a hospital, like physician guidance about your care plan. Along with the overall rating, you should look at other aspects of hospital quality like rates of infection and complications, and patients' experience of care based on survey results.
What is the overall rating of a hospital?
The overall rating, between 1 and 5 stars, summarizes a variety of measures across 7 areas of quality into a single star rating for each hospital. The 7 measure groups include:
What Medicare Advantage Plans have a 5-star rating?
This is done intentionally to keep competition among plans. Sometimes it’s something as medial as not offering transportation coverage that can drag down their 5-star to a 4.5. Plus, a lot of their fate lies in the hands of their members, who leave reviews each year indicating how well they met all levels of care.
What does higher star rating mean for Medicare?
Plans with higher Medicare star ratings have proven higher quality (which may mean more doctors in-network, better care, or more care options), while lower ratings have not. Knowing what these Medicare star ratings mean and how to utilize them in your search for the best health insurance can be a massive help in deciding which plan is best for you.
What does a 3 star rating mean?
Three stars indicate that beneficiaries can choose from more than one provider within their plan’s healthcare providers network. This includes specialists such as cardiologists and cancer surgeons—even if they’re outside your plan’s local area. You’ll also be able to see pricing information before you sign up for coverage, so you’ll know how much each doctor visit costs ahead of time.
How many stars does Medicare have?
Medicare uses a system that assigns each plan a star rating from one to five stars. Plans with higher ratings offer higher quality, meaning they offer better care at lower costs through well-known providers and hospitals in their network.
What does a star mean in a health plan?
Two stars indicate that beneficiaries can choose from one provider within their plan’s network without cost-sharing or restrictions.
Is a 5 star plan good?
They also offer more favorable customer service hours and higher satisfaction ratings from beneficiaries who have used them in the past year. Although 5- star plans are ideal, this rating is extremely difficult to achieve.
How many stars does Medicare have?
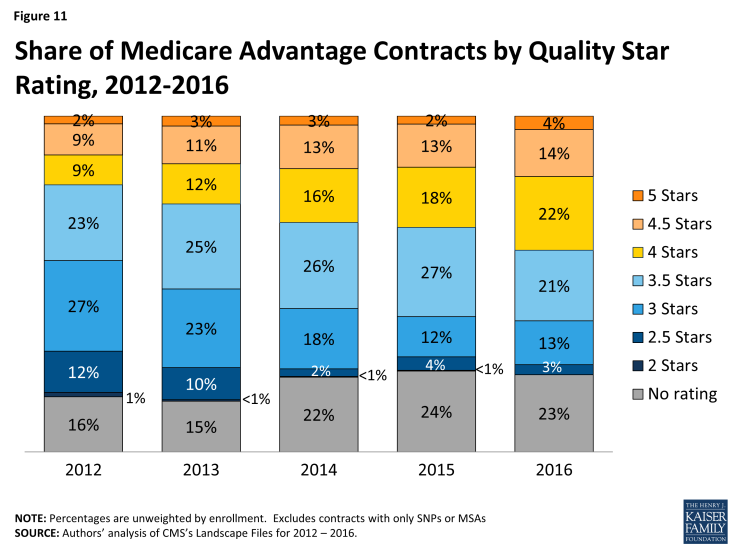
Plans can receive from one star (poor) to five stars (excellent), and the ratings are based on numerous measures, including factors such as customer service, how easy it is for enrollees to receive care, how well the plan does at improving or maintaining members’ physical and mental health, and how quickly the plan handles appeals – among many others. ( See Tables 9, 10, and 11 ).
How many stars will Medicare Advantage receive in 2022?
For 2022, the average Medicare Advantage plan with integrated Part D coverage (MA-PD) received 4.37 stars, up from 4.06 stars in 2021 (average is weighted by enrollment). And the average stand-alone Part D plan received 3.7 stars (up from 3.58 in 2021). CMS reported that approximately 90% of MA-PD enrollees are in plans that have received at least four stars for 2022.
How many Medicare Advantage plans will be available in 2022?
For 2022, there are a total of 87 Medicare contracts nationwide that have a 5-star rating (a significant increase from the 28 Medicare contracts that had 5-star ratings in 2021). Three are Medicare cost plans and 74 are Medicare Advantage plans with integrated Part D coverage. The other ten are stand-alone Part D plans, but they’re only available as employer group plans, and cannot be purchased by individuals (see Table A3 here for details). Of the 87 contracts that received five stars for 2022, there were 60 that had lower ratings in 2021.
Why do some contracts not have star ratings?
Some contracts do not receive star ratings, either because sufficient data are not available, or because the contract is too new.
Is the 2021 Star Ratings based on new data?
So the 2021 star ratings were based on a combination of new and previous data.
Can you collect star ratings remotely?
Due to the pandemic, the federal government had to contend with the fact that a significant amount of the data used for star ratings could not be collected remotely, and that in-person data collection wasn’t feasible.
Will CMS change the rating system for 2022?
CMS noted that although some changes had been made to the rating system for 2022 to account for the COVID pandemic, the sharp increase in the number of contracts with 5-star ratings “also reflects improvements in sponsors’ scores on several measures.”
Why do we need star ratings for Medicare?
Medicare star ratings can help you get a sense of how well a plan performs for its members. While it isn’t the only factor you should take into account when choosing a plan, it can be a helpful.
What is the star rating for Medicare Advantage?
The Medicare star rating is designed as a way to help consumers select a Medicare Advantage plan as well as evaluate how well plans that contract with Medicare perform . Medicare assigns a star rating from 1 to 5, with 5 being the best, for both Medicare Advantage and Medicare Part D (prescription drug coverage) plans.
What is considered in-network coverage for Medicare Advantage?
Coverage. You should also evaluate a health plan based on the coverage it offers. This includes considerations for in-network providers, covered prescription drugs, and additional services you may wish to receive under Medicare Advantage. These may include dental, vision, and hearing coverage.
What factors are considered when determining Medicare rating?
Medicare takes a variety of variables into account when determining the rating, including plan participants’ ratings and member complaints. A person can use the ratings, along with factors such as cost and coverage, to choose the right Medicare Advantage plan. When you’re trying to choose a Medicare Advantage or Part D (prescription drug) plan, ...
What is the symbol for a 5 star plan?
A 5-star plan has a special symbol, which is a yellow triangle with a white star that has the number 5 inside of it. Medicare determines these ratings from multiple data sources. These include: complaint tracking. grievances and appeals tracking.
How many categories does Medicare consider when assigning a star rating to a Medicare Advantage plan?
Medicare considers five categories when assigning a star rating to a Medicare Advantage plan:
Why do Medicare stars come out?
Medicare times the release of its star ratings in time to help you make decisions about your plan for the upcoming year.
How does Medicare's star rating system work?
You could choose from a wide range of Medicare Part C (now known as Medicare Advantage) plans as early as 1997. But you didn't have a good way to compare them until 2008. That's when the Centers for Medicare & Medicaid Services (CMS) first rolled out the star rating system.
What parts of a health insurance plan are rated?
The way that the CMS rates healthcare plans depends on what type of plan it is.
What is the standard rating for a Medicare plan?
Most Medicare plans have a good rating these days, but not all. According to the CMS, nearly 68% of Medicare plans with prescription drug coverage (MA-PDP) in 2022 have a four-star rating or higher. That’s up from 49% in 2021.
How to use the rating system to pick the best health insurance plan
In general, it's best to choose the highest-rated plan that you can afford. You can compare plans and their ratings on the Medicare Plan Finder website. On the Plan Finder tool, each plan has an overall star rating based on all the rated categories.
The bottom line
Choosing between different Medicare plans can be tough. But the star ratings can help you identify high-performing ones and those with higher scores in categories that may matter to you. The CMS rates each plan on up to 40 different factors to create a helpful picture of how well the plan treats its members and their healthcare needs.