What are the changes to Medicare Advantage plans for 2020?
Apr 26, 2019 · On Jan. 1, 2020, newly-eligible Medicare beneficiaries won’t be able to purchase Medicare supplement plans that cover the Part B deductible. This includes Medicare supplement Plans C, F, High-Deductible F. A new Medicare supplement Plan High-Deductible G will be available effective Jan. 1 where offered. This will not affect your Medicare Supplement …
Can I Keep my Medicare plan before January 1 2020?
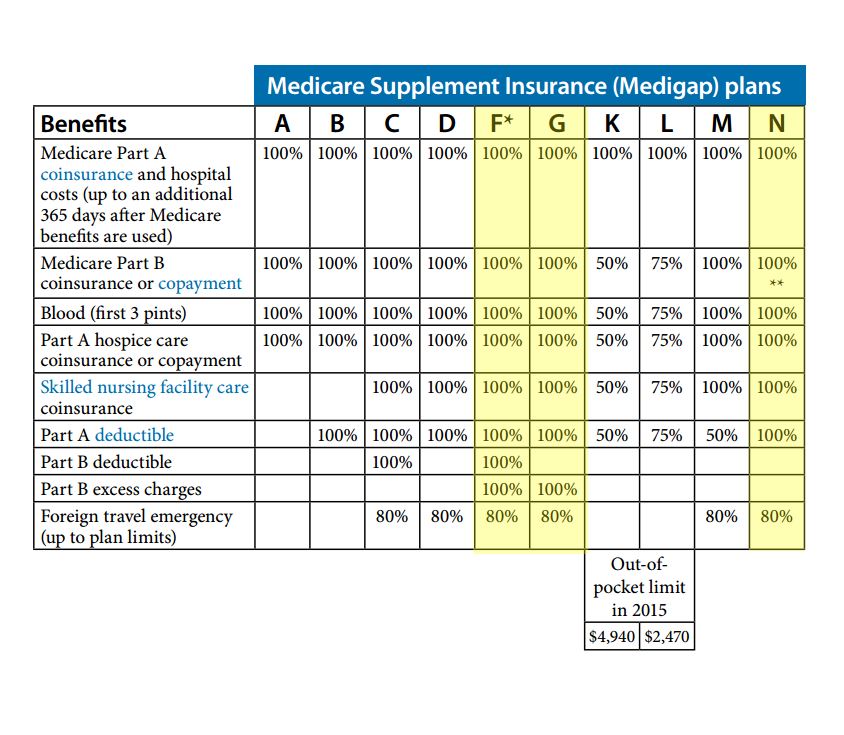
The 2020 Medigap changes will not affect these clients because their coverage falls into “grandfathered” status. New clients eligible for Medicare after December 31, 2019 will not be allowed to enroll in these plans. Instead, they will have two guaranteed issue options: Plan D and G. Plan G will have a high-deductible option beginning in 2020.
What is the cost of Medicare Part B in 2020?
Feb 25, 2022 · To utilize guaranteed issue rights, beneficiaries must abide by MACRA when selecting their plan. At this time, only those who enrolled in Part A before January 1, 2020, can be guaranteed issue to Plan F or Plan C. Like guaranteed issue rights, Open Enrollment Periods allow beneficiaries to enroll in a Medigap plan with no underwriting health questions. Those who …
Are Medigap plans C and F still available in 2020?
Because of this, Plans C and F are no longer available to people new to Medicare on or after January 1, 2020. If you already have either of these 2 plans (or the high deductible version of Plan F) or are covered by one of these plans before January 1, 2020, you can keep your plan.
What states are guaranteed issue for Medicare supplement?
What are the top 3 most popular Medicare supplement plans in 2021?
Is Medicare Part D guaranteed issue?
Is Plan G guaranteed issue in 2020?
What is the least expensive Medicare supplement plan?
What is the most expensive Medicare supplement plan?
Is Plan G guaranteed issue in 2021?
How long is the guaranteed issue period for Medicare Supplement?
Can you be denied a Medicare Supplement plan?
Is Plan G going away?
Why do doctors not like Medicare Advantage plans?
Are Medigap policies guaranteed renewable?
What are the changes to Medicare?
The biggest changes to Medicare in 2020 will be: 1 Slightly higher premiums for Medicare Part A 2 Slightly higher premiums and deductibles for Medicare Part B and the requirement that the Medicare Part B deductible be part of every supplement plan 3 Discontinuation of supplement plans that don’t require payment of the Medicare Part B deductible—meaning Medicare Supplement plans C and F will no longer be options for people enrolling in Medicare in 2020 4 The addition of a higher-deductible Medicare Supplement plan in the form of Medicare Plan G 5 The closing of the Medicare Part D “donut hole” which will allow for a reduction in prescription medication costs for most people
What is the Medicare Part B premium?
The Medicare Part B premium will rise to $1 44.58 and the Medicare Part B deductible will rise to $198 as of 2020. As of 2020, any plan that does not require payment of the Medicare Part B deductible will no longer be allowed to be sold, which is why Medicare Supplement plans C and F are now discontinued.
Will Medicare Supplement Plan C and F be available in 2020?
The biggest Medicare changes of 2020 were to new enrollees. Medicare Supplement Plan C and F will no longer be available for people enrolling in Medicare in 2020. That means people who were enrolled before 2020 will in most cases be allowed to keep coverage, but for people newly turning 65 and enrolling Medicare, the Part C plan won’t be available.
Does Medicare cover prescription drugs?
Medicare Part D covers prescription medications. As far as Medicare changes in 2020, the secondary coverage for Medicare Part D—known as the “Medicare Part D donut hole”—continues to be more closed than it was in previous years.
Is there a new Medicare Supplement Plan?
There’s a new high-deductible Medicare Supplement plan being introduced in 2020. It’s called Medicare Part G, and it’s similar to the previous Medicare Part F plan, except it also covers the Medicare Part B deductible so it’s still legal as of the changes to 2015 law that requires this coverage.
How many people will be enrolled in Medicare Advantage in 2020?
Enrollment in Medicare Advantage has doubled over the past decade. In 2020, nearly four in ten (39%) of all Medicare beneficiaries – 24.1 million people out of 62.0 million Medicare beneficiaries overall – are enrolled in Medicare Advantage plans; this rate has steadily increased over time since the early 2000s.
How many people will be on Medicare in 2020?
In 2020, nearly four in ten (39%) of all Medicare beneficiaries – 24.1 million people out of 62.0 million Medicare beneficiaries overall – are enrolled in Medicare Advantage plans; this rate has steadily increased over time since the early 2000s.
What percentage of Medicare beneficiaries are in Miami-Dade County?
Within states, Medicare Advantage penetration varies widely across counties. For example, in Florida, 71 percent of all beneficiaries living in Miami-Dade County are enrolled in Medicare Advantage plans compared to only 14 percent of beneficiaries living in Monroe County (Key West).
When did CVS buy Aetna?
CVS Health purchased Aetna in 2018 and had the third largest growth in Medicare Advantage enrollment in 2020, increasing by about 396,000 beneficiaries between March 2019 and March 2020.
How much is the deductible for Medicare Advantage 2020?
In contrast, under traditional Medicare, when beneficiaries require an inpatient hospital stay, there is a deductible of $1,408 in 2020 (for one spell of illness) with no copayments until day 60 of an inpatient stay.
How much does Medicare Advantage pay in 2020?
However, 18 percent of beneficiaries in MA-PDs (2.8 million enrollees) pay at least $50 per month, including 6 percent who pay $100 or more per month, in addition to the monthly Part B premium. The MA-PD premium includes both the cost of Medicare-covered Part A and Part B benefits and Part D prescription drug coverage. Among MA-PD enrollees who pay a premium for their plan, the average premium is $63 per month. Altogether, including those who do not pay a premium, the average MA-PD enrollee pays $25 per month in 2020.
Does Medicare Advantage offer supplemental benefits?
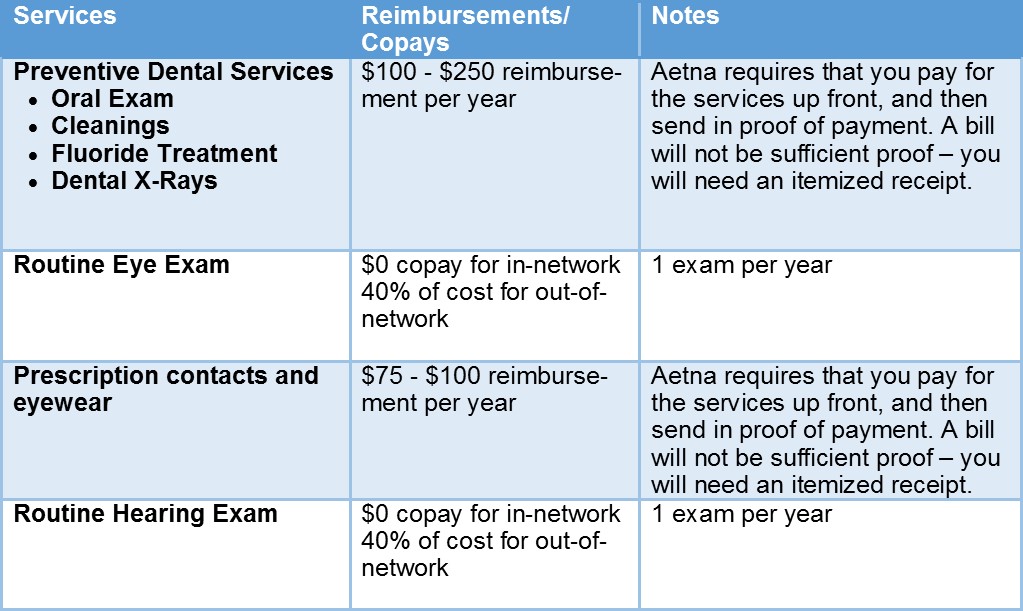
Medicare Advantage plans may provide extra (“supplemental”) benefits that are not offered in traditional Medicare, and can use rebate dollars to help cover the cost of extra benefits. Plans can also charge additional premiums for such benefits. Beginning in 2019, Medicare Advantage plans have been able to offer additional supplemental benefits that were not offered in previous years. These supplemental benefits must still be considered “primarily health related” but CMS expanded this definition, so more items and services are available as supplemental benefits.
Will Medicare change in 2020?
Medicare changes in 2020 will affect what Medigap products you have available to sell, including one of the most popular consumer choices. But with the right preparation, you can organize your portfolio (and your process) to best assist your new and existing clients in the coming year.
Is HealthMarkets insurance licensed?
HealthMarkets Insurance Agency, Inc. is licensed as an insurance agency in all 50 states and the District of Columbia. Not all agents are licensed to sell all products. Service and product availability varies by state.
Is Medicare a federal program?
Even though Medicare is a Federal program, some states have different terms for Open Enrollment, Guaranteed Issue Rights, excess charges, disability, etc. Below, we’ll highlight what states have their own unique rules.
What is guaranteed issue rights?
Guaranteed Issue rights are in place to ensure you can obtain a Medigap policy. Companies must offer you an option, even if you have pre-existing health conditions. For example, Susan lives with COPD, Guarantee Issue rights allow her to get a policy without fear of denial!
How long does it take to change Medigap policy in California?
California – California Medigap rules abide by the birthday rule. The birthday rule in California allows you to change policies within a 60-day window. The birthday rule begins 30 days before your birthday and ends 30 days after.
How long does it take to switch Medigap plans?
Missouri – If you have a Medigap policy, you can switch plans within 60 days of your enrollment anniversary . New York – You can enroll in a Medigap policy without underwriting throughout the year. Washington – Allows Medigap enrollees to change Medigap plans (except for Plan A) at any point.
Does Medigap cover excess charges?
If you’re looking at purchasing a Medigap policy, you may find that some of the plans cover excess charges. When a doctor doesn’t accept Medicare, excess charges may occur; doctors can only charge 15% above the threshold.
What does voluntary group termination mean?
Voluntary group termination means you decide to end your group insurance plan. Sometimes, people pay more for their group insurance than they would pay for Medicare. If this is your current situation, group termination may be beneficial to your pocketbook.
Is Medicare primary or secondary?
If your employer’s health care policy is the primary form of insurance, and Medicare is secondary.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
How long do you have to wait to get a Medigap policy?
The Medigap insurance company may be able to make you wait up to 6 months for coverage of pre-existing conditions. The number of months you've had your current Medigap policy must be subtracted from the time you must wait before your new Medigap policy covers your pre-existing condition.
How long is the free look period for Medigap?
Medigap free-look period. You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period.". The 30- day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
How long do you have to pay for Medigap?
You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period." The 30-day free look period starts when you get your new Medigap policy. You'll need to pay both premiums for one month.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
Does Medicare cover hospitalization?
Medicare Part A covers hospitalization costs. Part A has out-of-pocket costs when enrollees need hospital care, although most enrollees do not pay a premium for Part A. But you’ll have to pay a premium for Part A if you don’t have 40 quarters of work history (or a spouse with 40 quarters of work history).
Is Medicare Advantage available for ESRD?
Under longstanding rules, Medicare Advantage plans have been unavailable to people with end-stage renal disease (ESRD) unless there was an ESRD Special Needs Plan available in their area. But starting in 2021, Medicare Advantage plans are guaranteed issue for all Medicare beneficiaries, including those with ESRD. This is a result of the 21st Century Cures Act, which gives people with ESRD access to any Medicare Advantage plan in their area as of 2021.
How much will Medicare copay be in 2021?
The copay amounts for people who reach the catastrophic coverage level in 2021 will increase slightly, to $3.70 for generics and $9.20 for brand-name drugs. Medicare beneficiaries with Part D coverage (stand-alone or as part of a Medicare Advantage plan) will have access to insulin with a copay of $35/month in 2021.
Is there a donut hole in Medicare?
The Affordable Care Act has closed the donut hole in Medicare Part D. As of 2020, there is no longer a “hole” for brand-name or generic drugs: Enrollees in standard Part D plans pay 25 percent of the cost (after meeting their deductible) until they reach the catastrophic coverage threshold.
How much is the Part A deductible for 2021?
If the person needs additional inpatient coverage during that same benefit period, there’s a daily coinsurance charge. For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020).
